Concept of Meningitis – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Concept of Meningitis
Meningitis is an acute inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The most common symptoms are fever, headache, and neck stiffness. Other symptoms include confusion or altered consciousness, vomiting, and an inability to tolerate light or loud noises.
Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding. If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash.
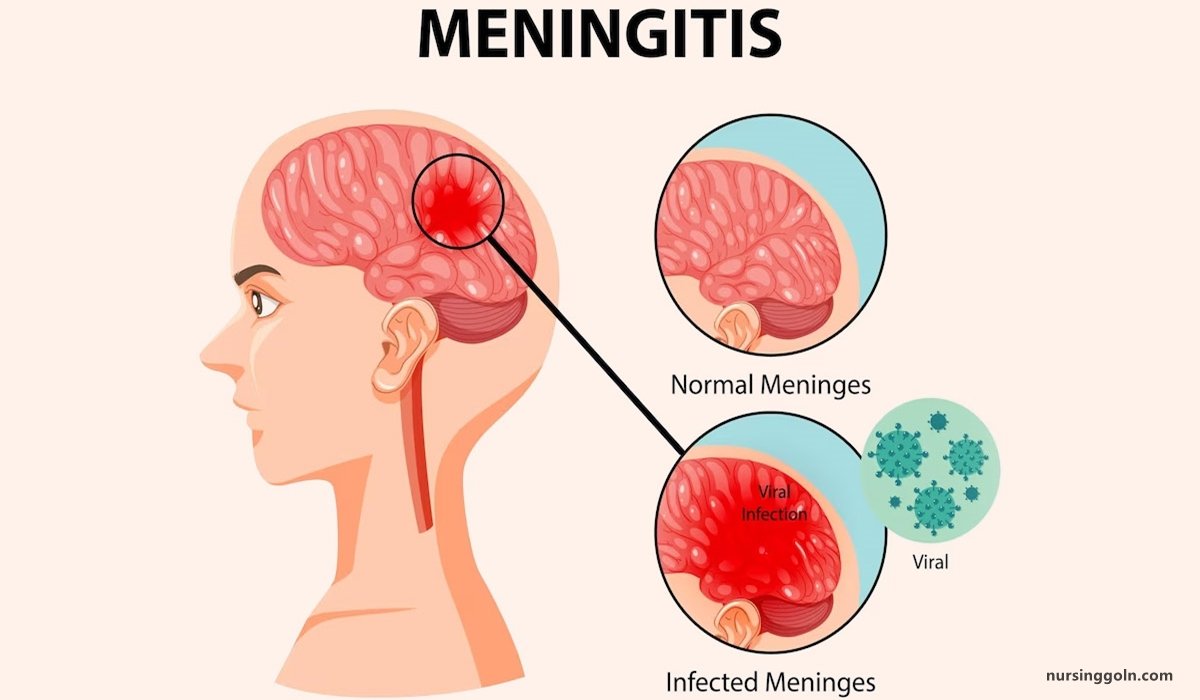
The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs. Meningitis can be life-threatening because of the inflammation’s proximity to the brain and spinal cord; therefore, the condition is classified as a medical emergency.
A lumbar puncture can diagnose or exclude meningitis. A needle is inserted into the spinal canal to collect a sample of cerebrospinal fluid (CSF) that envelops the brain and spinal cord. The CSF is examined in a medical laboratory.
Definition of Meningitis:
Meningitis refers to inflammation of the meninges overlying brain and spinal cord.
