Definition of Amputation -An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Definition of Amputation
Amputation is the removal of a body extremity by trauma, prolonged constriction, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene.
[Reference: en.wikipedia.org]
Or
Surgical removal of a dead or non-functioning limb, part of a limb or organ is called amputation.
[Ref-Bailey & Love’s, 25th edition, P-915]
Or
Amputation is defined as removal of the limb through a part of a bone.
[Ref-John Ebnezar’s, “Orthopedics for Nurses”, 1″ edition, P-371)
Or
Amputation is the surgical or traumatic removal of a part of an individual’s body through bone. Disarticulation is the removal of a part of the body through a joint Space.
[Ref-Lippincott, Adult orthpaedic nursing, Page-445]

Incidence rate of amputation:
1) Age: Common in 50-75 years age group.
2) Sex: Seventy-five percent men, twenty-five percent women.
3) Limbs: Eighty-five percent is through the lower limbs, fifteen percent is the upper limbs.
[Ref-John Ebnezar’s, “Orthopedics for Nurses”, 1″, Pg-777]
Indications of amputation:
1) Dead limb: Gangrene.
2) Deadly limb:
a) Wet gangrene.
b) Spreading cellulites.
e) Arteriovenous fistula.
d) Others (e.g. Malignant bone tumor)
3) Dead loss’ limb :
a) Severe rest pain.
b) Paralysis.
c) Other (e.g. contracture, trauma)
[Ref-Bailey & Love’s, “Short Practice of Surgery”, 25th edition, P-915]
Or
A. Hippoerates described three indications of amputation:
a. To remove useless limbs.
b. To reduce invalidism and
c. To save the patient’s life.
B. Today, elective amputations of the lower extremity are often performed as a result of-
a. A progressive peripheral vascular disease and arteriosclerosis (often secondary to diabetes mellitus).
b. Infection due to gangrene and osteomyelitis.
e. Trauma including crushing injuries, thermal and electrical burn and frostbite.
d. Congenital deformities.
e. Malignant tumors
f. Nerve injuries.
g. Miscellaneous.
C. Upper extremity elective amputations are most often performed as a result of;
a. Severe trauma (acute injuries, thermal and electrical burns, frostbite).
b. Malignant tumors.
e. Infection (gas gangrene and chronic osteomyelitis).
d. Congenital deformities.
D. Traumatic amputations of upper or lower extremities occur when a portions of the body is unexpectedly severed.common instances in which that occurs are accidentals with:
a. Saws.
b. Knives.
c. Machinary.
d. Vehicles.
[Ref-Lippincott, Adult orthopaedic nursing, Pg-445]
Indications of mid thigh amputation or above knee amputation:
1. Buerger’s disease with gangrene.
2. Osteomyelitis.
3. Severe trauma of the lower limb below knee.
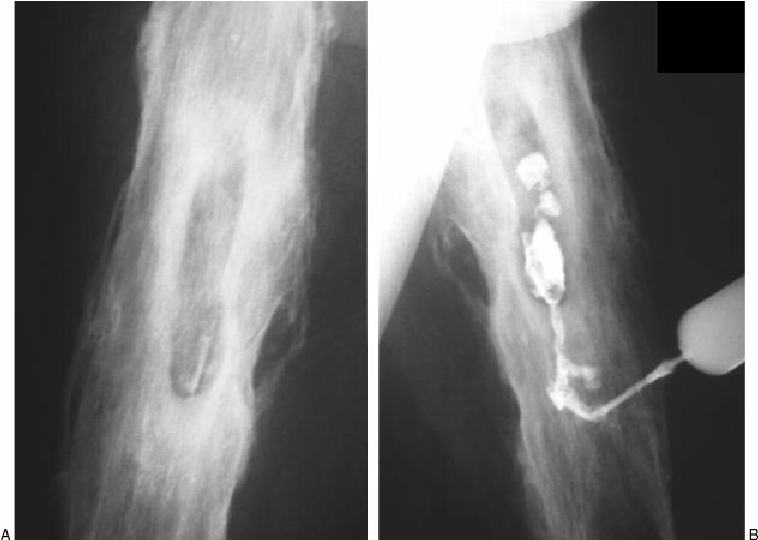
There are two types of amputation:
1. Closed amputation: In closed type amputation, skin flaps are pulled over the bone end and are sutured in place as part of the amputation procedure. This is done most of the times as an elective procedure and may be above knee or below knee, above elbow or below elbow this skin is closed primarily after amputation.

2. Open amputation: The open method is used for patients who have or are likely to develop an infection. The wound remains open with drains to allow sections to escape from the site until the infection has been eradicated. This is done in emergency or severe life threat situations. In this type of amputation the skin is not closed primarily and it is followed by any one of the closure methods like secondary cle reamputation, revision amputation or plastic repair depending upon prevailing local situation. Indications for open amputations are infections and severe crush injuries

[Ref-John Ebnezar’s, “Orthopedics for Nurses” + Lippincott, Adult orthopaedic nursing -445]
Level of amputation:
1. Upper limbs:
a. Forequarter.
b. Shoulder disarticulation.
e. Short above elbow,
d. Standard above elbow.
e. Elbow disarticulation.
f. Very short below elbow,
g. Medium below elbow,
h. Long elbow,
L. Wrist disarticulation.
j. Transmetacarpal amputation.
