Concept of Epilepsy – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Concept of Epilepsy
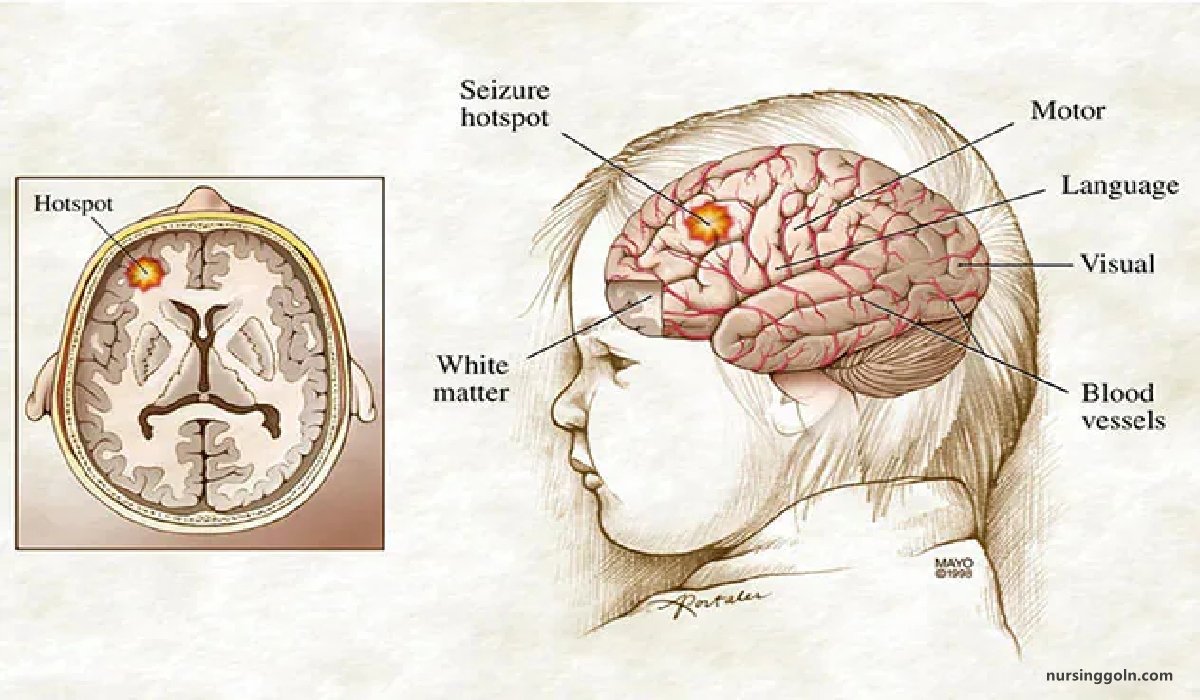
Epilepsy is a neurological condition (affecting the brain and nervous system) where a person has a tendency to have seizures that start in the brain.
The brain is made up of millions of nerve cells that use electrical signals to control the body’s functions, senses and thoughts. If the signals are disrupted, the person may have an epileptic seizure (sometimes called a ‘fit’ or ‘attack’).

Not all seizures are epileptic. Other conditions that can look like epilepsy include fainting (syncope) due to a drop in blood pressure, and febrile convulsions due to a sudden rise in body temperature when a young child is ill. These are not epileptic seizures because they are not caused by disrupted brain activity.
Definition of Epilepsy:
Epilepsy is recurrent, episodic, paroxysmal transient disturbances of brain function due to abnormal electrical activity of the neurons.
Or,
Epilepsy is recurrent seizure for which there is no immediate precipitating cause,
Classification of Epilepsy:
A. Generalized Seizures
a) Tonic-clonic seizures (Grand mal)
b) Absence seizures:
- Typical (petit mal)
- Atypical
c) Atopic seizures (drop attacks)
d) Myoclonic seizures.
B. Partial Seizures
a) Simple partial seizures (with elementary symptoms and no impaired consciousness)
- With motor signs (Jacksonians or focal motor).
- With somatosensory or special sensory i.e’ visual or auditory.
- With autonomic manifestations (abdominal epilepsy) no aton 1
b) Complex partial seizures-Manifested with impaired consciousness and with automatism. It includes psychomotor or temporal lobe seizures.
Epileptic syndrome:
Epileptic syndrome is a syndrome where epilepsy is a prominent feature.
Causes of Epilepsy;
- Sequelae of any of the acute causes of seizures
- Cerebral malformations
- Metabolic diseases
- Degenerative brain diseases
- Neoplasms
- Genetic disorders
Stages of Epilepsy:
1. Aura: A tonic clonic seizure may be preceded by a partial seizure the ‘aura’.
2. Tonic phase: The patient then goes rigid and becomes unconscious, falling down heavily if standing and often sustaining injury. During this phase, respiration is arrested and central cyanosis may be witnessed.
3. Clonic phase; After a few moments, the rigidity is periodically relaxed, producing clonic jerks. During the attack, urinary incontinence may occur, as may tongue biting. A severely bitten, bleeding tongue after an attack of loss of consciousness is pathognomonic of a generalized seizure.
4. Postictal phase: The patient then gradually regains consciousness, but is in a confused and disorientated state for half an hour or more after regaining consciousness. Full memory function may not be recovered for softie hours. After a generalized seizure the patient usually feels terrible, may have a headache and will want to sleep.
Typical Grand Mal Seizure:
It is divided into several phases –
i. Prodromal phase:
- Lasting hours to days before attack.
- May warn the pt. that an attack is impending.
- May be change of mood such as irritability.
ii. Aura:
- It lasts for seconds to min.
- It is a warning sign for a coming attack.
