Copncept About Mucolytics – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination setup according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Copncept About Mucolytics
Drug Affecting Respiratory System
Basic Concepts
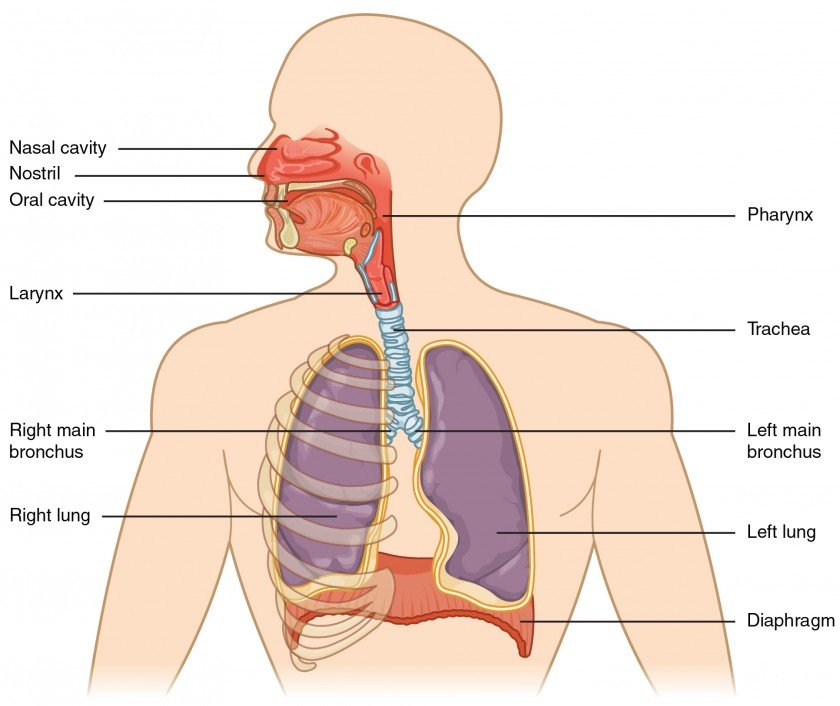
Respiration is the process of exchange of oxygen and carbon dioxide between an organism and its external environment. This principally involves the lungs, which possess the largest surface area in the body in contact with the external environment. The respiratory system has defense mechanisms which can be divided into physical (such as coughing or the mucociliary escalator, to remove foreign agents) and immunological (such as enzymes, pulmonary macrophages and lymphoid tissue, to ‘disarm’ foreign agents). These defense mechanisms can be launched inappropriately or may be insufficient to deal with the triggering agent, and thus disease may occur.
Diseases of Respiratory System
Cough
Cough is a protective reflex, its purpose being expulsion of respiratory secretions or foreign particles from air passages. It occurs due to stimulation of mechanic or chemoreceptors in throat, respiratory passages or stretch receptors in the lungs. Cough may be useful or useless. Useless (nonproductive) cough should be suppressed.
Useful (productive) cough serves to drain the airway, its suppression is not desirable, may even be harmful, except if the amount of expectoration achieved is small compared to the effort of continuous coughing.
Causes of cough:
- Chronic bronchitis
- Asthma (productive cough)
- Bronchogenic carcinoma
- Tuberculosis (TB)
- Bronchiectasis and lung abscess
Apart from specific remedies (antibiotics, etc. see box), cough may be treated as a symptom (nonspecific therapy) with:
1. Pharyngeal demulcents Lozenges, cough drops, linctus’s containing syrup, glycerin, liquorice.
2. Expectorants (Mucokinetics)
(a) Bronchial secretion enhancers: Sodium or Potassium citrate, Potassium iodide, Guaiphenesin (Glyceryl guaiacolate), balsum of Tolu, Vasaka, Ammonium chloride.
(b) Mucolytics: Bromhexine, Ambroxol, Acetyl cysteine, Carbocisteine
3. Antitussives (Cough centre suppressants)
a. Opioids: Codeine, Ethylmorphine, Pholcodeine.
b. Nonopioids: Noscapine, Dextromethorphan, Chlophedianol.
c. Antihistamines: Chlorpheniramine, Diphenhydramine, Promethazine.
d. Peripherally acting: Prenoxdiazine.
4. Adjuvant antitussives Bronchodilators: Salbutamol, Terbutalin.
Mucolytics
Bromhexine:
A derivative of the alkaloid vasicine obtained from Adhatoda vasica (Vasaka), is a potent mucolytic and mucokinetic, capable of inducing thin copious bronchial secretion. It depolymerises mucopolysaccharides directly as well as by liberating lysosomal enzymes- network of fibres in tenacious sputum is broken. It is particularly useful if mucus plugs are present.
