Concept about Osteosarcoma – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Definition of hone tumor:
According to the eminent British oncologist Sir Rupert Willis: A neoplasm is an abnormal mass of tissue the growth of which exceeds and is uncoordinated with that of normal tissue & Persists in the same excessive manner after cessation of stimuli which evoked the changes.

[Ref-Rabhins, Pathology, edition, Page-260]
or
Neoplasm’s originating in bone may arise from osseous tissue or forming cartilaginous cells associated with the epiphyses or from the blood forming elements contained in red bone marrow.
(Ref-JN ASTON’S, “Orthopedics and Traumatology”, 2 edition)
Causes of tumors:
Causes of tumors is not clearly understood-
A) Carcinogens/Acquired environmental factors.
B) Genetic factors.
C) Predisposing or risk factors.
A) Carcinogens / Acquired environmental factors:
1) Chemical carcinogen:
a) Directly acting: Dimethyl sulphate, Dimethyl carbamyl chloride.
b) Indirectly acting: Benzopyrene, Benzidine, Alfatoxin, Griseofulvin, Nickel, Chromium, Asbestos, Arsenic.
2) Physical carcinogens(radiation energy)
a) UV-Rays: Derived from sunlight (UV320-400nm)
b) lonizing radiation.
c) Electromagnetic: X-rays, gamma rays.
d) Particulates: Alpha particulates, beta-particulates, Proton
3) Human oncogenic virus:
Virus producing cancer cells predominantly
a) DNA Virus: Human papiloma virus, Epsteinbarr virus, Hepatitis B virus, Kaposi sarcoma herpes virus.
b) RNA virus: Human T-cell leukaemia virus type-1, Hepatitis C virus
B) Genetic factors: Inherited tumors
C) Predisposing or Risk factors:
1) Host factors:
a) Age:
- Old age (>60Years) =Carcinoma.
- Young age Sarcoma
b) Hormone: Breast and endometrial carcinoma due to estrogen deficiency.
c) Premalignanat condition & genetic predisposition.
2) Environmental factors: Diet, cigarette smoking, Alcohol consumption, Air pollution, Occupational hazards.
3) Hormones: Oestrogen, Pituitary hormones, Androgen.
4) Cancer following chronic diseases.
5) Miscellaneous- Schistosomasis.
[Ref-Robbins, Pathology, edition, Page-312-315]
Definition of benign tumors:
Benign tumor is that tumor which is well differentiated, usually grows progressively and slowly but do not invade the surrounding structure and do not metastasis.
[Ref-Dr.Mosharraf Hossain, Pathology & haematology, 5th edition.page-148]

Malignant tumor:
Malignant tumor is one where tumor grows slowly and invade the surrounding tissue which could not well differentiated but create fatal complication.
Classification of bone tumors according to origin:
A) Primary bone tumors:
| Predominant tissue | Benign tumors | Malignant tumors |
| 1) Bone forming |
|
|
2) Cartilage forming |
|
|
| 3) Fat forming tumor |
|
|
| 4) Fibrous tumor |
|
|
| 5) Vascular tumor |
|
|
| 6) Giant cell tumor |
|
|
| 7) Marrow tumor |
| |
| 8) Other |
|
B) Secondary bone tumors: Metastasis are the most common bone tumors in adults.
1) Breast (35%)
2) Lung (30%)
3) Prostate (25%)
4) Kidney (5%)
5) Thyroid (2%)
[Ref-Baily & Loves, Short practice of surgery, 25th edition, Page-548]
Differences between benign and malignant tumors:
| Traits | Benign tumors | Malignant tumors |
| 1) Differentiation | Well differentiated | Less or no differentiation |
| 2) Anaplasia: a) Pleomorphisms b) Orientation of neoplastic cell c) Neucleus & Cytoplasm ratio | Absent Not disturbed Not altered | Often present Disturbed Altered |
| 3) Rate of growth | Usually slow & progressive | Irregular & may be slow |
| 4) Local inCvasion | Usually cohesive & Extensile mass Do not invade the surrounding tissue. | Locally invasive & infiltrative the surrounding tissue. |
| 5) Metastasis | Absent | Usually present |
| 6) Size | Usually small | Usually large |
| 7) Stroma | Well formed | Poorly formed |
| 8) Haemorrhage & necrosis | Little tendency | Common to occur. |
| 9) Capsule | Usually capsulated | Usually uncapsulated |
| 10) Effects | Effects are not fatal. Eraly detection can prevent fatal effect | Serious or fatal effect |
| 11) X-rays shows | Some lesion | III defined border, mottoled appearance, cortex of bone may be broke |
Characteristics of benign tumour:
Please see above.
