Concept about Osteoarthritis – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
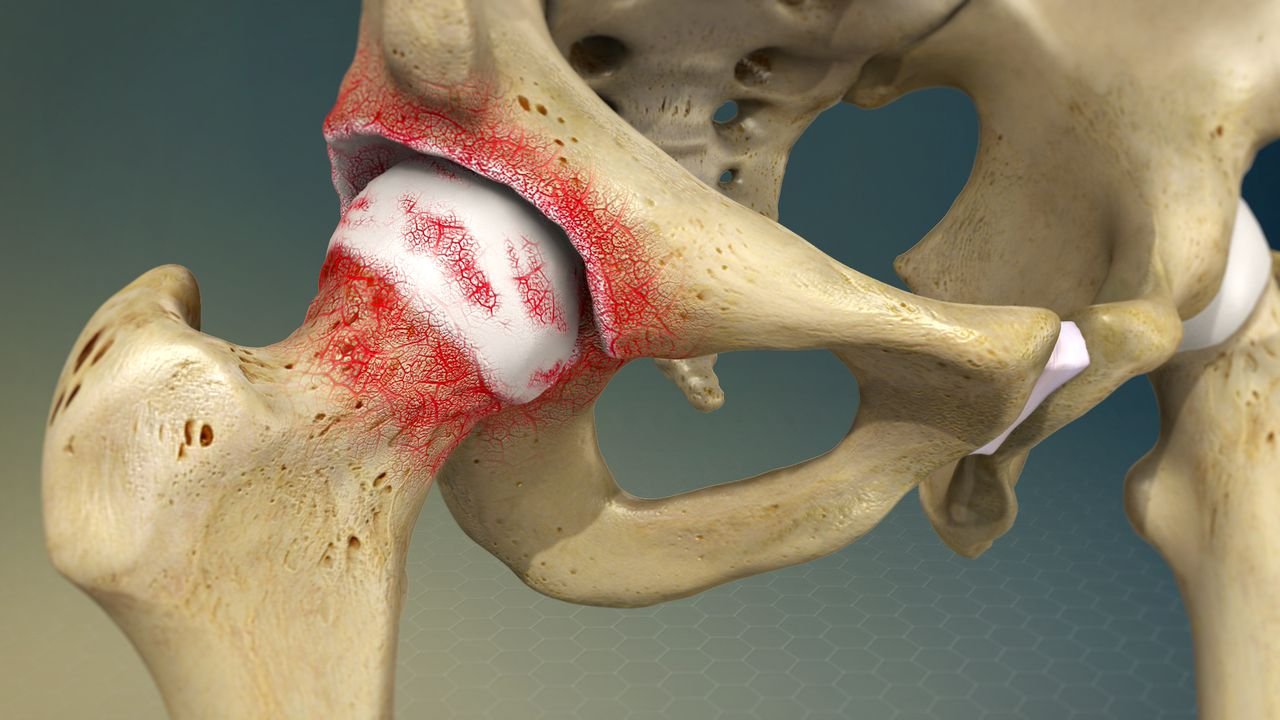
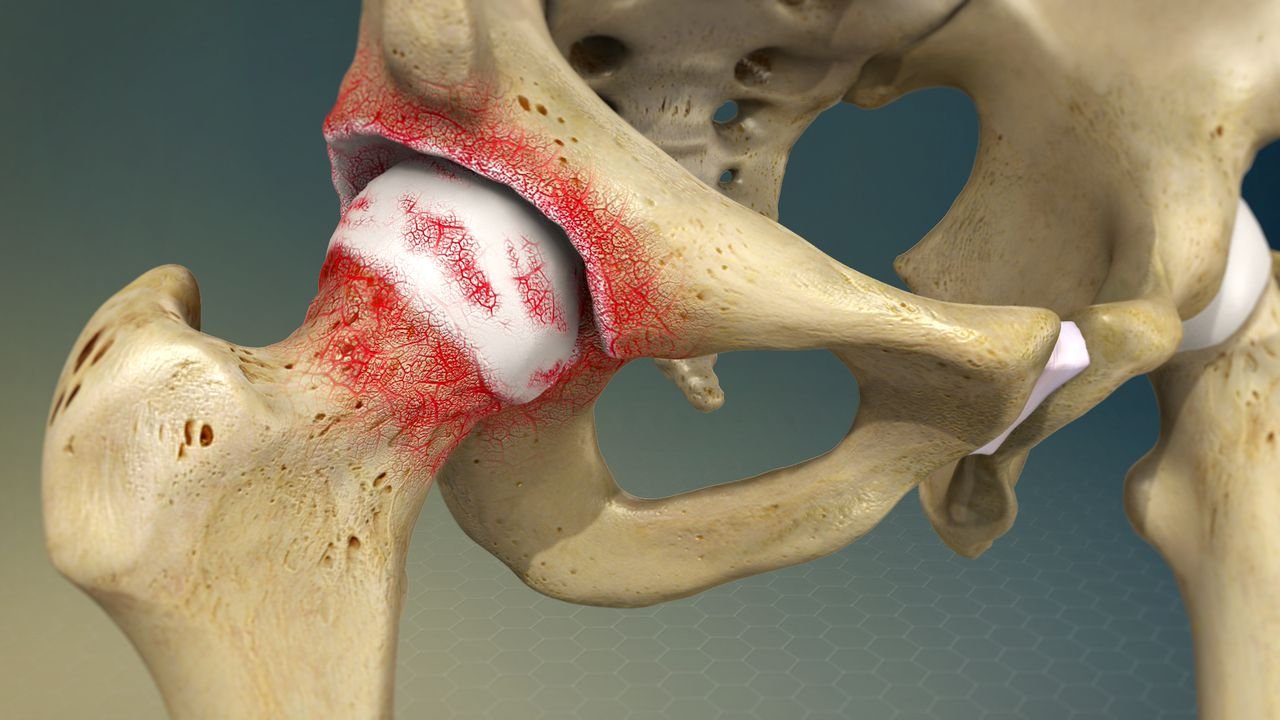
Concept about Osteoarthritis
Osteoarthritis (also known as osteoarthrosis, degenerative arthritis, and hypertrophic) is an idiopathic, slowly progressive, non inflammatory disease of diarthrodial(synovial-lined) joints, characterized by deterioration and erosion of articular cartilage and the formation of new bone, or spurs, at the articular margins.
[Ref-Lippincot Adult orthopedic nursing, page-55]
Or
Osteoarthritis is defined as a degenerative, non-inflammatory joint disease characterized by destruction of articular cartilage and formation of new bone at the joint surfaces and margins.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page 674]
Or
It is defined as a condition of synovial joints characterized by focal loss of articular hyaline cartilage with proliferation of new bone and remodeling of joint contour.
[Ref-Davidson’s “Principles & Practice of Medicine” 21″ edition page-1083]
Or
Osteoarthritis (OA) is a chronic disorder of synovial joints in which the progressive softening and disintegration of articular cartilage accompanied by new growth of cartilage and bone at the joint margins (osteophytes), cyst formation sclerosis in the sub-chondral bone, mild synovitis and capsular fibrosis.
[Ref-Apley’s “System of Orthopaedics and Fractures” 9 edition p-87]
Or
Osteoarthritis is a non-inflammatory condition that is characterized by progressive damage and loss of the articular cartilage. The progressive nature of the process is the result of the body’s innate inability to regenerate hyaline cartilage.
[Ref-Bailey & Love’s short practice of surgery 25th edition page-87]
Causes of osteoarthritis:
A. Primary osteoarthritis:
1. Cause unknown, termed idiopathic.
2. Femoracetabular impingement implicated as a possible cause.
B. Secondary osteoarthritis:
causes due to-
a) Pre-existing jointdamage: Including
- Rheumatoid arthritis.
- Gout
- Seronegative spondarthritis.
- Septic arthritis.