Side effects are rhinorrhoea and lacrimation, nausea gastric irritation, hypersensitivity. Dose: adults 8 mg TDS, children 1-5 years 4 mg BD, 5-10 years 4 mg TDS, BROMHEXINE 8 mg tablet, 4 mg/5 ml elixir.

Ambroxol: A metabolite of bromhexine having similar mucolytic action, uses and side effects. Dose: 15-30 mg TDS.
Acetylcysteine: It opens disulfide bonds in mucoproteins present in sputum-makes it less viscid, but has to be administered directly into the respiratory tract.
Carbocisteine: It liquefies viscid sputum in the same way as acetylcysteine and is administered orally (250-750 mg TDS). Some patients of chronic bronchitis have been shown to benefit. It may break gastric mucosal barrier; is contraindicated in peptic ulcer patients. Side effects are gastric discomfort and rashes.
Antitussives
These are drugs that act in the CNS to raise the threshold of cough center or act peripherally in the respiratory tract to reduce tussal impulses, or both these actions. Because they aim to control rather than eliminate cough, antitussives should be used only for dry nonproductive cough or if cough is unduly tiring, disturbs sleep or is hazardous (hernia, piles, cardiac disease, ocular surgery).
Classification anti-tussives:-
a) Peripherally acting anti tussives.
- Linctuses
- Water aerosol inhalation
- Benzoin inhalation
- Methanol and eucalyptus
b)Centrally acting anti-tussive

1. Opioid derivatives (addicting powerful respiratory depretion). Eg,
- Morphine
- Diamorphine
- Methadone
2. Opioid analgesics (non-addiction, less respiratory depression)
- Codeine
- Pholcodine
3. Sedative antihistamines (sedation reduces cough)mo) dos
- Diphenhydramine
- Chlorpheniramine
Opioids
Codeine:
An opium alkaloid, qualitatively similar to and less potent than morphine, but is more selective for cough centre. Codeine is regarded as the standard antitussive; suppresses cough for about 6 hours.
The antitussive action is blocked by naloxone indicating that it is exerted through opioid receptors in the brain. Abuse liability is low, but present; constipation is the chief drawback. At higher doses respiratory depression and drowsiness can occur, especially in children. Driving may be impaired. Like morphine, it is contraindicated in asthmatics and in patients with diminished respiratory reserve; should be avoided in children.
Dose: 10-30 mg; children 2-6 years 2.5-5 mg, 6-12 years 5-10 mg, frequently used as syrup codeine phos. 4-8 ml.
Ethylmorphine:
It is closely related to codeine which is methylmorphine, and has antitussive, respiratory depressant properties like it, but is believed to be less constipating. Dose: 10-30 mg TDS
Nonopioids
Noscapine (Narcotine):
An opium alkaloid of the benzoisoquinoline series (see Ch. 34). It depresses cough but has no narcotic, analgesic or dependence inducing properties. It is nearly equipotent antitussive as codeine, especially useful in spasmodic cough. Headache and nausea occur occasionally as side effect. It can release histamine and produce bronchoconstriction in asthmatics.
Dose: 15-30 mg, children 2-6 years 7.5 mg, 6-12 years 15 mg.
Dextromethorphan:
A synthetic central NMDA (N-methyl D-aspartate) receptor antagonist; the d-isomer has antitussive action while /-isomer is analgesic. Dextromethorphan does not depress mucociliary function of the airway mucosa and is practically devoid of constipating action. Though considered non-addicting, some drug abusers indulge in it. The antitussive action of dextromethorphan has been rated equivalent to codeine, but some clinical studies have found it
to be no better than placebo.
- Side effect: Dizziness, nausea, drowsiness; at high doses hallucinations and ataxia may occur.
- Dose: 10-20 mg, children 2-6 years 2.5-5 mg, 6-12 years 5-10 mg. It is a common ingredient of many proprietary cough formulations (see antitussive combinations below).bs2
Chlophedianol:
It is a centrally acting antitussive with slow onset and longer duration of action.
- Side effect: Dryness of mouth, vertigo, irritability.