Or,
Inflammation of meninges overlying brain and spinal cord present with characteristic combination of pyrexia, headache
Causes of Meningitis:
A. Infective causes of meningitis
a) Bacterial causes
According to Age of Onset
| Age of onset | Common | Less common |
| A. Neonate |
|
|
| B. Pre-school child |
|
|
| C. Older child and adult |
| Listeria monocytogenes Mycobacterium tuberculosis Staphylococcus aureus (skull fracture) Haemophilus influenzae |
b) Viruses:
- Enteroviruses (echo, Coxsackie, polio)
- Mumps
- Influenza
- Herpes simplex
- Varicella zoster
- Epstein-Barr
- HIV
- Lymphocytic choriomeningitis
- Mollaret’s meningitis (HSV type 2)
c) Protozoa and parasites:
- Toxoplasma
- Amoeba
- Cysticercus
d) Fungi:
- Cryptococcus neoformans
- Candida
- Histoplasma
- Blastomyces
- Coccidioides
- Sporothrix
B. Non-infective (‘sterile’):
a) Malignant disease:
- Breast cancer
- Bronchial cancer
- Leukaemia
- Lymphoma
b) Inflammatory disease (may be recurrent):
- Sarcoidosis
- SLE
- Behçet’s disease
(Ref-Davidson’s Medicine/22nd/1205)
Types of Meningitis
| A. According to micro-organism: | a) Pyogenic or bacterial meningitis. b) Tuberculous meningitis. c) Viral meningitis. d) Fungal meningitis. |
| B. According to durations: | a) Acute meningitis b) Chronic meningitis |
| C. According to pus formation | a) Pyogenic or bacterial meningitis: Forms pus. b) Aseptic meningitis: (Tuberculosis meningitis. Viral meningitis. Fungal meningitis & parasite): Not form pus. c) Non-infective (‘sterile’) meningitis:
|
(Ref-Davidson’s Medicine/22nd/1202)
Pathophysiology of Meningitis
Meningococcal meningitis generally has a better prognosis than septicemia. Meningococci reach the brain from the bloodstream, implying that the patient’s immune response has prevented bacterial proliferation in the blood and not suffered overwhelming sepsis. This is because organisms are handled differently in these patients, which is probably due to differences in their inflammatory response to infection as well as different bacterial characteristics.
Deaths do occur, however due to the severity of the inflammatory process within the brain.
Once bacteria penetrate the blood-brain barrier, endotoxin and inflammatory mediators initiate a CSF inflammatory response, causing leakage of protein and fluid out of the cerebral vasculature. In addition, the processes delineated in septicemia occur in brain blood vessels, causing cerebral oedema and cerebral vascular thrombosis.
As a consequence there is an increase in brain water content and an increase in intracranial pressure. Both the increased pressure and thrombosis may lead to a reduction in cerebral perfusion, and consequently cerebral infarction and sometimes brain death
Pathogenesis of Bacterial Meningitis
From infection in the ear or skull fracture or sinus or from other bacteraemic illness
↓
Leptomeninges
↓
Congested and infiltrated with inflammatory cells
↓
A thin layer of pus forms and this may later organise to form adhesions
↓
Obstruction to the free flow of CSF leading to hydrocaphalus and produces other signs-symptoms of meningitis.
Management of Pyogenic/ Bacterial Meningitis:
Clinical Features of Bacterial Mening’itis:
a) New born:
- Vacant stare
- Fever/hypothermia
- Drowsiness/ irritability
- Vomiting
- Reluctance to feed
- Poor tone and poor cry
- Convulsion
- Fontanelle may bulge
- Kernig’s sing may present
- Neck rigidity absent
b) Older and adult:
- Headache
- Drowsiness
- Fever
- Vomiting
- Restlessness
- Irritability
- Coma, convulsion
- Cranial nerve palsies
- Neck rigidity, kernig’s sing and Brudzinskis sign may be positive
Investigations:
- CSF study, cytology, biochemistry, gram stain, culture
- Serological tests
- Cranial ultrasound scan when fontanels are patient (up to 18 month)
- Blood for CBC & C/S
- CT scan to exclude more lesion: cerebral abscess
Treatment of Mening’itis
A. In 1st 3 months of life
a) Inj. ampicillin (400 mg/kg/day I/V, 4 divided doses) plus.
b) Inj. cefotaxime (200 nag/kg/day, 4 divided dose I/V) or
c) Inj. ceftriaxone (100 mg/kg/day once daily I/V).
B. Beyond 3 months of age:
a) Inj. Ampicillin Inj. plus chloramphenicol (100 mg/kg/day, 4 divided dose VV or I/M).
b) Inj crystalline penicilin (300,00 U/kg/24hr) for 5-7 day is the treatment complicated meningucoccal mening-itis.
c) Duration of therapy for mening-itis is generally 10-14 day (or 14-21 days in Gram negative bacillus infection).
C. Anti-inflammatory therapy
a) IV dexamethasone in a dose 0.15 mg/kg/dose given I/V hrly for 2 days.
b) It should be given 15 min before antibiotic treatment.