Characteristics of malignant tumour:
Please see above.
Silent features of tumors:
1. Pain
2. Mass.
3. Disability
4. Anorexia.
5. Weight loss.
6. Fever.
7. Onset-It is acute in malignant tumors and insidious in benign tumors.
8. Age-Certain tumors have predilection for certain age groups, e.g. Ewing’s sarcoma has a predilection for children.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, P-616]
Staging of benign bone tumors as described by Enneking:
There are three stages of benign bone tumor:
1) Latent stage:
a) Well defined margin,
b) Grows slowly and then stops,
c) Remains static or heals spontaneously, e.g. Osteoid osteoma.
2) Active stage
a) Progressive growth limited by natural barriers,
b) Not self-limiting,
c) Tendency to recur, e.g. Aneurysmal bone cyst.
3) Aggressive stage:
a) Growth not limited by natural barriers, e.g. Giant cell tumor.
[Ref- Apley’s “System of orthopedics and fractures”, 9 edition, P-191]
Tumor can be diagnosed in the laboratory:
A) Routine examination
B) Cytology
C) Tumor marker
A) Routine examination:
1) Sample collection material are taken by Biopsy, Whole tumor mass.
2) Histopathology:
- Paraffin section method
- Frozen section method.
B) Cytology:
1) FNAC (Fine needle aspiration cytology): From breast tumor, liver prostate, thyroid.
2) Exfoliative cytology: Exfoliative cells are used to appear smear and staining. Materials are –
- Vaginal smear (PAP smear)
- Stomach aspirate
- Sputum
- Urine
- Body fluid.
C) Tumor marker:
These are biochemical mediators of the presence tumor.these include cell surface antigen, enzymes, hormones.
| Markers | Associated cancer |
| Hormones:HCG | Trophoblastic tumor |
| Antigen: Alpha fetoprotein | Liver cell carcinoma. |
| Enzymes: Acid phosphate | Ca prostate |
| Protein:Immunoglobulin | Multiple myeloma |
[Ref-Dr.Mosharraf Hossain, Pathology & haematology, 5 edition,page-148]
Biopsy:
(Bio Life, Opsis Vision) Obtaining of a representative tissue sample for microscopic examination due to establish diagnosis.
Types of biopsy:

There are two types of biopsy:
1) Closed biopsy:
a) Needle biopsy
b) Aspiration biopsy
2) Open biopsy:
a) Incisional biopsy
b) Excisional biopsy (Biopsy taken after removal of an organ)
[Ref-Bailey & Love’s, 25th edition, Page-167]
How to send biopsy in the laboratory:
1. Biopsy is sent to laboratory with 10% formalin If not available, we can use normal saline.
2. Fatty tissue (e.g. lipoma) is sent with normal saline.
[Ref-Bailey & Love’s, 25 edition, Page-167]
Investigation for bone tumors:
A) Routine investigation:
1. HB%: Increased.
2. TC, DC, ESR: Increased.
3. S. Calcium, S.Phosphorus: Increased.
4. S.alkaline phosphate: Increased in osteogenic sarcoma.
5. S.acid phosphate: Increased in metastatic tumors.
B) Special investigation:
X-ray of involved part,CT scan, Angiography, Arteriography. Ultrasonography, MRI, Bone scan Biopsy.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, P-616]
Differential diagnosis:
1. Soft tissue haematoma.
2. Myositis ossifications.
3. Stress fracture.
4. Tendon avulsion injuries.
5. Bone infection.
6. Gout.
7. Other bone lesions.
[Ref-Apley’s “System of orthopedics and fractures”, 9 edition, P-187]
Principle of treatment of bore tumor:
Consultation and cooperation among the orthopedic surgeon, radii pathologist and (in case of malignant tumors) oncologist is essential in the management. In many cases physiotherapist, occupational therapists and prosthetist, will also be involved.
1. Benign, asymptomatic lesions: If the diagnosis is beyond doubt (e.g. non-ossifying fibroma or a small osteochondroma) one can afford to temporize, treatment may never be needed. However, if the appearances are not pathognomonic, a biopsy is advisable and this may take the form of excision or curettage of the lesion.
