Concept about Nutritional Anaemia – This book covers the entire syllabus of “Nutrition and Dietetics” prescribed by BNMC-for all Diploma in Nursing Science and Midwifery students. We tried to accommodate latest information and topics.
This book is examination friendly setup according to the teachers’ lectures and examination’s questions. At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourished. The unique way of presentation may make your reading of the book a pleasurable experience.
Concept about Nutritional Anaemia
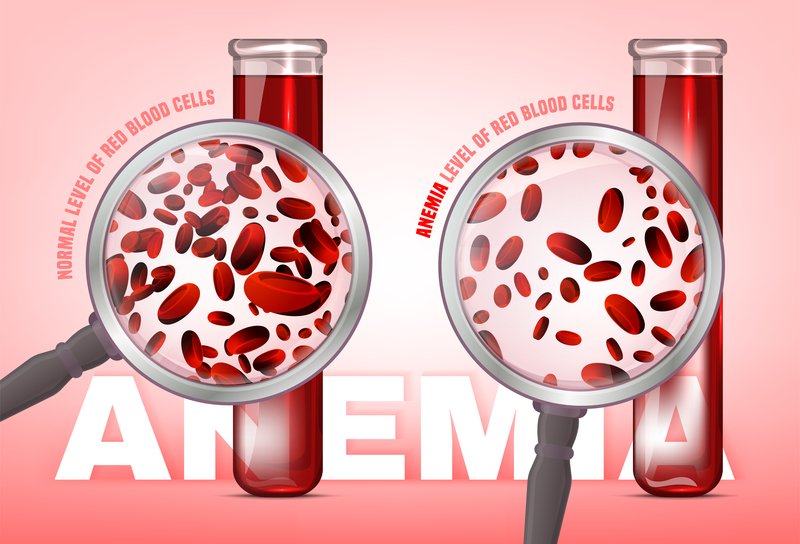
Definition of Anaemia:
It is a clinical condition characterized by the pale colouration of the skin & mucous membrane due to decrease concentration of Hb in the peripheral blood below the normal range for the age & sex of the person.
or
Anaemia is a clinical condition characterized by pale coloration of the skin and mucous membrane due to qualitative and quantitative deficiency of haemoglobin below the lower limit in the peripheral blood in respect of age and sex.
or
Anaemia refers to a state in which the level of haemoglobin in the blood is below the normal range appropriate for age and sex.
Definition of Nutritional Anemia
Nutritional anemia refers to types of anemia that can be directly attributed to nutritional disorders. Examples include Iron deficiency anemia and pernicious anemia
Or
Nutritional anemia in general is defined as a condition that results in a lowering of hemoglobin (Hb) levels below what is considered to be normal for specific demographic groups regardless of the underlying nutritional deficiencies that may be the cause.

Normal Hb level:
- Male: 13-18 gm/dl
- Female: 11.5-16.5gm/dl
- Children: 16-19 gm/dl
- At birth: 18-20 gm/dl
Site Where Anaemia is seen:
- Lower palpebral conjunctiva
- Dorsum of the tongue
- Buccal mucous membrane
- Palm of the hand
- Nail bed
- Sole of the feet
- Whole skin
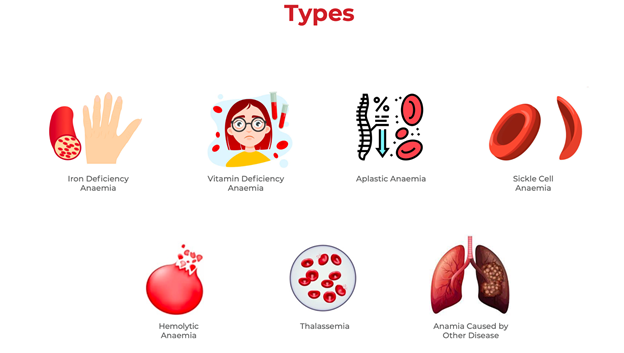
Classifications of Anaemia:
A. Morphological classification: (On the basis of absolute values – MCV, MCH, MCHC)
a) Microcytic hypochromic anaemia: (MCV, MCH & MCHC)
- Iron deficiency anaemia.
- Thalassaemias.
- Sideroblastic anaemia.
- Anaemia of chronic disease.
b) Normocvtic normochromic anaemia: (MCV, MCH & MCHC normal, but RBC & Hb)
- Aplastic anaemia.
- Haemolytic anaemia.
- Acute haemorrhagic anaemia.
c) Macrocytic anaemia: (MCV, MCHC normal)
- Megaloblasic anemia due to vtamin B12 deficiency.
- Megaloblastic anaemia due to folic acid deficiency.
B. Aetiological classification:
a) Haemorrhagic anaemia:
- Acute haemorrhage: Trauma, surgical operation.
- Chronic haemorrhage
✓GIT lesion: PUD, hookworm infestation, haemorrhoids etc.
✓ Gynaecological disturbance: Menorrhagia
b) Haemolytic anaemia: (Due to excess RBC destruction)
- Intra-corpuscular defect: Thalassaemia
- Extra-corpuscular defect: Haemolytic disease of newborn.
c) Dyshaemopoietic anaemia:
- Due- to deficiency of essential elements of erythropoiesis:
✓ Iron deficiency anaemia.