D. Symptomatic treatment
a) Parcetamol
b) Per rectally diazepam (0 5 mg/kg/dose)
c) Subsequently phenytoin 15-20 mg/kg loading dose followed by 5 mg/kg/24hrs as maintenance dose car be used.
E. Treatment of complications:
a) Increased intracranial pressure can be treated with intravenous mannitol (0.5
b) mg/kg/IV infusion) and intravenous furosemide.
e) Shock should be treated with volume expander.

(Ref by- M. R. Khan 4th)
Complication of Meningitis:
A. Immediate:
- Increase intracranial pressure (ICP)
- Cranial nerve palsies
- Cerebral or cerebellar herniation
- Subdural effusion
- Empyema
- Hydrocephalus
- SIADH
- Shock DIC
- Brain abscess
B. Late:
- Permanent brain damage
- Cerebral palsy
- Mental retardation
- Epilepsy
- Deafness
- Hydrocephalus
Differentiating Features of Different Meningitis:
| Traits | Normal findings | Acute bacterial mening-itis | Viral meningitis | Tuberculous meningitis |
| A. Pressure | 50-180 mm of water | Normal /increased | Normal | Normal/increased |
| B. Colour | Clear | Cloudy | Clear | Clear/cloudy/Spider web/fine clot |
| C. Red cell count | 0-4 ×106/1 | Normal | Normal | Normal |
| D. White cell count | 0-4×106/1 | 1000-5000 polymorphs | 10-2000 lymphocytes | 50-5000 lymphocytes |
| E. Glucose | > 60% of blood level | Decreased | Normal | Decreased |
| F. Protein | <0.45 g/1 | Increased | Normal/increased | Increased |
| G. Oligoclonal bands | Negative | Can be positive | Can be positive | Can be positive |
Nursing Management of Meningitis:
Nursing management of the patient with mening-itis include the following:
Nursing Assessment
Assessment of the patient with bacterial mening-itis include.
- Neurologic status. Neurologic status and vital signs are continually assessed.
- Pulse oximetry and arterial blood gas values. These values are used to quickly identify the need for respiratory support.
Nursing Diagnosis
Based on the assessment data, major nursing diagnoses include:
- Risk for Infection related to contagious nature of organism.
- Acute Pain related to headache, fever, neck pain secondary to meningeal irritation.
- Impaired Physical Mobility related to intravenous infusion, nuchal rigidity and restraining devices.
- Activity Intolerance related to fatigue and malaise secondary to infection.
- Risk for Impaired Skin Integrity related to immobility, dehydration, and diaphoresis.
- Risk for Injury related to restlessness and disorientation secondary to meningeal irritation.
- Interrupted Family Process related to critical nature of situation and uncertain prognosis.
- Anxiety related to treatment and risk of death.
- Risk for Ineffective Therapeutic Regimen Management
Nursing Care Planning & Goals
Goals for a patient with bacterial mening-itis include:
- Protection against injury.
- Prevention of infection.
- Restoring normal cognitive functions.
- Prevention of complications.
Nursing Interventions
Important components of nursing care include the following measures:
- Assess neurologic status and vital signs constantly. Determine oxygenation from arterial blood gas values and pulse oximetry.
- Insert cuffed endotracheal tube (or tracheostomy), and position patient on mechanical ventilation as prescribed.
- Assess blood pressure. (Usually monitored using an arterial line) for incipient shock, which precedes cardiac or respiratory failure.
- Rapid IV fluid replacement may be prescribed, but take care not to overhydrate patient because of risk of cerebral edema.
- Reduce high fever to decrease load on heart and brain from oxygen demands.
- Protect the patient from injury secondary to seizure activity or altered level of consciousness (LOC).
- Monitor daily body weight; serum electrolytes; and urine volume, specific gravity, and osmolality, especially if syndrome of inappropriate antidiuretic hormone (SIADH) is suspected.
- Prevent complications associated with immobility, such as pressure and pneumonia.
- Institute infection control precautions until 24 hours after initiation of antibiotic therapy (oral and nasal discharge is considered infectious).
- Inform family about patient’s condition and permit family to see patient at appropriate intervals.
Evaluation
Expected patient outcomes include:
- Avoidance of injury.
- Avoidance of infection.
- Restoration of normal cognitive functions.
- Prevention of complications.