Concepts of Pneumonia – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Concepts of Pneumonia
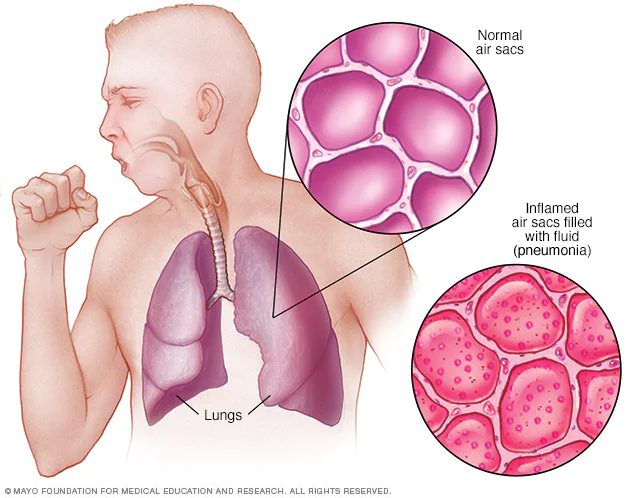
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia.
Pneumonia can range in seriousness from mild to life-threatening. It is most serious for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
Definition of Pneumonia
Pneumonia can be defined as any infection in the lungs parenchyma.
Or
Pneumonia can be defined as an acute respiratory illness associated with recently developed radiological pulmonary shadowing which may be segmental lobar or multi-lobar.
Or
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing.
(Ref by-Davidsons Medicine/22nd/682)
Classification/ Causes of Pneumonia
A. Anatomical, clinical and radiographic presentation.
a) Lobar pneumonia: consolidation of a large portion or entire lobe of lung.
b) Bronchopneumonia: Patchy consolidation in lung. atypical pneumonia
B. Clinical classification:-
a) Community acquired pneumonia-
b) Hospital acquired pneumonia
c) Pneumonia in immune-compromised hosts
d) Pneumonia in damaged lung

C. Aetiological classification:
1) Infective
a) Bacterial
- Pneumoccoci
- Staphylococcus aureus
- Streptococcus pyogens
- Haemophilus Influenza
- Mycoplasma pneumoneae
- Klebsiella Pneumonia
- M. Tuberculosis
b) Viral
- Respiratory syncytial virus
- Influenza and Para influenza
- Cytomegalo virus
- Measles virus
- Mumps virus
- Rhino virus
- Adeno virus
c) Fungal: Candida, Actinomycosis, and Histoplasma.
d) Protozoal: E. histolytica, Toxoplasma gondii, Pneumocystitis carinii.
e) Mycoplasmal: M. Pneumonia
f) Chlamydial: C. Psittaci
g) Ridkettsial: Typhus and Q-fever
2) Allergic: Collagen vascular disease
3) Chemical agents: fumes, gas
4) Physical: Irradiation