- Perthes disease.
- Avascular necrosis.e.g-Cortico steroid therapy.
b) Metabolic disease:
- Chondrocalcalcinosis
- Acromegaly
- Hereditary haemachromotosis.
c) Hematological factor:
- Haemophilia. E.g: recurrent haemarthrosis.
- Haemoglobinopathies. E.g: Sickle cell anaemia.
- Neuropathies.
d) Mechanical factors:
- Trauma &meniseal…
- Joint hypermobolity
- Joint dysplasia
e) Others:
- Congenital structure defect.
- Neurogenic arthropathies.

Risk factors of osteoarthritis: Remember the risk factors: Osteoarthritis –
- O = Obesity
- S-Senility or old age.
- T = Trauma.
- F = Emotional stress.
- O= Osteoporosis.
- A = Alcohol.
- R = Rigorous lifestyles.
- T = Taxing professions.
- H=Hormonal imbalance.
- R = 1 Repetitive injuries.
- I = Indian cultural habits
- T = Axing sports.
- I = Improper postural habits
- S = Smoking.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-676]
Types of osteoarthritis and their cause:
1. Primary osteoarthritis; primary osteoarthritis is a disease process present in individuals without history of joint injury, joint disease, or other systemic illness associated with osteoarthritis. It may be further classified into:
a) Localized: If an individual has osteoarthritis in one or two joints(e.g- both hip) the disease is classified as localized
b) Generalized: If there are three or more joints affected is classified as generalized. Primary osteoarthritis is somewhat more common in women. It develops spontaneously in middle age and progressive slowly as an exaggeration of the normal againg process. .
2.Secondary osteoarthritis: Secondary osteoarthritis usually develops following-
a) Trauma.
b) AVN of the femoral head.
c) Developmental dysplasia.
d) Slipped capital femoral epiphysis.
e) Perthes’ disease and
f) Enzymatic degradation of the articular cartilage in septic arthritis.
[Ref-Bailey & Love’s short practice of surgery 25th edition, page-517]
Clinical features of osteoarthritis:
A. Clinical symptoms:
a. Pain:
1) Deep aching, localized joint pain and pain may severe in the morning.
2) Patient over age 45 (often over age 60)
3) Insidious onset over months or years.
4) Variable or intermittent over time (‘good days, bad days’)
5) Mainly related to movement and weight-bearing, relieved by rest.
6) Only brief (<15 minutes) morning stiffness and brief (<1 minute) ‘gelling’ after rest. Usually only one or a few joint painful (not multiple regional pain).
b. Loss of function.
B. Clinical signs:
1) Restricted movement (capsular thickening, blocking by osteophyte). 2) Palpable, sometime audible, coarse crepitus (rough articular surfaces)
3) Bony swelling (osteophyte) around joint margins.
4) Deformity, usually without instability owing to-
✔ Loss of articular cartilage
✔ Collapse of subchondral bone.
✔ Overgrowth bone
✔Atrophy of adjacent muscle.
5) Joint-line or periarticular tenderness.
6) Muscle weakness, wasting.
7) No or only mild synovitis (effusion, increased warmth).
8) Enlarge joint due to formation of sprue.
C. Special feature:
1) Knee involvement- Varus volgus( knocked knees), flexion deformity, crepitus and limited ROM.
2) Heberden node- Bony protuberances occurring on the dorsal surface of the distal interphalangeal joints of the fingers.
3) Boucherss nodes- Bony protuberances occurring on proximal interphalangeal joints of the fingers.
4) Coxarthrosis(degenerative joint diease of the hip)-Pain in the hip on weight bearings, with pain progressing to include groin and medial knee and limited ROM.
[Ref-Davidson’s “Principles & Practice of Medicine” 21″ edition page-1085]
Investigation for confirming osteoarthritis:
1. CBC: Normal ESR.
2. Plain X-ray is usually the only useful investigation and show:
✔S Focal narrowing of joint space and osteophyte formation (cardinal features).