2. Benign, symptomatic or enlarging tumors: Painful lesions or tumors that continue to enlarge after the end of normal bone growth, require biopsy and confirmation of the diagnosis. Unless they are unusually aggressive, they can generally be removed by local (marginal) excision or (in case of benign cysts) by curettage.
3. Suspected malignant tumors: If the lesion is thought to be a primary malignant tumor, the patient is admitted for more detailed examination, blood tests. Chest X-ray, further imaging (including pulmonary CT) and biopsy. This should allow a firm diagnosis and staging to be established. The various treatment options can then be discussed with the patient (or the parents, in case of a young child). A choice needs to be made between amputations, limb-sparing operations and different types of adjuvant therapy and the patient must be fully informed about the pros and cons of each.
Methods of treatment of bone tumor:
1) Tumor excision: The more aggressive lesion the more widely does it need to be excised.
a) Intracapsular (intralesional) excision and curettage: Incomplete forms of tumors ablation.
b) Marginal excision: Excision goes beyond the tumor,but only just
c) Wide excision: Dissection is carried out well clear of the tumor, through normal tissue
d) Radical resection: The entire compartment in which the tumor lies is removed en block without lesion.
2) Limb salvage: Amputation is no longer automatic choice for grade Il sarcoma.Improved method of imaging and advances in chemotherapy have made limb salvage the treatment of choice for many patients.
3) Amputation conly choice when severity of tumor is harmful to the surrounding tissue and chance of metastasis.
4) Multi-agent chemotherapy
5) Radiotherapy.
[Ref- Apley’s “System of orthopedics and fractures”, 9 edition, P-192-193]
Choice of surgical procedure of tumor:
Surgery is usually advocated for local control of the tumor. Enneking’s staging of the tumor Tumor decides the choice of surgery as suggested below,
| Stages of tumor | Methods of treatment |
| Grade I A | Require local procedure |
| Grade 1 B | Wide excision |
| Grade II A | Radical excision |
| Grade II B | Radical excision |
| Grade III | Surgery+Chemotherapy+Radiotherapy |
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4″ edition, Page-617]
Different sites of long bone tumor:
| Site | Bone tumor |
| Metaphysis | Osteosarcoma |
| Diaphysis | Ewing’s tumor |
| Epiphysis | Osteoclastoma or Giant cell tumor |
(Ref-Dr. Jahir’s, “Surgery Paper-I”, Edition-2010, P-575)
Highly malignant tumors of bone:
a) Osteosarcoma.
b) Chondrosarcoma.
c) Ewing’s sarcoma.
d) Multiple myeloma
e) Fibrosarcoma
Concept about Osteosarcoma
Definition of osteosarcoma:
Osteosarcoma is defined as a malignant mesenchymal tumor in which the cancerous cells produce bone matrix.
[Ref-Robbins, Pathology, 8th edition, Page-317]
Or
Osteosarcoma is a highly malignant tumor arising within the bone and spreading rapidly outwards to the periosteum and surrounding soft tissues.
(Ref- Apley’s “System of orthopedics and fractures”, 9h edition, P-207)
Or
Osteogenic sarcoma or osteosarcoma is a highly malignant bone tumor which arises from primitive bone forming cells. It destroys the bone structure and eventually bursts into the surrounding tissue. It may be composed of fibrous tissue of cartilage or of myxomatous tissue and benigns in the metaphysic. It predominantly affects children or adolescent.
Or
[Ref-Adams, Text Book of pathology, 11 edition, Page-88]
Osteogenic sarcoma is a highly malignant tumor, where tumor cells invariably form a neoplastic osteoid, bone or both.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, P-624]
Common sites of osteosarcoma:
1) Lower end of the femur.
2) Upper end of the tibia
3) Upper end of the humerus.
4) Lower end of the radius

Stages of osteosarcoma:
The stage of a cancer is a term used to describe its size and whether it has spread beyond its original site. Knowing the particular type and stage of a cancer helps the doctors decide on the most appropriate treatment. Most people are grouped depending on whether cancer is found in only one part of the body (localized disease) or whether the cancer has spread from one part of the body to another (metastatic disease).