- Dose: 20-40 mg

Obstructive Airways Disease
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is a chronic and progressive disease with fixed or poorly reversible airflow obstruction. It encompasses several disease components, namely chronic bronchitis and bronchiolitis, consisting of inflammation and mucus hyper secretion and emphysema, involving destruction of alveolar walls. Long-term smoking is the leading factor in the development of COPD. Cigarette smoke activates inflammatory cells (mainly macrophages and neutrophils), which can cause connective tissue damage in the lung parenchyma, resulting in emphysema and hyper secretion of mucus.
al-Antitrypsin is a protease inhibitor, deficiency of which can result in decreased inhibition of proteases released by neutrophils, thus predisposing to destruction of lung tissue leading to emphysema. Other factors, such as atmospheric pollution, can also have causal links. Patients with COPD experience cough with the production of sputum, wheeze and breathlessness. Infective exacerbations can occur, giving purulent sputum.
Asthma
Asthma is a chronic inflammatory disease of the bronchiolar airways. It is characterized by recurrent reversible obstruction to airflow causing airflow limitation, airway hyperresponsiveness and inflammation of the bronchi. Asthma may be allergic (extrinsic) or non-allergic (intrinsic).
In asthma, smooth muscle that surrounds the bronchi is hyperresponsive to stimuli, and underlying inflammatory changes are present in the airways. Asthmatic stimuli include inhaled allergens (e.g. pollen, animal dander), occupational allergens, and drugs or non-specific stimuli such as cold air, exercise, stress and pollution.
The stimuli cause asthmatic changes through several complex pathways. The possible mechanisms of these pathways include the following:
1. Immune reactions (type 1 hypersensitivity) and release of inflammatory mediators: the cross-linking of IgE by allergens causes mast cell degranulation which releases histamine, eosinophilic and neutrophilic chemotactic factors. The eosinophils, neutrophils and other inflammatory cells release inflammatory mediators that cause a bronchial inflammatory reaction, tissue damage and an increase in bronchial hyperresponsiveness. Bronchial inflammatory mediators include leukotrienes, prostaglandins, thromboxane, platelet-activating factor and eosinophilic major basic protein.
2. An imbalance in airway smooth muscle tone involving the parasympathetic nerves (vagus), non-adrenergic non-cholinergic (NANC) nerves and circulating noradrenaline that act under normal circumstances to control airway diameter.
3. Abnormal calcium flux across cell membranes, increasing smooth muscle contraction and mast cell degranulation. Leaky tight junctions between bronchial epithelial cells allowing allergen access. phase response. Immediate-phase response
4. The above result in symptoms of wheezing, breathlessness and sometimes cough. In many people the asthmatic attack consists of two phases: an immediate-phase response and a late- An immediate-phase response occurs on exposure to the eliciting stimulus. The response consists mainly of bronchospasm. Bronchodilators are effective in this early phase. Late-phase response ck to back Several hours later, the late-phase response occurs. This consists of bronchospasm, vasodilatation, oedema and mucus secretion caused by inflammatory mediators released from cosinophils, platelets and other cells, and neuropeptides released by axon reflexes. Anti- inflammatory drug action is necessary for the prevention and/or treatment of this phase.
Communication
Children with asthma who are very young can have difficulty using inhalers or nebulizers, and it is therefore more effective to give them theophylline, as this can be given in tablet form. Zara is a 4-year-old girl who is on theophylline for this reason. Zara presents to accident and emergency (with her mother) in pain, distress and with pyrexia (a high temperature). She is found to have an infection. Should she be given erythromycin as normal?
No! Theophylline plasma concentrations would increase because enzymes involved in its breakdown would be occupied with erythromycin as well. Theophylline has a very narrow therapeutic range and so small increases above the therapeutic dose can be toxic and even fatal.
Management of Obstructive Airways Disease
Anti-asthmatic drugs include symptomatic bronchodilators (these are most effective in the immediate-phase response), and prophylactic or anti-inflammatory agents, which prevent and/or resolve the late-phase response. The step-wise management of asthma is summarized in the stage-dependent treatment of COPD.
Most patients with COPD get some symptom relief from bronchodilators and anti-inflammatory agents in a fashion similar to people with asthma, yet the response of their airways to these drugs is much less marked, and there are no proved benefits for life expectancy. Long-term oxygen therapy does prolong survival in patients with COPD; however, this must be undertaken with care in patients with carbon dioxide retention because it will reduce their hypoxic drive to breathe.
Classification of drugs used in asthma.
| A. Bronchodilator a. Beta agonist:
b. Xanthine derivatives:
c. Anti-cholinergic bronchodilator:
d. Antihistamines:
| B. Anti-inflammatory agents ➤ Steroids:
➤ Mast cell stabilizers, eg
➤Leukotriene antagonists:
|