✔S Subchondral sclerosis (focal increased density of bone)
✔S Cysts and osteochondral ‘loose’ bodies within the synovium.
✔S Increased association with chondrocalcinosis.
3. Synovial fluid as pirated from OA knees (shows variable characteristics but is predominately viscous with low turbidity).
4. CPPD (Calcium pyrophosphate dehydrate) crystals may be identified in up to 50% of knee OA fluids.
5. Radioisotope bone scans (Often show increased uptake in OA joints due to bone remodeling).
6. Unexplained young-onset OA requires additional investigation guided by the suspected underlying condition.
[Ref-Davidson’s “Principles & Practice of Medicine 21” edition, page-1087]

Typical symptoms of osteoarthritis:
1. Pain.
2. Early morning stiffness.
3. Restricted range of joint movements.
4. Swelling of the joints.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-67]
Aim of treatment of osteoarthritis patient:
1. Relieve pain
2. Restore function
3. Reduce disability of the any part of body.
4. Rehabilitation.
A. General or non specific or management:
a. During acute stage rest is essential.
b. Diet should be adjusted that it helps reduction of overweight.
e. Unusual strenuous joint movements must be avoided.
d. Occupation may be changed if required.
e. Maintenance of strength & instability by exercise.
f. Physiotherapy may be required.
g. Gradually rehabilitation may be done by using appliance like chair etc.
h. Local heat, ice packs, contrast birth may relieve muscle spasm &stiffness.
i. Hydrotherapy: especially in the lower limb.
j. Self education: Educating the patients and family measures about the disease is the important aspect of the not- pharmacological treatment and should be done first-
✔Health professional & social support.
✔ Weight loss.
✔ Physiotherapy.
✔Therapeutic exercise.
✔Assistive device.
✔Occupational therapy.
✔Strengthening of the quadriceps.
✔Supervised fitness walking programme,
✔Swimming/ hydrotherapy.
✔Modification of actinity of daily living.
B. Specific management:
1. Non-opioid analgesics: e.g- Paracetamol- this is the drug of first choice up to 1 gm/day can be used.
2. NSAIDs: Give if pt fail to response paracetamol. E.g- Aspirin, Indomethacin, Piroxicam.
3. Opiod analgesies: This can be tried if pts fail to respond paracetamol or NSAIDs.
4. Food supplementation: Glucosamine & Sulfate can reduce 20-25% pain in mild to moderate over the counter food suppliments 1500mg/day for at least 3 months.
5. Intra-articular steroid injection: This is indicated if there is effusion & there are sign of inflammation.
6. Viscosupplimentation: Injection of hyaluronic acid into the joint. This is indicated for the removal of pathogenic osteoarthritis synovial fluid & replacement of hyaluronan based products that restore molecular weight concentration of hyaluronan. 7. Topical analgesics: These are indicated in the following situation:
✔ If patient do not respond to the oral analgesics.
✔ If the patient do not wish to take systemic drugs.
✔Can be used as a nontherapy or adjunct.
Capsaicin-4 times a day.
8. If conservative measure fail: Then surgery total replacement, arthroplasty has transformed the management of severe knee or hip OA.
C. Surgical management:
The surgical options include-
1. Arthrodesis.
2. Osteotomy.
3. Joint replacement in the form of a resurfacing arthroplasty.
4. Total joint replacement.
D. The choice of a particular procedure is based upon-
1. The age of the patient.
2. The lifestyle.
3. Activity status and
4. The stage of the disease.
[Ref-Bailey & Love’s short practice of surgery 25 edition page->518]
Aims of treatment of osteoarthritis (OA) knee:
It can be best illustrated by 4 R’s:
1. Relieve pain.
2. Restore function.
3. Reduce disability if any.
4. Rehabilitation.
[Ref-John Ebnezar’s “Textbook of Orthopedics” edition page-679]
Role of exercise in the management of osteoarthritis of the hip and knee:
1. Built-up the exercises gradually.
2. Avoid rough ground while exercising.
3. To take warm baths before starting the exercises.
4. To perform the exercises 20 times each twice a day and later four times a day.
(Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-686)
Aims of the exercises in osteoarthritis hip and knee:
1. To increase the range of movements.
2. To increase stability and shock absorption.
3. To prevent deformity
4. To improve posture.
5. To reduce pain and stiffness,
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-686]
The causes for secondary osteoarthritis of the knee are as follows:
1. Obesity.
2. Valgus and varus deformities of the knee.
3. Intra-articular fractures of the knee, etc.
4. Rheumatoid arthritis, infection, trauma, TB, etc.
5. Hyperparathyroidism.
6. Hemophilia.
7. Syringomyelia.
8. Neurological disease like diabetes.
9. Overuse of intra-articular steroid therapy.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-682]
Nursing management for osteoarthritis patient:
As a graduate nurse I will provide following nursing care for an osteoarthritis Patient:
A) Nursing assessment:
a) Obtain history of deep aching, localized joint pain, joint crepitation & client may complain at audible joint” grinding”.
b) Assess joint for swelling, tenderness & range of motion, contractures, atrophy of adjunct muscle.
c) Assess for sleep pattern disturbance, alteration in activities of daily living, lack of appetite & altered self concept.
B) Nursing diagnosis:
a) Alteration in comfort, acute & chronic pain related to disease process.
b) Impaired physical mobility related to joint stiffness, deformity & operative procedure.
c) Sleep pattern disturbance related to pain & anxiety.
d) Alteration in daily living activities related to adverse effect of drug therapy.
e) Activity intolerance related to fatigue & pain.
f) Altered in nutrition les than body requirement related to loss of appetite.
C) Nursing intervention:
1. Promoting comfort & relieving pain:
a) Provide comfort measures to reduce or alleviate pain.
b) Assess for level of pain related to joint stiffness, deformity and trauma.
c) Assess for limited joint motion.
d) Avoid forceful & repitative movement.
e) Handle patient gently.
2. Maintain muscle strength & improve physical activities:
a) Assess for the degree of functional limitation related to pain, stiffness & deformities.
b) Encourage range of motion exercise to maintain muscle strength.
c) Conduct exercise/activities programme to maintain joint function.site
d) Use orthopedic device & ambulatory aids.
e) Encourage consultation with physical therapist as indicated.
3. Maintenance of sleep pattern:
a) Promote rest & sleep.
b) Teach relaxation methods to promote sleep.
c) Use of analgesics as needed.
d) Discuss use of bed time routine to promote sleep.
4. Maintenance of daily activity of life:
a) Discuss the need to modify activities environment to accommodate limitations.
b) Increased activity as tolerate.
c) Provide for & teach use of assistance device as needed-
✓-Gait device(rubber-tipped, crutches, canes, walks)
✓-Orthopedic devices.
✓-Rained toilet seats.
d) Demonstrate using assistive devise to perform self care activities & accomplish daily tasks.
e) Teach problem solving skills for dividing. To be done.
5. Improving activity tolerance:
a) Encourage frequent rest period & light activity as toleratd.
b) Identified the specific physical & psychological activities that are fatiguing.
c) Assess pt in recognizing daily activities to optimize rest periods & to avoid excessive activity.
d) Instruct principle of energy conservation.
6. Promote optimal nutritional status:
a) Assess for lack of appetite, anorexia, anaemia in client with systemic disorder.
b) Integrate pts personal, cultural & aged related food preferences, practices appetite 7 eating patterns into dietary planning.
c) Develop a wt reduction plan & activity prescription for over wt client.
d) Assess for underlying depretion or grief which may contribute to dietary imbalacce.
7. Patient education and health maintenance:
a) Teach pt about pain relief method.
b) Teach pt about the importance of regular physical exercise.
c) Teach pt about relaxation method & how to use analgesics.
d) Encourage the pt use of assistive device.
e) Encourage the pt
f) Encourage the patient to keep the wt of optimal level & maintain well balanced diet.