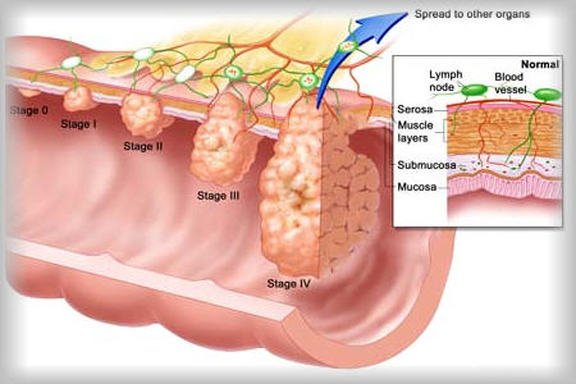
1) Stage IA: The cancer is low-grade and is contained within the hard coating of the bone.
2) Stage 1B: The cancer is low-grade and extends outside the bone into the soft tissue spaces, which contain nerves and blood vessels.
3) Stage 2A: The cancer is high-grade and is completely contained within the hard coating of the bone.
4) Stage 2B: The cancer is high-grade and extends outside the bone into the soft tissue spaces, which contain nerves and blood vessels. Most osteosarcomas are stage 2B.
5) Stage 3: The cancer can be low-grade or high-grade and it’s found either within the bone or extending outside the bone. In stage 3, the cancer has spread to other parts of the body, or to other bones not directly connected to the bone where the tumor started. If the cancer comes back after initial treatment, this is known as recurrent or relapsed cancer.
Characteristics facts of osteogenic sarcoma:
1) Highly malignant bone tumor.
2) Arises from multipotent cells.
3) Most frequent primary bone tumor next only to multiple myeloma.
4) 75% are below 25 years of age.
5) 90% occur in the metaphysis.
6) Neoplastic osteoid is always present.
7) Both osteosclerotic and osteolytic variety is the most common.
8) Leg of mutton appearance.
9) Spindle cells.
10) No giant cells.
11) Pain is the first symptoms,
12) Skin is stretched, shiny and dilated veins are present.
13) Pathological fractures are not common.
14) 80% has blood spread.
15) Sunray appearance and Codman’s triangle are special X-ray feature.
16) Multipronged approach gives better survival rate.
Causes of osteosarcoma:
1) Primary sarcoma: tumors originate in the bone or soft connective tissue. Primary tumors caused by,
a) Primary bone tumors,
b) Primary soft connective tissue tumors.
2) Secondary sarcomas are caused by metastasis from other organs such a lung, thyroid glands or liver.
3) Risk factors are associated with sarcoma
a) Infection.
b) Hormonal deficiency.
c) Trauma & Injuries.
d) Virus-DNA virs, RNA virus.
e) Radiation.
f) Chemicals: 20-methyl cholanthrene, Beryllium compounds etc.
g) Paget disease of bone.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4 edition, P-626]
Classification of osteosarcoma:
A) On the basis of site of involvement
1) Primary osteosarcoma.
2) Secondary osteosarcoma.
B) Dahlin’s (Prognostic) classification:
1) Osteoblastis: Poor five year survival rate.
2) Chondroblastic: Five year survival rate is three times more than that < osteoblastic variety.
3) Fibroblastic: Five year survival rate is two times more of osteoblastic variet)
C) Geschickter and Copeland classification:
1) Sclerosing type.
2) Osteolytic type.
3) Mixed type of both osteoblastic and osteolytic varieties.
4) Telangiectatic type.
(Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4″ edition, P-626)
Clinical features of osteosarcoma:
1. Age: Commonly found in children between 9 and 16 years.
2. Sex: Male > Female.
3. Site: Around the knee and upper arm.
4. Gradual onset of pain and swelling.
5. Swelling is firm near the end of a bone, close to the joint (Metaphysis).
6. Limitation of the motion.
7. Loss of weight.
8. General weakness.
9. The patient may complain of fatigue.
10. Haemorrhage.
11. Anaemia.
12. Overlying skin is warmer than normal, stretched and shiny.
13. Pathological fracture.
14. Foot drop if common personal nerve and anterior tibial nerves are involved.
15. Cough, dyspnoea, haemoptysis: if pulmonary metastasis.
16. Abdominal discomfort, jaundice: if liver metastasis.

(Ref-Adams/11 edition, P-/86,87)
Radiological evaluation of osteosarcoma:
Plain X-rays of the affected area are usually sufficient to make a diagnosis of osteosarcoma. The classic features of osteosarcoma are:
- Poorly delineated or absent margins around the bone lesion
- Bone destruction
- New bone formation with calcification of the matrix
- Periosteal reaction, usually non-continuous and thin, with multiple laminations
Note: histological confirmation of the radiological diagnosis must be deferred until the patient is assessed by a surgeon with expertise in the management of bone malignancies.