- It is characterized by epigastric discomfort/olfactory hallucination before the onset of the attack.
- The aura may be somatic, psychic or autonomic.
iii. Tonic phase:
- Rapid discharging of motor cortex causes tonic contraction of all the musculature & pt. goes rigid.
- Rolling of the the eyeballs upwards & arm flexed & legs extended.
- Respiration is arrested & cyanosis may develop.
- Loss of consciousness lasts for 10-30 sec and
- there is a characteristic cry
iv. Clonic phase:
- This stage lasts for about 1-5 minutes.
- There is interrupted powerful jerking movement of the face, body & limb
- Clenching of the teeth with tongue biting and
- Frothing from the mouth, traction of head to one side and
- Urinary incontinence may occur.
v. Post-ictal phage:
- This stage lasts only a few minutes but may be prolonged for half an hour or more.
- The pt. is in a flaccid state which evolus into normal sleep
- After regaining consciousness pt. is confused and may suffer from headache.
Clinical Features of Epilepsy:
A. In an aura phase:
- A peculiar sensation with dizziness occurs in about one-third epileptic children before tonic-clonic seizure.
- It is a transitory premonitory symptom which the child may recognize as the impending convulsions and adopt measures for self-protection.
B. In tonic spasm phase:
- Entire body becomes stiff
- Face may become pale and distorted,
- Eyes fixed in one position,
- Back may be arched.
- Head turned to backward or in one side,
- Arms are usually flexed and hands are clenched.
- The child usually falls on the ground from standing or sitting position and may utter a peculiar piercing cry.
- The child loses consciousness and having frothy discharge from mouth due to inability
- to swallow the saliva.
- Due to spasm of respiratory muscles, there is ineffective breathing and cyanosis.
- Pulse may become weak and irregular.
C. In clonic phase:
- Rhythmic jerky movements due to alternating contractions of muscle groups following the tonic state.
- Usually start in one part and become generalized including the facial muscles.
- The child may pass stool and urine involuntarily and may have tongue or chick bite due to sudden forceful contraction of abdominal muscles and jaw.
D. In the postictal or postconvulsive state:
- The child is usually become sleepy
- Confused or exhausted or perform automatic actions and may complain headache.
Investigations of Epilepsy:
i. Epileptic nature of attacks:
- Ambulatory EEG Video telemetry
| Investigation of epilepsy: (Viva) i. EEG ii. CT/MRL |
ii. Types of epilepsy:
- Standard EEG Sleep EEG
- EEG with special electrodes.
iii. Structural lesion:
- CT MRI
iv. Metabolic disorder:
- Urea and electrolytes Blood glucose
- Liver function test
- Serum calcium, magnesium
v. Inflammatory or infective disorder:
- Full blood count, ESR, C-reactive protein
- Chest x-ray
- Serology for syphilis, HIV, collagen disease
- CSF examination,
Principle of Management of Epilepsy:
1. It is important to explain the nature & cause of seizures to patient & relatives.
2. Instruct relatives about first aid.
3. Immediate care:
a. Move the patient from danger (fire, water, machinery)
b. After convulsion cease (turn into recovery position)
- Ensure airway is clear.
- Don’t insert anything in mouth.
c. If convulsion >5 minutes persist or recur without regaining consciousness- summon urgent medical attention.
d. Do not leave alone until fully recovered.
4. Immediate medical attention:
- Ensure airway is patent
- O₂ to offset cerebral hypoxia.
- IV anticonvulsants-Diazepam 10 mg.
- Draw blood for anticonvulsants level.
- Investigate the cause
5. Long-term anti-convulsant drugs: If more than one seizure
- Carbamazipine – 200-2000 mg/day
- Sodium valproate-400-2500 mg/day
- Ethosuximide-500-1500 mg/day
- Phenytoin-150-350 mg/day
6. Advice to patient:
- Pt. of epilepsy should be employed in some form of work which should not endanger their lives.
- Should not be allowed to work near fire, machines or at light.
- Swimming, cycling or driving should be abandoned.
- Precipitating factors should be avoided.
Nursing Management of Epilepsy:
1. Administer anticonvulsant therapy as prescribed.
2. Protect the patient from injury during seizures.
3. Monitor the patient continuously during seizures.
4. If the patient is taking antiseizure medications, constantly monitor for toxic signs and symptoms such as slurred speech, ataxia, lethary, and dizziness.
5. Monitor the patient’s compliance with anticonvulsant drug therapy.
6. Teach the patient to take exact dose of medication at the times prescribed.
7. Encourage the patient to eat balanced, regular meals.
8. Advise the patient to be alert for odors that may trigger an attack.
9. Limit or avoid alcohol intake.
10. Encourage to have enough sleep to prevent attacks
11. Avoid restraining the patient during a seizure.
12. Loosen any tight clothing, and place something flat and soft, such as pillow, jacket, or hand, under his head.
13. Avoid any forcing anything into the patient’s mouth if his teeth is clenched.
14. Avoid using tongue blade or spoon during attacks which could lacerate the mouth and lips of displace teeth, precipitating respiratory distress.
15. Protect the patient’s tongue, if his mouth is open, by placing a soft object between his teeth.
16. Turn the patient’s head to the side to provide an open airway.
17. Reassure patient after the seizure subsides by telling him that he’s all right, orienting him to time and place, and informing that he’s had a seizure.
Diet Therapy for Epileptic Patient:
1. Ketogenic diet may be given to raise the seizure threshold with calculated amount of proteins and fats without carbohydrates.
2. This diet makes the child ketotic as fat is used for energy production rather than carbohydrate. It seems that ketones may inhibit the seizure.
3. The child should not be given IV fluid with dextrose and strict fluid restriction to be maintained.
