Concept about Epilepsy – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric- nursing.
Pediatric-nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric-nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Concept about Epilepsy

Epilepsy is a neurological condition (affecting the brain and nervous system) where a person has a tendency to have seizures that start in the brain.
The brain is made up of millions of nerve cells that use electrical signals to control the body’s functions, senses and thoughts. If the signals are disrupted, the person may have an epileptic seizure (sometimes called a ‘fit’ or ‘attack’).
Not all seizures are epileptic. Other conditions that can look like epilepsy include fainting (syncope) due to a drop in blood pressure, and febrile convulsions due to a sudden rise in body temperature when a young child is ill. These are not epileptic seizures because they are not caused by disrupted brain activity.
Definition of Epilepsy:
Epilepsy is recurrent, episodic, paroxysmal transient disturbances of brain function due to abnormal electrical activity of the neurons.
(Ref: Paediatric Nursing, Parul Datta/4/344)
Or.
Epilepsy is recurrent seizure for which there is no immediate precipitating cause.
(Ref: IAP Text Book of Pediatrics/5/339)
Classification of Epilepsy:
A. Generalized Seizures
a) Tonic-clonic seizures (Grand mal)
b) Absence seizures:
- Typical (petit mal)
- Atypical
e) Atopic seizures (drop attacks)
d) Myoclonic seizures.
B. Partial Seizures
a) Simple partial seizures (with elementary symptoms and no impaired consciousness)
- With motor signs (Jacksonians or focal motor).
- With somatosensory or special sensory i.e. visual or auditory.
- With autonomic manifestations (abdominal epilepsy)
b) Complex partial seizures-Manifested with impaired consciousness and with automatism. It includes psychomotor or temporal lobe seizures.
(Ref: Paediatric Nursing, Parul Datta/4/344)
Epileptic syndrome;
Epileptic syndrome is a syndrome where epilepsy is a prominent feature.
(Ref: IAP Text Book of Pediatrics/5th/339)
Causes of Epilepsy;
- Sequelae of any of the acute causes of seizures
- Cerebral malformations
- Metabolic diseases
- Degenerative brain diseases
- Neoplasms
- Genetic disorders
Clinical Features of Epilepsy:
A. In an aura phase:
- A peculiar sensation with dizziness occurs in about one-third epileptic children before tonic-clonic seizure.
- It is a transitory premonitory symptom which the child may recognize as the impending convulsions and adopt measures for self-protection.
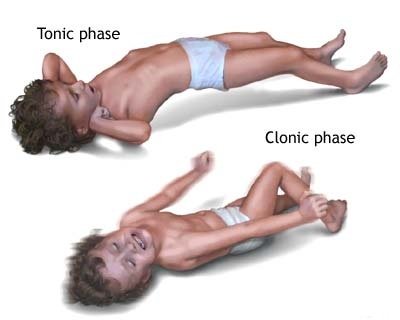
B. In tonic spasm phase:
- Entire body becomes stiff
- Face may become pale and distorted,
- Eyes fixed in one position,
- Back may be arched.
- Head turned to backward or in one side,
- Arms are usually flexed and hands are clenched.
- The child usually falls on the ground from standing or sitting position and may utter a peculiar piercing cry.
- The child loses consciousness and having frothy discharge from mouth due to inability to swallow the saliva.
- Due to spasm of respiratory muscles, there is ineffective breathing and cyanosis.
- Pulse may become weak and irregular.
C. In clonic phase:
- Rhythmic jerky movements due to alternating contractions of muscle groups following the tonic state.
- Usually start in one part and become generalized including the facial muscles.
- The child may pass stool and urine involuntarily and may have tongue or chick bite due to sudden forceful contraction of abdominal muscles and jaw.
D. In the postictal or post-convulsive state:
- The child is usually become sleepy
- Confused or exhausted or perform automatic actions and may complain headache.
(Ref: Paediatric Nursing, Parul Datta/4th/344)
Clinical Features of Absence Seizure:
Absence seizures rarely appears before 5 years of age. It is manifested as the followings: .
- The child may loss contact with the environment for a few seconds.
- The child may appear as staring or day dreaming.
- The child may discontinue the activity suddenly (eg, reading, writing) and may resume the same activity when the seizure is over.
- Atypical absence seizure may present as rolling of the eyes, nodding of the head, slight hand movements and smacking of lips.
(Ref: Paediatric Nursing, Parul Datta/34/372)
Stages of Epilepsy:
1. Aura: A tonic clonic seizure may be preceded by a partial seizure the ‘aura’.
2. Tonic phase: The patient then goes rigid and becomes unconscious, falling down heavily if standing and often sustaining injury. During this phase, respiration is arrested and central cyanosis may be witnessed.
3. Clonic phase: After a few moments, the rigidity is periodically relaxed, producing clonic jerks. During the attack, urinary incontinence may occur, as may tongue biting. A severely bitten, bleeding tongue after an attack of loss of consciousness is pathognomonic of a generalized seizure.
4. Postictal phase: The patient then gradually regains consciousness, but is in a confused and disorientated state for half an hour or more after regaining consciousness. Full memory function may not be recovered for softie hours. After a generalized seizure the patient usually feels terrible, may have a headache and will want to sleep.