Investigations are done to diagnose osteosarcoma:
Usually you begin by seeing your family doctor (GP), who will examine you and may arrange any necessary tests or x-rays. If a bone tumour is suspected, you’ll be referred directly to a specialist hospital or bone tumour centre for further tests. A variety of tests and investigations may be needed to diagnose an osteosarcoma.
1) Bone x-ray: This involves the use of x-rays to build up a picture of the bone.
2) Needle biopsy: For this test a small sample of the tumour is taken from the affected bone. The doctor then examines the sample under a microscope to identify the exact type of tumour you may have.
3) Open biopsy: This type of biopsy is not often used, as the needle biopsy is much quicker and simpler. In an open biopsy a small piece of bone is removed during a minor operation while you’re under a general anaesthetic. It may be necessary to do this if a needle biopsy can’t be done or doesn’t give a clear diagnosis.
4) Bone scan: This is a more sensitive test than the simple x-ray and shows up any abnormal areas of bone more clearly. For this test, a small amount of a mildly radioactive substance is injected into a vein, usually
in your arm. Abnormal bone absorbs more radioactivity than normal bone so these areas are highlighted and picked up by the scanner as hot spots.
5) MRI (magnetic resonance imaging) scan: This test is similar to a CT scan (see below), but uses magnetism instead of x-rays to build up crosssectional pictures of your body. During the test, you’ll be asked to lie very still on a couch inside a largemetal cylinder that is open at both ends. The whole test may take up to an hour.
It can be slightlyuncomfortable and some people feel a bit claustrophobic during the scan.It’s very noisy, but you will be given earplugs or headphones. You’ll be able to hear, and speak to, the personoperating the scanner. If you have any metal implants (such as surgical clips, pacemakers, metal in the eye from previous accidents or trauma), it will not be possible for you to have this test.
6) CT (computerized tomography) scan: A CT scan takes a series of x-rays that build up a three- dimensional picture of the inside of the body. The scan is painless and takes just a few minutes. CT scans use small amounts of radiation, which is very unlikely to harm you or anyone you come into contact with. You’ll be asked not to eat or drink for at least four hours before the scan. You may be given a drink or an injection of dye that allows particular areas to be seen more clearly.
This may make you feel hot all over for a few minutes. If you’re allergic to iodine or have asthma, you could have a more serious reaction to the injection so it’s important to let your doctor know beforehand. We’ll probably be able to go home as soon as the scan is over.
7) PET (positron emission tomography) scan or PET-CT scan: This uses low-dose radioactive sugar to measure the activity of cells in different parts of the body. A very small amount of a mildly radioactive substance is injected into a vein, usually in your arm. A scan is then taken a couple of hours later. Areas of cancer are usually more active than surrounding tissue and show up on the scan. Sometimes a type of scan that combines a PET scan and a CT scan
[Ref- European Society of Medical Oncology (ESMO) Clinical practice guideline, Volume-21,Edition 2010]
Bone tumor on the basis of location:
| Sites of bone | Tumor type |
| Proximal humerus | Simple bone cyst. |
| Epiphysis | Chondroblastoma Giant cell tumor |
| Tibia | Adamantioma |
| Sacrum | Chordoma |
| Posterios spine | Osteoblastoma |
| Distal femur | Parosteal sarcoma |
| Tibia | Periosteal sarcoma |
Treatment of osteosarcoma:
As osteosarcomas are very rare, they are usually treated at specialist hospitals by a team of doctors and other health professionals.
1) Surgery:
Major improvements have been made in surgery for bone cancer. In the past, it was often necessary to remove (amputate) the affected limb if osteosarcoma was found. Now it’s often possible just to remove the affected part of the bone and some of the healthy tissue around it. The bone is then replaced with a specially designed metal replacement (prosthesis) or a bone graft (bone taken from another part of the body). If the cancer affects a bone in or near a joint, the whole joint can often be replaced with an artificial
one. These operations are known as limb-sparing surgery. Unfortunately, it’s not always possible to use limb-sparing surgery and sometimes removing the whole of the affected limb (amputation) may be the only way to treat the cancer. This is often due to the cancer
spreading
2) Chemotherapy:
Chemotherapy is the use of anti-cancer (cytotoxic) drugs to destroy cancer cells. It’s an important treatment for most people with osteosarcoma as it can greatly improve the results of surgical treatment. It is usually given before surgery and may shrink large tumours enough to avoid amputation. The course of chemotherapy continues after surgery to destroy any remaining cancer cells and to stop the sarcoma from spreading outside the bone.