2. Lower limbs:
a. Hip disarticulation.
b. Very short above knee.
c. Short above knee.
d. Medium above knee.
e. Very long above knee.
f. Knee disarticulation.
g. Very short below knee,
h. Short and below knee.
3.Ankle amputation:
a. Syme’s amputation: here the level of bone section is 0.6 cm proximal to the ankle joint.
b. Sarmiento’s amputation; here the level is 1.3 cm proximal to the joint,
c. Wagner’s is two stage Syme’s amputation.
d. Body’s amputation; this consists of talectomy and calcaneotibial arthrodesis.
e. Pirogoff’s amputation; in this only anterior part of the calcaneum is removed.
4. Foot amputation:
a. Amputation of great toes and other toes,
b. Amputation through the metatarsal bones,
c. Lisfranc’s operation; amputation is at the level of the tarso-metatarsal joints,
d. Chopart’s operation; amputation is through the midtarsal joints.
[Ref-John Ebnezar’s, “Orthopedics for Nurses”, 4″ edition, P-788]

Complications of amputation:
1. Early complications:
i) Reactionary hemorrhage.( due to in adequate ligature hemostasi)
ii) Haematoma.
ⅲ) Abscess formation.
iv) Gas gangrene. (can occur in a mid thigh stump from faecal contamination)
v) Wound dehiscence (due to Ischemia)
vi) Pulmonary embolism.
vii) Deep vein thrombosis.
viii) Infection.
2. Late complications:
i) Pain due to unresolved infection (sinus, osteitis, sequestrum),
ii) A bone spur.
iii)A scar adherent to bone.
iv) Amputation neuroma.
v) Phantom limb. (Pseudo feeling of the presence of the amputed limb).
vi) Ulceration of the stump.
vii) Cold and discolored stump.
(Ref-Bailey & Love’s, “Short Practice of Surgery”, 25th edition, P-917-918)
Level of amputation in details:
Toe: loss of any or all of the toes is usually due to trauma or as a sequella to diabetes mellitus or frostbite.
Metatarsal: Metatarsal or mid foot amputation is performed as a result of trauma or PVD secondary to diabetes mellitus. Metatarsal amputation is performed over removal of toes to gain assurance of good blood supply.
Syme: Syme or foot amputation is the removal of the foot at the ankle.
Below the knee: below the knee amputation preserve the knee joint and make prosthetic fitting and amputation easier
Knee disarticulation: Knee disarticulation removes the lower leg through the knee joint the procedure is rarely used because of difficulty in fitting prosthetics.
Above knee: Above the knee amputation do not preserve the knee, they are usually performed for trauma or PVD..
Hip disarticulation: Hip disarticulation is the removal of the leg through the hip joint. And occurs more commonly in younger patients due to trauma or neoplasm. Hemipelvictomy: Hemipelvictomy is an amputation that removes half of the patients leg and is usually performed because of neoplasm.
Hemicorporectomy: Hemicorporectomy is the removal of the lower half of the body, which includes the loss of the lower extremities, a colostomy, a urinary diversion, and loss of sex organs. It is usually performed for advanced pelvic cancer or pelvic sepsis.
Finger and thumb: finger and thumb amputation includes all or only apportions of the digit, it is usually due to trauma or frostbite.
Wrist disarticulation: Wrist disarticulation is the removal of the hand through the wrist joint.
Below the elbow: Below the elbow amputation is usually performed as the result of trauma or a congenital deformity.
Elbow disarticulation: Elbow disarticulation is the removal of the arm through the elbow.
Above the elbow: above the elbow amputation is usually performed as the result of trauma or congenital deformity
Shoulder disarticulation: It is the removal of an arm through the shoulder joint,
Forequarter amputation: it is the removal of a large portion of the patients shoulder and an arm. It is usually performed as the result of trauma or neoplasm.
[Ref-Lippincott, Adult orthopaedic nursing -446]
Preparation the patients for this operation:
1) Mental preparation:
This is very important and is certainly is not easy task to make the patients accept the reality. As a nurse motivation and assurance can be given tactfully.
a) Explained clearly to the patients that amputation which is being planned for him is in the best interest.
b) You should convince a dead and useless limb will create more harm than good and lead to fetal complications like septicaemia, gas gangrene, tetanus, fat embolisms, shock etc.
c) Explain to the patient that it is better to lose a limb rather than a life will make the patient cope easily with the tragedy.
d) Example of the patient who has a similar worser experience can help to lessen the sorrow.
e) Assurance that with the availability of the state of art prosthetics. Rehabilitation is made easier and patient need not life of a handicap.
f) Encourage the family member to help to cope with the problem.
g) Divert the mind to reduce tension by relaxation technique such as watching tv, listening song, reading book,deep breathing,
h) Tell patients that nurse and doctor will do the best for him.
