Concept About Anticoagulants – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination setup according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Concept About Anticoagulants
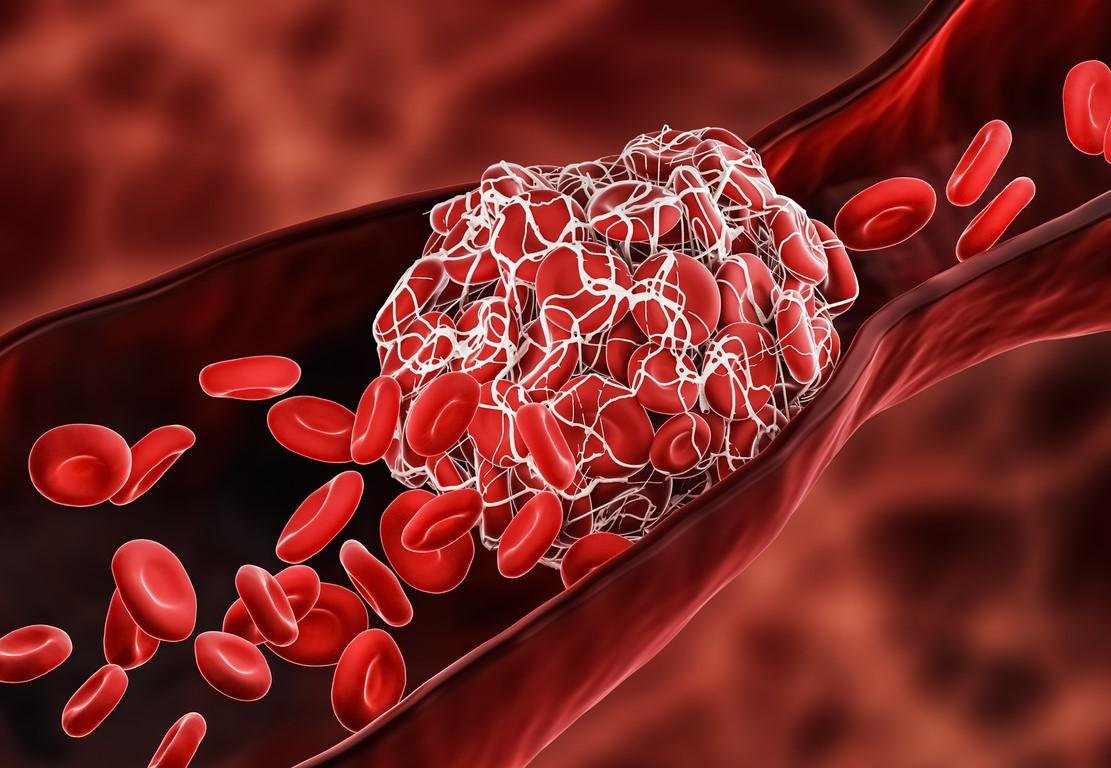
Anti-coagulants are the drugs, which are used to prevent unwanted coagulation.
Classification of anticoagulants:
A. Anticoagulant acting in vitro:
First group:
- Na and K salts of oxalate, citrate and fluoride
- EDTA (ethylene diamine retra acetic acid)
Second group:
- Heparin
- Dextran sulphate
B. Anticoagulant acting in vivo:
- Coumarin derivatives:
- Dicoumarol
- Warfarin
- Cyclocoumerol
- Ascencoumerol
Indandione derivalives:
- Phenindione
- Diphenadione
- Anisidione
C. Anticoagulant acting both in vivo and vitro:
- Heparin
- Dextran sulphate
- Ancord
D. According to mechanism of action
Directly acting:
- Heparin
- Dextran sulphate
Indirectly acting:
- Coumarin derivatives
- Indandione derivatives
E) According to route of administration Injectable anti-coagulants:
- Heparin
- Ancord Oral anticoagulants:
- Warfarin
- Dicoumarol
Name of natural anticoagulants
- Anti-thrombin III
- Heparin (basophils)
- Protein C
- Heparan sulphate
- a2 macroglobulin
- al anti-trypsin
- al anti-plasmin.
Mechanism of anti-coagulants action
Different anticoagulants act by different mechanism. These are:
- Oral anticoagulant drugs inhibit the hepatic synthesis of several clotting factors.
- Injectable anticoagulants (heparin) inhibit the activity of several of these activated clotting factors.
- The endogenous anticoagulants protein C and S downregulate the amplification of blood clotting by proteolysis of factors Va. VIlla, and Xla.
Indication of anticoagulant therapy
- Establish venous thromboembolism.
- Secondary prophylaxis of venous thrombosis & pulmonary embolism.
- Prosthetic heart value.
- Rheumatoid mitral valvular disease.
- Myocardial infraction (atrial fibrillation).
Contraindication of anticoagulant therapy
- Haematological: Pre-existing bleeding disorder.
- Neurological: stroke within 3 weeks, or surgery to brain, eye.
- CVS: Severe uncontrolled hypertension.
- Kidney: Renal failure.
- Alimentary: active peptic ulcer, IBS, oesophageal varices.
- Liver: Cirrhosis.
- Pregnancy (warfarin).