3) Radiotherapy:
Radiotherapy treats cancer by using high energy rays to destroy the cancer cells, while doing as little harmas possible to normal cells. Radiotherapy is sometimes used after surgery and may be used to treat theprimary tumour (for example where surgery is not possible)
Sites of amputation:
1) On the tibia: Amputation through mid thigh. 2) Lower end of femur: Disarticulation of femur.
3) Upper end of femur: Hind quadrant amputation.
4) Upper end of humerus: Fore quadrant amputation.
[Ref-Adams/11 edition, P-/86,87]
Pre-malignant conditions of osteosarcoma:
1. Paget’s di sease of bone.
2. Fibrous dysplasia.
3. Multiple exostosis.
4. Oncogenic virus.
5. Radiation.
6. Chemical.
[Ref-Adams/11 edition, P-/86,87]
Nursing Interventions:
A) General nursing management:
1) Keep the patients in bed rest.
2) Immobilization of the joint by cast.
3) Give analgesics according to doctors order to relieve pain.
4) Maintainence of personal hygiene.
B) Special nursing care:
1) Chemotherapy: Various agents used singly or in combination before or after surgery Highdose methotrexate with citrovorum factor rescue, doxorubicin, bleomycin,actinomycin D, cyclophosphamide, ifosfamide, cisplatin, vincristine.
2) Nursing Considerations:
a) Control nausea and vomiting with antiemetics prior to treatment.
b) Manage side effects of treatment.
c) Client Education:
- Encourage to take chemotherapy.
- Assurance of the patients before chemotherapy.
- Check vital signs before chemotherapy.
- Give knowledge of patients about dose, cycle and next date of chemotherapy. Teach the family to recognize signs of infection, skin breakdown, and nutritional deficiency.
- Encourage the patients and family to maintain good hygiene.
- Instruct the family in the proper use of vascular access devices.
3) Limb amputation for osteosarcoma:
a) Provide routine pre and postoperative care.
b) Provide emotional support.
c) Care for the stump as prescribed.
d)Assess for the presence of phantom limb pain postoperatively and medicate appropriately.
e) Client Education:
- Prepare the patients for fitting of a temporary prosthesis, which may occur immediately after surgery.
- Encourage cooperation with postoperative physical therapy.
- Work with the patients and family to plan for issues such as appropriate clothing to wear with prosthesis.
- Role play issues that the patients will need to deal with after discharge, such as talking to strangers who ask about the prosthesis.
- Assist the family to recognize that the patients emotions, such as anger, are normal grief reactions after amputation, chemotherapy, and other treatments.
4) Localized radiation therapy :Radiation therapy may be used in combination with chemotherapy and surgery.
a) Assist the patients with positioning during radiotherapy.
b) Monitor for side effects of radiotherapy.
c) Educate the patients and family regarding the course of therapy.
5) Others:
a) Evaluate laboratory data and assess for symptoms of complications:
- Infection – Elevated WBC and fever.
- Hemorrhage Blood in urine or stool, bruising, and petechiae.
- Anemia – Fatigue and decreased hemoglobin/hematocrit.
b) Prevent infection:
- Provide a private room when hospitalized. Restrict staff/visitors who have infections.
- Promote frequent hand hygiene by staff/visitors.
- Avoid all live-virus vaccines during periods of immunosuppression.
- Ensure that siblings are up-to-date on vaccinations.
- Provide a diet adequate in proteins and calories.
c) Prevent hemorrhage or injury from bleeding:
- Use a strict aseptic technique for all invasive procedures.
- Use gentle technique when providing mouth care.
- Clean the perineal area carefully to prevent trauma and avoid obtaining temperatures rectally.
d) Prevention of anaemia:
- Provide rest periods as needed.
- Infuse packed red blood cells as prescribed.
6) Care After Discharge:
a) Educate the patients and family regarding the importance of follow-up care.
b) Initiate appropriate referrals to assist the child to resume normal activities (school attendance, physical activities).