Concept about Placenta praevia – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Concept about Placenta praevia
When the placenta is implanted partially or completely over the lower uterine segment, it is called placenta praevia.
or
Placenta previa is an obstetric complication in which the placenta is inserted partially or wholly in the lower uterine segment. It is a leading cause of antepartum haemorrhage (vaginal bleeding). It affects approximately 0.4-0.5% of all labours.
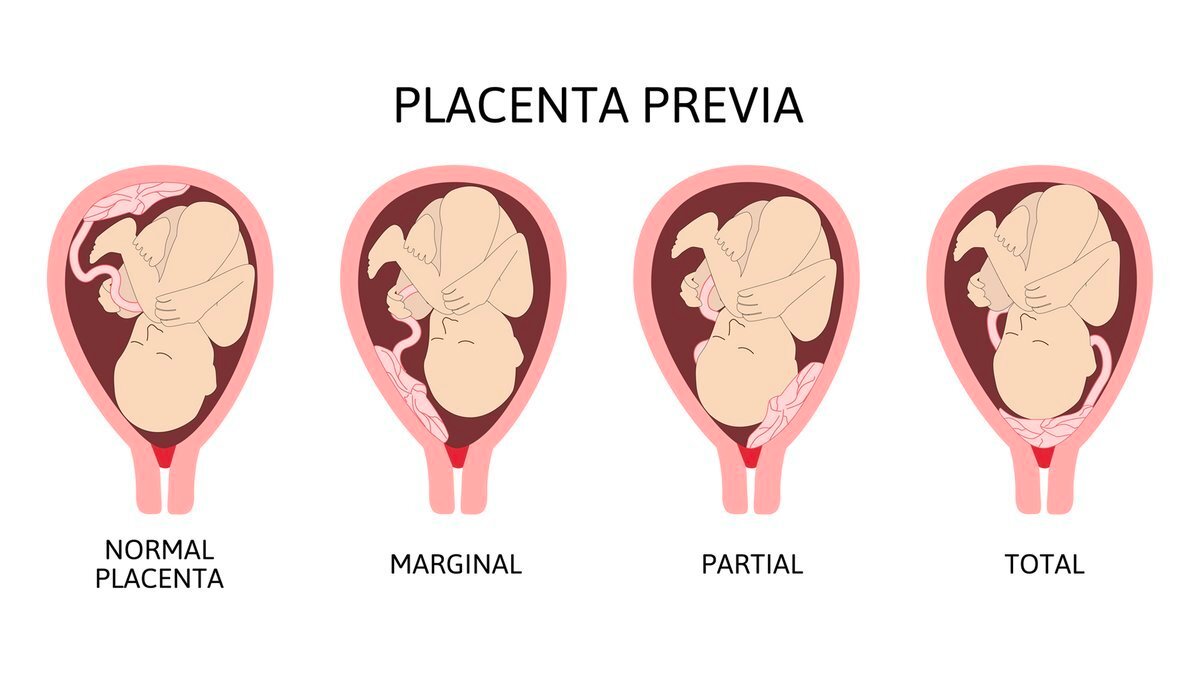
Types or Degree of Placenta Praevia:
1. Type I (low lying): The major part of the placenta is attached to the upper segment and only the lower margin encroaches onto the lower segment but not up to the OS
2. Type 2 (Marginal): The placenta reaches the margin of the internal OS but does not cover it.
3. Type 3 (Incomplete or partial central): The placenta covers the internal OS partially.
4. Type 4 (Central or total): The placenta completely covers the internal OS even after it is fully dilated.
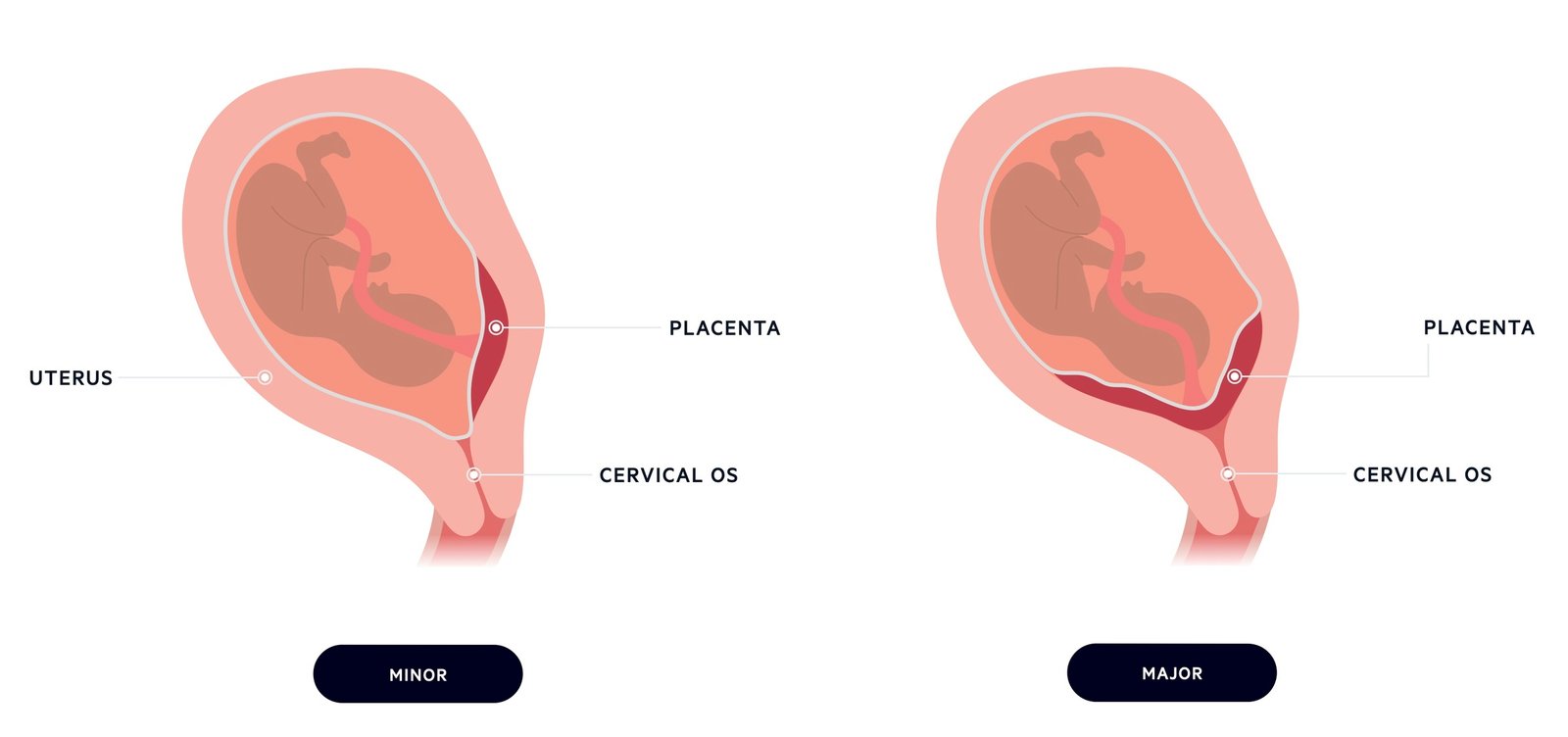
For clinical purpose, the types are graded in to –
1. Mild degree (Type 1 & 2 anterior)
2. Major degree (Type 2,3 &. type 4)
Clinical Features of Placenta Praevia:
A. Symptoms of placenta praevia –
Vaginal bleeding: Sudden onset, painless, apparently causeless and recurrent.
B. Signs of placenta praevia:
a) General signs: Anemia
b) Abdominal examination:
- The size of the uterus is proportionate to the period of gestation
- The uterus feels relaxed, soft, elastic and not tender
- Persistence of mal-presentation
- The head is floating
- Fetal heart sound is present
c) Per vaginal examination: On inspection, the blood is bright red.
Investigation:
- Blood for TC, DC, Hb% and ESR.
- Blood grouping and Rh. typing
- Blood sugar
- Serum creatinine
- Urine for RME
- Chest X-ray
- ECG
- Ultrasonogram
Management of Placenta Praevia:
At home:
1. Patient is immediately put to bed
2. To assess the blood loss