D. Clinical classification of pediatrics:
a) 2 month to 5 years
- very severe disease
- severe pneumonia
- pneumonia
- No pneumonia: Cough and cold
b) Less than 2 month
- very severe disease
- severe pneumonia
- No pneumonia: Cough and Col

(Ref by-Davidsons Medicine/22nd/683)
Another Answer
Causes of Pneumonia
| Age group | Organism |
| Neonatal period |
|
| Post neonatal period |
|
| Beyond 5 years |
|
Classification of Severity of Pneumonia According to WHO:
| Sign or symptoms | Classification | Treatment |
| Severe pneumonia or Very severe pneumonia |
|
| Pneumonia |
|
| No pneumonia Cough or |
|
(Ref by: WHO)
Clinical Features of Pneumonia:
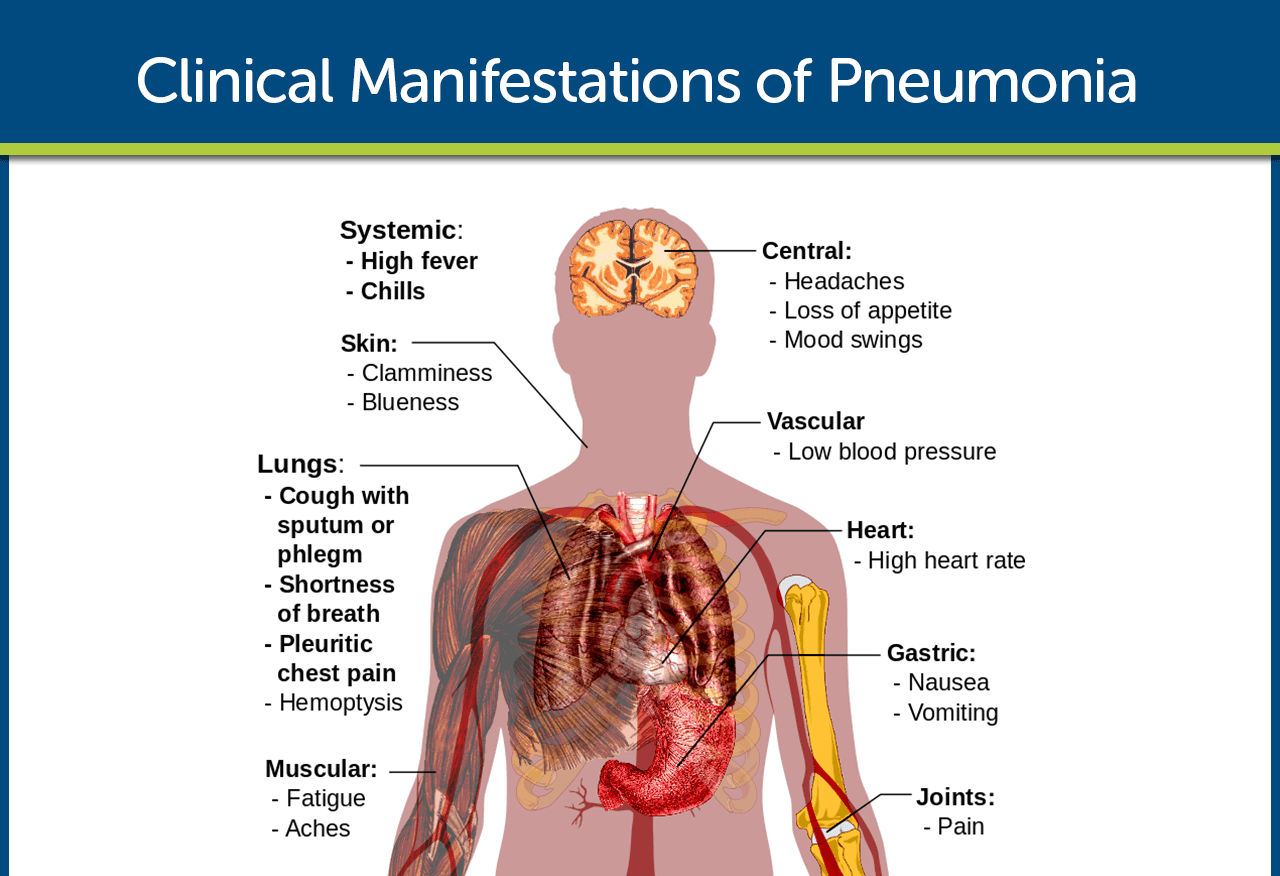
A. Symptoms
a) Fever
- Sudden onset
- High fever
- Usually associated with rigor & vomiting.
b) Chest pain
- Pleuritic chest pain.
- Occasionally referred to the shoulder or anterior abdominal wall.
- c) CoughShort, painful.
- At first dry.
- Later become productive and may become rust coloured or even frankly blood stain
d) Dyspnoea
e) Loss of appetite & headache
B. Signs
a) Tachycardia,
b) Pyrexia,
c) Tachypnea,
d) Cyanosis,
e) Hypotension,
f) Confusion
Diagnosis of Pneumonia:
Routine examination (R/E)
- a) InspectionRespiratory rate in increased
- Respiratory movement is diminished on the affected side
b) Palpation
- Trachea-central, may be shifted to the opposite side (in pleural effusion) A
- Apex beat-normal in position, may be shifted to the opposite site
- Chest walls movement is diminished on the affected side
c) Percussion
- Woody dull in case of consolidation
- Stony dull in case of pleural effusion
d) Auscultation
- Breath sound is high pitched bronchial in consolidation and diminished
- Vocal resonance is increased in consolidation and diminished or absent in pleural effusion.
