Cord Prolapse – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Cord Prolapse
Cord prolapse:
Cord prolapsed/umbilical cord prolapsed is a complication that occurs prior to or during the delivery of the baby. In a prolapse the umbilical cord drops through the open cervix into the vagina ahead of the baby.
Cord presentation:
Cord presentation is the presence of the umbilical cord between the fetal presenting part and the cervix, with or without membrane rupture. The overall incidence of cord prolapse ranges from 0.1% to 0.6%.

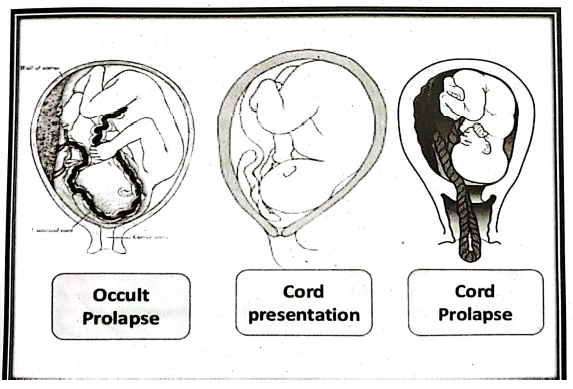
Types of cord prolapsed:
A. Occult cord prolapse
- Cord is adjacent to the presenting part
- Cannot be palpated during pelvic examination.
- Might lead to variable decelerations or unexplained fetal distress.
B. Funic (cord) presentation
- Prolapse of the umbilical cord below the level of the presenting part before the rupture of fetal membranes
- Cord can often be easily palpated through the membranes
- Often the harbinger of cord prolapse
C. Overt cord prolapse
- Umbilical cord lies below the presenting part
- Associated with rupture of membranes, and displacement of the cord through the vagina.
Causes of cord prolapsed:
The most common cause of an umbilical cord prolapse is a premature rupture of the membranes that contain the amniotic fluid. Other causes include:
➤ Premature delivery of the baby.
➤ Delivering more than one baby per pregnancy (twins, triplets, etc.).
➤ Excessive amniotic fluid..
➤ Breech delivery (the baby comes through the birth canal feet first).
➤ An umbilical cord that is longer than usual.
Predisposing factors of cord prolapsed:
Risk factors of cord prolapsed:
➤ Fetal congenital abnormality.
➤ Second twin.
➤ Prematurity
➤ Multiparity.
➤ Low birth weight (<2.5 kg).
➤ Breech.
➤ Oblique, transverse and unstable lie.
➤ Cephalopelvic disproportion.
➤ Pelvic tumours.
➤ Low-lying placenta.
➤ Polyhydramnios.
➤ Macrosomia.
➤ High fetal station.
➤ Long umbilical cord.
➤ Obstetric interventions including:
✓ Amniotomy with high presenting part.
✓ Vaginal manipulation of the fetus with ruptured membranes.
✓ Insertion of intrauterine pressure catheter.
✓ Attempted external cephalic or internal podalic version.
Clinical features of cord prolapsed:
➤ Usually sudden decrease fetal heart rate.
➤ Fetal heart tracing.
➤ The cord can be seen or felt on vaginal examination.
➤ Prolapsed of the cord can occur at any time after rupture of membrane.
➤ Patient reports feeling of cord within the vagina.
➤ Sometimes she present with cord-prolapsed.
➤ The fetal heart rate usually drops precipitously.
Management of cord prolapsed:
Treat a prolapsed cord as an acute obstetric emergency.
With an overt prolapse:
➤ Administer oxygen to the woman 4-6 L/minute.
➤ If the fetus is viable, place the mother in the knee-chest position (patient facing the bed,
chest level to bed, knees tucked under chest, pelvis and buttocks elevated) or head-down tilt in the left lateral position and apply upward pressure against the presenting part to lift the fetus away from the prolapsed cord. This can be done manually or by filling the urinary bladder.
➤ Manual replacement of the prolapsed cord above the presenting part is not currently recommended.