Common adverse effects of anticoagulant therapy
- Haemorrhage (by both oral and injectable anticoagulant)
- Osteoporesis (heparin)
- Hypersensitivity (heparin)
- Urticaria
- Dermatitis
- Anaphylaxis
- Teratogenicity (warfarin, heparin is preferred in pregnancy)
- Alopecia (heparin)
- Necrosis of skin (warfarin)
- Thrombocytopenia (heparin)
Oral Anticoagulants
Oral anticoagulants are:
- Warfarin
- Dicoumarol
- Phenindione
➤ Oral anticoagulants are indirectly acting anticoagulants.
➤ Indicated when prolong anticoagulant therapy is needed.
➤ Delayed onset of action and take about 72 hours to become full active,
➤ Advantage over heparin: it can be given orally.
➤ Therapy with oral anticoagulant should be monitored by prothrombin time.
➤ Antidote of oral anticoagulants: vitamin K.
Dicoumarol
Oral anticoagulants are antagonists of vitamin K; thereby they show their anticoagulant effects by clotting the synthesis of vitamin K dependent clotting factors (II, VII, IX, X). Hence they are called indirectly acting anticoagulants.
- Upon oral administration their bioavailability is nearly complete (11%)
- Oral anticoagulants are highly plasma protein bound.ear) aile
- Biotransformation occurs in liver & kidneys (metabolites are inactive).
- Onset of action of oral anticoagulants are delayed.
- They can cross the placenta; therefore cause birth defect.
- Bleeding is the major toxicity of oral anticoagulant drugs
Mechanism of action of Dicoumarol:
- Dicoumerol has structural similarity with vitamin K. So, it competitively interferes with vitamin-K cycle by blocking the enzyme vitamin-K epoxide reductase which reduces vitamin-K epoxide to vitamin-K in liver.
- Dicoumerol also blocks the vitamin-K dependent carboxylation of glutamic acid residues of factor II,VII, IX and X. So, inhibition of activation of these factor prevent the coagulation.
- Thus, it indirectly inhibits the synthesis of vitamin K dependent clotting factors.
Pharmacological action of oral anticoagulants
Route of administration: oral, iv, im, rectal. Absorption: Readily absorbed from the GIT
Distribution: Small, highly plasma protein bound (99% with albumin)
Bioavailability: 100%
Onset of action: 36-48 hours of ingestion (delayed onset) Duration of action: 20-40 hours (35 hours average) Plasma half-life: 2-6 days
Metabolism: Liver (by microsomal enzyme)
Excretion: Urine, bile
✔ Dicoumerol can cross placental barrier (teratogenicity)
✔Appears in milk (danger to newborn)
✔ Therapy is complicated.
Highly protein bound drugs
- Oral anticoagulants
- Cardiac glycoside (Digitoxin)
- Antiepileptic (phenytoin)
- Oral hypoglycemic drugs (sulfonylurease)
Indication of oral anticoagulant (Dicoumarol)
- Prophylaxis and treatment of venous thrombosis and pulmonary embolism.
- Acute myocardial infarction.
- Arterial embolism in patient with atrial fibrillation, mitral stenosis, etc.
- Angina pectoris, frost bite.
- Acute gangrene.
- Dilated cardiomyopathy.
- Prosthetic cardiac valve
Adverse effects of oral anticoagulant (Dicoumarol):
- Haemorrhage: (antidote: vitamin k)
- Transient purpura
- Warfarin necrosis on skin (mainly in female)
- Teratogenicity
- Liver damage (more)
- Urticaria, alopecia
- Purple toe syndrome
- Congenital bony abnormality in foetus (if given in pregnancy).
- Overdose causes: Haemorrhage, pulpura, nausea, headache. vomiting and diarrhoea.
Contraindications of oral anticoagulant (Dicoumarol):
- Recent trauma, injury (head injury)
- Active internal bleeding, e.g. peptic ulceration.
- Severe hypertension.
- Non-thromboembolic strokes
- Major surgery (brain, spinal cord, eye)
- Pre-existing haemostatic defects.
- First and last two months of pregnancy
- Lactating mother
- Threatened abortion
- Severe liver and renal disease
Choice of anticoagulant:
- For brief and immediate action: Heparin (i/v)
- For prolonged period: Oral anticoagulant (Dicoumerol)
Antidote of Dicoumerol:
- Immediate antagonism: By plasma concentrated with vitamin x dependent clotting factor (factor II, VII, IX, X).
- Delayed antagonism: by inj vitamin K (/v)
Monitoring of oral anti-coagulant therapy:
Therapy with oral anticoagulants is monitored by the patient’s prothrombin time. The results are reported as the international normalized ratio (INR). The INR is the prothrombin time ratio (test/control) obtained if the more sensitive international reference thromboplastin is used. Normal INR = 1. In oral anticoagulant therapy INR should times of normal for effective anticoagulant effect. In anticoagulant raised to 2.5 0 3.5
INR 2.5: Dose of warfarin should be increased. INR > 3.5: Stop the therapy (chance of haemorhage) In summary dosage is usually adjusted to give an INR of 2.5-3.5 Precaution for using oral anticoagulants
- Perform a coagulation screen & platelet count before starling treatment to exclude a pre-existing haemostatic defects. .
- More frequent prothrombin time testing should be carried out to monitor efficacy and compliance.