- Fine crepitation early and coarse crepitation in resolution phase
Investigation
a) Blood: TC, DC, ESR, and culture sensitivity test.
b) Sputum
- Gram stain – Gram positive diplococci
- culture and sensitivity-pneumococcus can be isolated
c) Chest X-ray test
d) Serological test – To detect the pneumococcal antigen.
(Ref by- Kumar & Clark clinical Medicine/7th +Harrison’s internal medicine/17th + short case Abdullah Sir 4 +Davidson’s Medicine 683-85/224)
Management of Pneumonia
1. Refer urgently to hospital.
2. Start first dose of an antibiotic.
3. Rx of fever-if fever is high (>39°C): Paracetamol)
4. Rx of wheeze: Rapid acting bronchodilator – Salbutamol
5. Antibiotic therapy (duration 10 days):
| For age 2 months to 5 years | Less than 2 month |
| Inj. Ampicillin | Inj. Ampicillin+ Inj. Gentamicin. |
Treatment of pneumonia of for age 2 months to 5 years:
1. Advice the mother on home care:
a) Feed the child:
- Feed the child during illness.
- Increases feeding after illness
- Clear the nose if it interferes with feeding.
b) Increase fluids:
- Offer the child extra to drink.
- Increases breast feeding.
c) Sooth the throat & relieve the cough with a safe remedy (like honey, lemon juice)
d) Give referral knowledge to mother: Return the child when
- Breathing becomes fast.
- Breathing becomes difficult.
- Not able to drink.
- Child becomes sicker.
2. Antibiotic therapy for. 5 days duration- Any one of the following can be given.
- Cotrimoxazole – two times daily for 5 days (oral)
- Amoxicillin – three times daily for 5 days (oral)
- Ampicillin – four times daily for 5 days (oral)
3. Treatment of fever –
- If high (> 39°c)) paracetamol
- If not high (38°C-39°C) – Advice the mother to give more fluid.
- Fever for more than five days: refer for assessment.
4. Rx of wheezing: oral salbutamol
5. Advice the mother to return the child in 2 days for reassessment or earlier if the condition getting
Treatment of No pneumonia:
1. Advice the mother on home care:
a) Feed the child:
- Feed the child during illness.
- Increases feeding after illness.
- Clear the nose if it interferes with feeding.
b) Increase fluids:
- Offer the child extra to drink.
- Increases breast feeding.
c) Sooth the throat & relieve the cough with a safe remedy (like honey, lemon juice)
d) Give referral knowledge to mother: Return the child when
- Breathing becomes fast.
- Breathing becomes difficult.
- Not able to drink.
- Child becomes sicker.
2. No antibiotics.
3. Rx of fever.
4. Rx of wheeze.
5. If coughing more than 30 days- refer for assessment. 6. Assess & treat ear problem/sore throat, if any.
7. Assess & treat other problems, if any.
(Ref- M. R. Khan 4th/edition)
FOR SAQ
1. Specific: Antimicrobial therapy.
2. Supportive:
- O2 inhalation.
- Hydration (fluid may be restricted, considering SIADH).
- Nutrition.
- Antipyretics.
- Bronchodilators.
- Physiotherapy.
(Ref by- Kumar & Clark clinical Medicine /7th+Davidson’s Medicine 683-85/22)
Nursing Management of Pneumonia
A. To improve airway patency
a) Removal of secretions. Secretions should be removed because retained secretions
interfere with gas exchange and may slow recovery.
b) Adequate hydration of 2 to 3 liters per day thins and loosens pulmonary secretions.
c) Humidification may loosen secretions and improve ventilation.
d) Coughing exercises. An effective, directed cough can also improve airway patency.
e) Chest physiotherapy. Chest physiotherapy is important because it loosens and mobilizes secretions.