➤ Avoid handling the cord outside the vagina, as this induces vasospasm.
➤ Proceed to emergency caesarean section as soon as possible.
➤ If available, give terbutaline 0.25 mg subcutaneously to reduce contractions when there are persistent fetal heart rate trace abnormalities, despite attempts to prevent cord compression manually, and there may be delays in achieving delivery.
➤ Only proceed with vaginal delivery if delivery is imminent, the cervix is fully dilated and there are no contra-indications.
➤ This can be expedited with episiotomy/vacuum extraction or forceps.
➤ Ensure resuscitation is available for the baby post-delivery.
➤ If the fetus has died, deliver in the manner that is safest for the woman.
If an occult prolapse is suspected:
➤ Place the mother in the left lateral position.
➤ If the fetal heart rate returns to normal, allow labour to continue with the mother receiving O2 and fetal heart rate being continuously monitored.
➤ If the fetal heart rate remains abnormal, expedite a rapid caesarean section.
With funic presentation:
➤ A decision needs to be made between prompt elective caesarean section prior to membrane rupture or artificial rupture of membranes (ARM) with full preparations for an emergency caesarean section, in case the cord does become an overt prolapse on rupture.
In the community, cord-prolapse is associated with a ten-fold increase in perinatal mortality rate, compared with that occurring in hospital.
Emergency community management of cord prolapse:
➤ Arrange ambulance transfer to the nearest consultant-led obstetric unit for delivery, unless spontaneous vaginal delivery is assessed.
➤ Advise knee-chest, face-down position whilst awaiting the ambulance.
➤ Elevate the presenting part whilst awaiting transfer and during transfer to hospital.
➤ Use the left lateral position with pillow under hip for transfer in the ambulance.
Management of cord prolapse and cord presentation:
Diagnosis:
- It is diagnosed by vaginal examination. If the cord is prolapsed it is necessary to detect whether it is pulsating i.e. living foetus or not ie. dead foetus but this should be documented by auscultating the FHS.
- Ultrasound: occasionally can diagnose cord presentation.
Management:
A. Cord presentation:
Caesarean section: for contracted pelvis.
In other conditions the treatment depends upon the degree of cervical dilatation:
1. Partially dilated cervix: prevent rupture of membranes as long as possible by:
❖ putting the patient in Trendelenburg position,
❖ avoiding high enema,
❖ avoiding repeated vaginal examination.
❖ When the cervix is fully dilated manage as mentioned later
2. Fully dilated cervix: the foetus should be delivered immediately by:
❖ Rupture of the membranes and forceps delivery: in engaged vertex presentation.
❖ Rupture of the membranes and breech extraction: in breech presentation.
❖ Rupture of the membranes + internal podalic version + breech extraction: may be tried in transverse lie otherwise,
❖ Caesarean section: is indicated as well as for non-engaged vertex and other cephalic malpresentations.

B. Cord prolapse:
Management depends upon the foetal state:
1. Living foetus:
- Partially dilated cervix: Immediate caesarean section is indicated. During preparing the theatre minimise the risk to the foetus by:
✓ putting the patient in Trendelenburg position,
✓ manual displacement of the presenting part higher up,
✓ if the cord protrudes from the vulva, handle it gently and wrap it in a warm moist pack.
✓ Giving oxygen to the mother.
- Fully dilated cervix: the foetus should be delivered immediately as in cord presentation.
2. Dead foetus:
- Spontaneous delivery is allowed.
- Caesarean section: is the safest procedure in obstructed labour as destructive operations are out of modern obstetrics.
Complications of cord prolapsed: Cord-prolapse is obstetric emergency because following complications occur due to cord prolapse and need immediate treatment and nursing care.
➤ Placental abruption
➤the fetus can put stress on the cord
➤ loss of oxygen to the fetus,
➤ Decreased vascular supply to the fetus
➤ Increased maternal mortality and morbidity
➤ stillbirth
➤ Fetal death