Management of Epilepsy/Convulsive Disorders
Management of convulsive disorder depends upon the identified cause. The management is mainly done with drug therapy, diet therapy and surgery, if indicated. Emotional support, psychosocial rehabilitation and vocational guidance are also important aspects of management. Long-term management may continue over one to four years and needs supervision and explanation for treatment compliance.
Drug Therapy
The selection of antiepileptic drugs depends upon age, type of seizure and economical status The commonly used drugs are:
➤Phenobarbital: 3 to 5 mg/kg/day in 1 or 2 divided doses and indicated in tonic-clonic. partial, akinetic and febrile convulsions.
➤ Diphenylhydantoin: 5 to 8 mg/kg/day in 2 divided doses, indicated in tonic-clonic, atonic, akinetic and partial seizures.
➤ Carbamazepine: 10 to 20 mg/kg/day in 2 to 3 divided doses and indicated in tonic- clonic, atonic, akinetic and partial seizures.
➤ Diazepam: 0.2 mg/kg/dose IV or per rectal is indicated in status epilepticus.
➤Sodium valproate: 15 to 20 mg/kg/day in 3 to 4 divided doses is indicated as broad spectrum anticonvulsive agent.
➤ Ethosuximide: 10 to 20 mg/kg/day in 2 divided doses are indicated in absence seizure.
Usually single drug is used but if fails to relieve seizures than addition of a second drug is needed. Duration of treatment may vary, usually 2 to 4 years, but mentally retarded children may need longer duration. Side effects of the drugs should be observed and special precautions to be followed during administration and thereafter.
Success of treatment depends upon regularity in taking drugs. Duration will be decided and must be informed to the parent or caregiver.
Diet Therapy
➤ Ketogenic diet may be given to raise the seizure threshold with calculated amount of proteins and fats without carbohydrates. This diet makes the child ketotic as fat is used for energy production rather than carbohydrate. It seems that ketones may inhibit the seizure.
➤The child should not be given IV fluid with dextrose and strict fluid restriction to be maintained.
Surgical Management
Neurosurgery is indicated in some cases of convulsive disorders, especially in anatomical lesions like brain tumor, hematoma and in medically intractable seizure disorders.
The possible surgical interventions include corpus callosumotomy, focal resection of parts of cerebral cortex such as temporal lobe, extratemporal regions involved as epileptogenic foci.
(Ref: Paediatric Nursing, Parul Datta/4th/346)
Nursing Management of an Epileptic Child:
Nursing assessment:
Detailed subjective and objective data to be collected to formulate nursing diagnosis and to plan nursing interventions.
Nursing diagnoses: The important nursing diagnoses include the followings:
- Risk for injury related to convulsive episodes.
- Ineffective breathing related to spasms of respiratory muscles.
- Social isolations related to misconceptions.
- Altered self-esteem related to lack of control over seizures.
- Knowledge deficit related to long-term care of seizure disorder.
Nursing interventions
➤Ensuring safety during seizures:
Provide preventive measures to protect the child from injury by removal of hard objects, sharp things or toys from the child and placing child on floor or bed.
- Side rails of the bed or crib to be padded.
- Removing oropharyngeal secretions by suctioning and turning head to one side (if possible). Suction machine to be kept ready beforehand.
- Oxygen therapy to be given and all emergency equipment to be kept ready to manage cardiorespiratory problems.
- Close observation and frequent monitoring of child’s condition for vital signs, airway, breathing patterns, pre-seizure events, presence of aura, types of movements during seizures, sites of contractions or twitching, eye movements, pupil size, bladder incontinence, pallor/cyanosis/flushing, teeth clenched, tongue bite, frothy discharge/vomitus aspirations, level of consciousness, neurological status and postictal events (memory, paralysis, speech alteration, restlessness, behavior change), etc.
- Administering prescribed medications, IV/IM or per rectal or oral, as indicated.
- Following special instructions about diet, rest and activities.
Preventing respiratory arrest and aspiration:
- Loosen the clothing around neck and placing the child flat.
- Avoid restraining the child and not to give anything in between teeth or in the mouth, when the teeth are
- clenched during convulsions.
- Clear airway, remove secretions, turn head to one side during seizures and on side lying position in postictal stage.
- Record the events in details.
➤ Promoting socialization: Instructing the par parent to allow the child to perform normal life as possible with some restricted activities like, not to climb high places, or to avoid swimming and exertional activities. An identity card should be kept with the child.
➤ Strengthening self-esteem: Explanation, reassurance, encouraging to discuss about feeling, promoting independence in self-care and family counseling are important for child and parents to improve their self-esteem.
➤ Providing health teaching: Necessary related health teaching to be given with special emphasis on continuation of medications, care during convulsions, diet therapy, restricted activities, misconception regarding the disease and follow-up.
(Ref: Paediatric Nursing, Parul Datta/4/346)
Diet Therapy for Epileptic Patient:
1. Ketogenic diet may be given to raise the seizure threshold with calculated amount of proteins and fats without carbohydrates.
2. This diet makes the child ketotic as fat is used for energy production rather than carbohydrate. It seems that ketones may inhibit the seizure.
3. The child should not be given IV fluid with dextrose and strict fluid restriction to be maintained.
(Ref: Paediatric Nursing, Parul Datta/34/373)