B. To promote rest and conserve energy
a) Encourage avoidance of overexertion and possible exacerbation of symptoms.
b) Semi-Fowler’s position. The patient should assume a comfortable position to promote rest and breathing and should change positions frequently to enhance secretion clearance and pulmonary ventilation and perfusion.
C. To promote fluid intake
a) Fluid intake. Increase in fluid intake to at least 2L per day to replace insensible fluid losses.
D. To maintain nutrition
a) Fluids with electrolytes. This may help provide fluid, calories, and electrolytes.
b) Nutrition-enriched beverages. Nutritionally enhanced drinks and shakes can also help restore proper nutrition.
E. To promote patient’s knowledge
a) Instruct patient and family about the cause of pneumonia, management of symptoms, signs, and symptoms, and the need for follow-up.
b) Instruct patient about the factors that may have contributed to the development of the disease.
Factors That Predispose to Pneumonia
1. Upper respiratory tract infection
2. Alcohol
3. Cigarette smoking
4. Corticosteroid therapy
5. Old age
6. Recent influenza infection
7. Indoor air pollution
8. AIDS
9. Preexisting lungs disease
Pathophysiological Condition of Pneumonia
(Ref by-Davidsons Medicine/22nd/682)
Having an idea about the disease process helps the patient understand the treatment regimen and its importance, increasing patient compliance.
➤ Pneumonia arises from normal flora present in patients whose resistance has been altered or from aspiration of flora present in the oropharynx.
➤ An inflammatory reaction may occur in the alveoli, producing exudates that interfere with the diffusion of oxygen and carbon dioxide.
➤White blood cells also migrate into the alveoli and fill the normally air-filled spaces.
➤Due to secretions and mucosal edema, there are areas of the lung that are not adequately ventilated and cause partial occlusion of the alveoli or bronchi.
➤Hypoventilation may follow, causing ventilation-perfusion mismatch.
➤Venous blood entering the pulmonary circulation passes through the under ventilated areas and travels to the left side of the heart deoxygenated.
➤ The mixing of oxygenated and poorly oxygenated blood can result to arterial hypoxemia.
Complications of Pneumonia:
- Pleural effusion.
- Empyema.
- Septicemia.
- Bacteremia.
- Collapse.
- Lung abscess.
- Bronchiectasis.
- Subcutaneous emphysema.
- Metastatic spread: Meningitis, septic arthritis. Osteomyelitis etc.
Prevention of Pneumonia:
➤ Preventing pneumonia in children is an essential component of a strategy to reduce child
mortality.
➤ Immunization against Hib, pneumococcus, measles and whooping cough (pertussis) is the most effective way to prevent pneumonia.
➤ Adequate nutrition is key to improving children’s natural defenses, starting with exclusive breastfeeding for the first 6 months of life.
➤ In addition to being effective in preventing pneumonia, it also helps to reduce the length of the illness if a child does become ill.
➤ Addressing environmental factors such as indoor air pollution (by providing affordable clean indoor stoves, for example) and encouraging good hygiene in crowded homes also reduces the number of children who fall ill with pneumonia.
➤In children infected with HIV, the antibiotic cotrimoxazole is given daily to decrease the risk of contracting pneumonia.

(Ref by-https://www.who.int/news-room/fact-sheets/detail/pneumonia)
Another Answer:
➤ Get vaccinated: Vaccines are available to prevent some types of pneumonia and the flu Talk with doctor about getting these shots. The vaccination guidelines have changed over time so make sure to review vaccination status with doctor even if you recall previously receiving a pneumonia vaccine.
➤Make sure children get vaccinated: Doctors recommend a different pneumonia vaccine for children younger than age 2 and for children ages 2 to 5 years who are at particular risk of pneumococcal disease. Children who attend a group child care center should also get the vaccine. Doctors also recommend flu shots for children older than 6 months.
➤ Practice good hygiene: To protect yourself against respiratory infections that sometimes lead to pneumonia, wash hands regularly or use an alcohol-based hand sanitizer.
➤ Don’t smoke. Smoking damages lungs’ natural defenses against respiratory infections.
➤ Keep immune system strong: Get enough sleep, exercise regularly and eat a healthy diet.