✓ Megaloblastic anaemia (due to deficiency of vitamin B12 & folic acid.
✓ Nutritional anaemia in PEM (protein-energy malnutrition).
✓ Anaemia with scurvy (due to deficiency of vitamin C). - Due to bone marrow disturbance:
✓ Aplastic anaemia.
✓ Sideroblastic anaemia.
✓ Anaemia with renal failure (due to reduced erythropoietin secretion).
✓ Anaemia with endocrine disorders.
C. Clinical classification:
a) Mild anaemia: When Hb = 12 to 9 gm /dl. (‘+’)
b) Moderate anaemia: When Hb = 9 to 6 gm/dl. (++)
c) Severe anaemia: When Hb = Less than 6 gm/dl. (+++)
Causes of Anemia in Bangladesh
- Blood loss anaemia:
✓ Haemorrhoids.
✓ Anal fissure.
✓ Bleeding peptic ulcer disease.
✓ Carcinoma of stomach, colon etc.
✓ Menorrhagia
✓ Hook worm infestation. - Nutritional deficiency: Lack of iron and folate in diet, mal-absorption.
- Frequent pregnancy.
- Chronic kidney disease (CKD).
- Haematological malignancy.
- Aplastic anaemia.
- Congenital haemolytic anaemia.
- Anaemia of chronic disease.
Common Nutritional Anaemia:
- Iron deficiency anaemia.
- Folic acid deficiency anaemia. (Megaloblastic anaemia).
- Vitamin B12 deficiency anaemia. (Megaloblasic anaemia).
C/F of Anaemia:
A. Symptoms of Anaemia
- Fatigue.
- Tiredness.
- Effort intolerance.
- Effort dyspnoea.
- Palpitations.
- Headaches.
- Faintness.
- Giddiness.
- Pounding in the ear.
- Effort angina.
- Symptoms of the cause.
B. Signs of Anaemia
- Pallor.
- Tachycardia.
- Koilonychia: Iron Deficiency Anaemia.
- Jaundice: Haemolytic Anaemia.
- Haemolytic facies: Haemolytic Anaemia,
- Bleeding manifestation: Aplastic Anaemia, anaemia due to bone marrow infiltration such as leukaemia.
- Temperature: Aplastic Anaemia, Anaemia due to bone marrow infiltration such as leukaemia,
- Lymphadenopathy: Anaemia due to leukaemia, lymphoma etc
- Systolic flow murmur.
- High cardiac output state.
- Features of congestive cardiac failure.
- Leg ulcer: sickle cell anaemia.
- Rarely papilloedema.

Prevention/Intervention of Anaemia:
An estimation of haemoglobin should be done to assess the degree of anaemia. If the anemia is severe (Hb 10 gm/dl), high dose of iron or blood transfusion may be necessary. If Hb between 10 to 12 gm/dl, the other interventions are –
Iron and folic acid supplementation:
➤ Mothers: 1 tab of iron & folic containing 60 mg of elemental iron (180 mg of ferrous sulfate) 0.5 mg of folic acid should be given daily up to 2-3 months.
➤ Children: 1 tab of iron and folic acid containing 20 mg of elemental iron (60 mg of ferrous sulfate) & 0.1 mg of folic acid should be given daily.
Iron fortification: Iron fortification with salt by adding ferric ortho-phosphate or ferrous sulfate with Na bisulfate. Iron fortification has many advantages over implementation a salt is a universally consumed dietary item.
Other strategies: (Long term measures)
- Changing dietary habits
- Control of parasites
- Nutrition education.
Detrimental Effects of Nutritional Anaemia:
The detrimental effects of anaemia can be seen in 3 important areas:
1. Pregnancy: Anaemia increases the risk of maternal and foetal mortality and morbidity. Conditions such as abortions, premature births, post-partum haemorrhage and low birth weight were especially associated with low haemoglobin levels in pregnancy.
2. Infection: Anaemia can be caused or aggravated by parasitic diseases, e.g., malaria, intestinal parasites. Further, iron deficiency may impair cellular responses and immune functions and increase susceptibility to infection.
3. Work capacity: Anaemia (even when mild) causes a significant impairment of maximal work capacity.
Risk of Nutritional Anaemia:
Some groups of people are more likely to be iron or folate deficient than others. They are ‘at risk’ of anaemia.
High-risk groups are:
- Women, especially during pregnancy or soon after delivery,
- Babies who are low birth weight or not breastfed,
- Young children- especially if they are malnourished, Adolescents, who are growing fast, especially girls,
- Older men and women, especially if they are poor.
Consequences of Anaemia:
| All individuals: |
|
Infant, pre-school and school children: |
|
Pregnant women and their fetuses: |
|
In summary consequences of anaemia: |
|
Benefits of Anaemia Prevention and Control:
All individuals:
- Increased immunity and low morbidity from infectious diseases.
- Improved cognition.
- Improved quality of life.
In-case of pregnant women (PW) and foetus:
- Decreased risk of complications during delivery, preterm delivery, LBW, maternal and neonatal death.
- Increased iron stores in infants and lower risk of anaemia in infancy and children.
In case of infants and children:
- Improved growth.
- Improved BCD.
- Risk of IDD.
- Improved child survival.
- Better iron store for future pregnancies (adolescent).