D) Expected outcome:
a) Pain is decreased or relieved.
b) Patient has increased mobility & muscle strength & no joint deformities.
e) Patient has adequate sleep and rest.
d) Patient demonstrates optimal independence in activities of daily living.
e) Patient tolerates activity without fatigue or pain.
f) Patient maintains optimal nutrition.
Factors are responsible for secondary osteoarthritis of the hip:
The following factors are responsible for the development of sector osteoarthritis of the hip joint:
1. Incongruity of the articular surface. E.g.
✔ Trauma.
✔ CDH.
✔ Slipped epiphysis.
2. Instability of the hip. E.g.
✔Subluxation.
3.Concentration of pressure load. E.g.
✔Coxa vara.
✔ Ante version.
4. Constitutional causes. E.g.
✔ Obesity
✔Hyperthyroidism.
5. Direct injury. E.g.
✔Infection.
✔Trauma.
6. Bone diseases like –
✔ AVN.
✔Rheumatoid arthritis.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition page-4]
Indications for osteoarthritis surgery:
1. Pain refractory to conservative measures.
2. History of frequent locking episodes.
3. Hemarthrosis due to loose bodies or osteochondral fractures.
4. Deformity, usually genu varum.
5. Joint instability.
6. Progressive limitation of knee motion.
[Ref-John Ebnezar’s “Textbook of Orthopedics” edition]
Complications of osteoarthritis:
1. Acute compartmental syndrome.
2. Chronic compartmental syndrome.
3. Crush syndrome.
4. Peripheral neuromuscular dysfunction.
5. Deep vein thrombosis.
6. Pulmonary embolism
7. Fat embolism.
8. Capsular herniation.
9. Loose bodies.
10. Rotator cuff dysfunction.
11. Spinal stenosis.
12. Spondylolisthesis.
13. Subluxation.
14. Ankylosis.
15. Haemophilia.
16. TB, trauma.
17. Mucinous cyst.
18. Syringomyelia.
19. Hyperparathyroidism.
20. Joint deformities.
[Ref-Apley’s “System of Orthopaedics and Fractures” h edition page-93]
Cardinal features of osteoarthritis:
1. Progressive cartilage destruction.
2. Subarticular cyst formation.
3. Sclerosis of the surrounding bone.
4. Osteophyte formation.
5. Capsular fibrosis.
[Ref-Apley’s “System of Orthopaedics and Fractures” 9″ edition page-88]
Type of exercise in osteoarthritis of hip:
A) Exercises lying on the back:
1. Pelvic tilt: Tighten the thigh and buttock muscles, pushing the knees flat, hold for a count of five and relax.
2. Pelvic lift: Bend both the knees up, push on the feet and lift, hold for a count of five and relax.
3. Leg stretch: Push one leg along the floor as through you are trying to make it longer than the other. Hold for a count of five and then repeat with the other leg.
4. Alternate leg exercise: Keeping the knees straight, lift alternate legs six inches from the ground.
B) Exercise laying on your side, with the painful Hip up:
1. Side leg rising: Keep the top leg straight and lift it as high as possible, hold for a count of five and relax.
2. Knee and hip flexion: Bend the hip and knee of the top leg forwards, and hold for a count of five. Then straighten the leg and stretch backwards as far as it will go, hold for a count of five, then relax.
C) Exercise for sitting posture:
1. Knee together, feet apart: Keep the ankles together and move the knees apart, then relax.
2 . Feet together, knees apart: Keep the ankles together and move the knees apart, then relax.
D) Exercise in standing posture:
1. Standing leg swing: Hold into a table or chair with one hand, swing one leg forward and backward. Try to get the backwards swing as wide as possible.
2. Standing side leg swing: Hold on to a chair with both hands. Swing bad leg out as far as it will go and then in. The outward swing is the hardest part and the leg should be allowed to fall back under muscular control.
a) Possible diagnosis: Osteoarthritis.
b) See above.
c) See above