2) Physical preparation:
i) G/A fitness:
a . Ask the patients about any previous heart lungs diseases. if present control them.
b. Control DM, asthma, HTN if present
e. Correct body weight
d. Prepare investigation profile of -TC, DC, ESR, Hb%, Chest x-ray, Limb X-ray, Rh typing & Rh grouping.
e. If sever anaemia is necessary Blood transfusion may be given.
f. Check blood pressure, pulse, heart sound to detect any abnormality.
ii) Skin preparation:
a. Shaving the limb with asetic technique for better operations
b. Washing the operative area by using soap and clean water.
c. Skin cleaning may be alcohol rubbed.
iii) GIT preparations:
a) Nothing per oral must be maintained day before operations from night.
b) If the operation is evening give light diet on the morning.
c) If patints feel thurs give seeps of water.
d) Avoid any kind of food to prevent vomiting.
3) Preoperative teaching:
a) Deep breathing
b) Active or passive exercise of the joints of the body.
c) Proper hygienic practice after operation
d) Correct use of prosthetic device
e) Discuss about the phantom limb/phantom pain sensation.
Nursing care plan of amputed patient:
A) Nursing assessment:
1) Assess level of consciousness.
2) Check vital signs every 15 minute untile stable.
3) Note any signs of pain
4) Assess fluid and electrolyte balance
5) Look for signs of bleeding along the incision
6) Note the amount of drainage from the wound drains.
7) Assess for urinary output and note down the amount.
8) Obserbe emotional response to the surgery and attitude towards loss of limb and copping capability.
9) Observe skin condition of the area.
B) Nursing diagnosis:
1) Pain and discomfort related to bone and soft tissue trauma from surgery.
2) Impaired physical mobility related to the loss of the lower leg.
3) Impaired skin integrity related to the surgical incision and the prosthesis. 4) Distuebance in self concept related to self-esteem, body image, and role performance.
5) Risk of developing infection related to lack of stump care.
C) Nursing care plan:
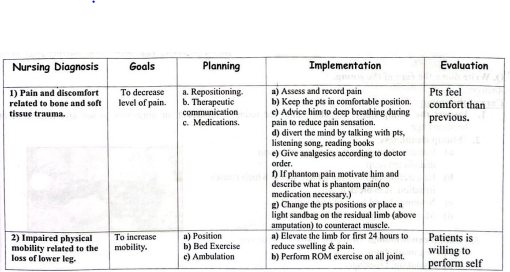
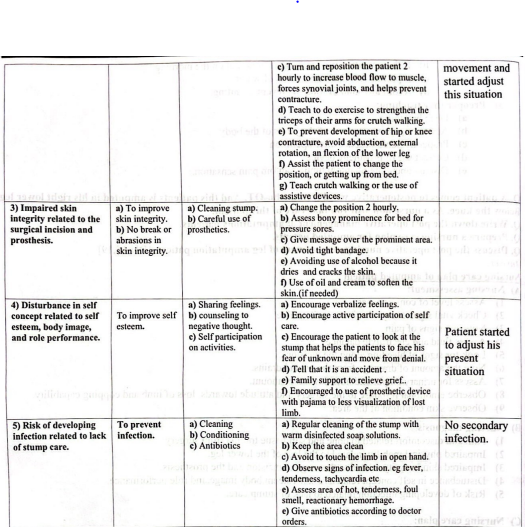
Care of the stump:
1. Inspect the stump daily:
Regular stump for redness, blistering, or abrasions to see any infection, or haemorrhage.
2. Stump cleanliness:
a) Regular cleaning of the stump with warm disinfected soap.
b) Be careful, soap will not adhere stump which causes irritation, skin break down.
c) Nothing should be used after bathed.
d) Mop it thoroughly with dry towel.
3. Stump conditioning:
The can be done by observing following instructions.
a) Avoid tight bandage.
b) Regular and correct application of a firm elastic bandage.
c) Regular isometric exercise to the stump muscles proximal to the amputation.
d) Repeated messaging to improve the tone of the muscle.
e) Avoiding use of alcohol,because it dries and cracks the skin.
4. Anti-oedema measure:
a. Limb should be elevated with elastropcripe bandage application.
b. All the joint including stump are subjected to active exercise.
c. Stump bandaging is an art and is very useful in preventing the oedema.
5. Other Measures:
a) Encourage prone lying to prevent hip flexion contractures.
b) Avoid pillows beneath the knee to prevent flexion contracture of the knee.
c) Avoid long period of setting for the same reasons mentioned above.
d) Avoid dragging on the bed, rather push up the forearm to get up.
e) Proper positioning can be achieved with the use of a pillow while lying face down in bed. If you are lying on your back, avoid placing any pillows under your limb.
f) One simple position that can greatly increase flexibility is to lay on your stomach and stretch the limb backward.
g) When lying in bed remember to keep your legs together and try to avoid any type of rotation.
h) Keeping these strategies in mind can help prevent unwanted contractures.