- Inspection of the clothing soaked with blood
- To note the pulse, BP, anemia.
3. Quick but gentle abdominal examination to mark the height of the uterus, to auscultation of the fetal heart sound and to note any tenderness on the uterus.
4. Vaginal examination must not be done
Transfer to hospital and admission to hospital:
Immediate attention:
- Amount of the blood loss
- Blood samples are taken for group, cross matching and estimation of Hb%
- An infusion of normal saline
- Gentle abdominal palpation
- Inspection of the vulva to note the presence of any active bleeding
Formulation of the line of treatment:
A. Expectant treatment: The aim is to allow the pregnancy to continue until baby grown sufficient enough to survive ex-utero
- Prerequisites:
– Availability of blood for transfusion
– Facilities for caesarean section available throughout 24 hours - Selection of cases –
– Pregnancy is less than 37 weeks
– Good maternal and fetal condition
– No active bleeding
B. Active treatment:
- Bleeding occurs at or beyond 37 weeks of pregnancy
- Patient is in labour
- Patient is in exsanguinated state on admission
- Bleeding in continuing and of moderate degree
- Baby is dead or known to be congenital deformed
Definitive treatment:
a) Vaginal examination: If the diagnosis is still uncertain after ultrasound examination, a pelvic examination is performed when the pregnancy is near term. It is done in the operation theatre with the woman anaesthetized and the instruments sterilized and ready for caesarean section
b) Termination of pregnancy:
1. ARM (low rupture of the membrane): If placenta praevia type 1 or type 2 anterior
2. Caesarean section:
- Placenta praevia type 2 posterior, type 3, type 4
- Other indications for caesarean section
Complication of Placenta Praevia:
| A. Maternal- | a) During pregnancy:
b) During labour:
c) Puerperium:
|
| B. Fetal: | a) Low birth weight b) Birth asphyxia c) Intra-uterine death d) Birth injury e) Congenital malformation is three times more common |