Definition of Health – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Definition of Health
The World Health Organization (1948) provided the widely accepted definition of health which is as follows:
“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”
or
During the Ottawa Charter for Health Promotion in 1986, the WHO said that health is:T “A resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities.”
Changing Concept of Health:
A brief account of the changing concepts of health is given below-
A. Biomedical concept: A person was considered as healthy if he was free from disease or absence of disease. This concept is known as the biomedical concept,
a) This concept is based on germ theory of disease
b) Criticism: role of environmental, social, psychological and cultural determinates of health are ignored.
B. Ecological concept: The ecologists viewed health as a dynamic equilibrium between men his environment and disease a mal-adjustment of the human organism to environment. The ecological concept raises two issues:
a) Imperfect man
b) Imperfect environment
C. Psychological concept: Health is not only a biomedical phenomenon, but one which is influenced by social, psychological, cultural, economic & political factors of the people concerned.
a) Social factor:
- Poverty
- Illiteracy
- Habits and lifestyles (Smoking, Drugs, Multiple sex partners etc.)
b) Psychological factor:
- Anxiety
- Tension
- Emotional breakdown
D. Holistic concept: The holistic model is a synthesis of all the above concepts. The holistic approach implies that all sectors of society have an effect on health.
Health Belief Model:
The Health Belief Model (HBM) is a psychological model that attempts to explain and predict health behaviors. This is done by focusing on the attitudes and beliefs of individuals. The HBM was first developed in the 1950s by social psychologists Hochbaum, Rosenstock and Kegels working in the U.S. Public Health Services. The model was developed in response to the failure of a free tuberculosis (TB) health screening program.
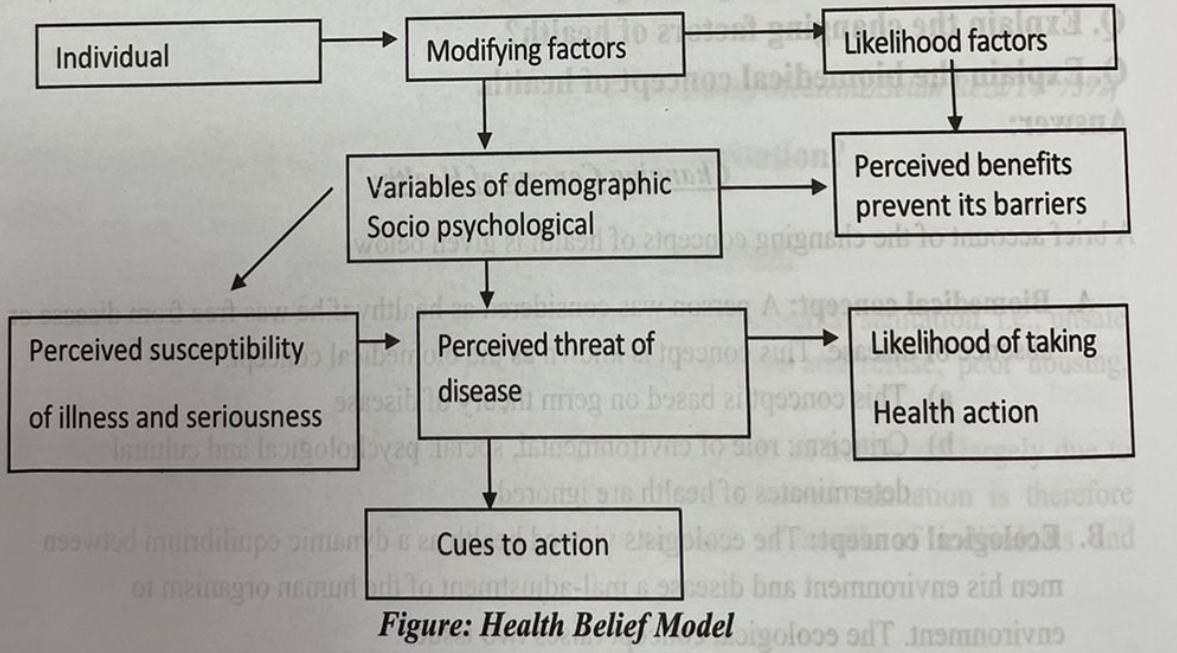
Components of Health Belief Model:
1. Perceived susceptibility to a disease, e.g. smokers suspect of cancer.
2. Perceived seriousness of a disease and its effect on individual lifestyle, e.g. cancer effects on lifestyle.
3. Perceived value of action, e.g. preventive measures or curative measures.
Factors That Influence Health & Illness Relate To Human Dimensions:
The factors that influence health and illness related to the person in terms of the human dimensions are as follows:
1. Physical dimension,
2. Emotional dimension,
3. Environmental dimension,
4. Intellectual dimension,
5. Socio-cultural dimension,
6. Spiritual dimension.
A. Physical dimensions: It includes genetic makeup, age, developmental level, race and sex. All are parts of individuals, which strongly influence health status, and health practices.
B. Emotional dimension: It express that how the mind and body interact to affect body function and to respond to body; emotion also influences health. Long-term stress affects the body system and anxiety affects health habits. Calm acceptance and relaxation can actually change the body responses to illness.
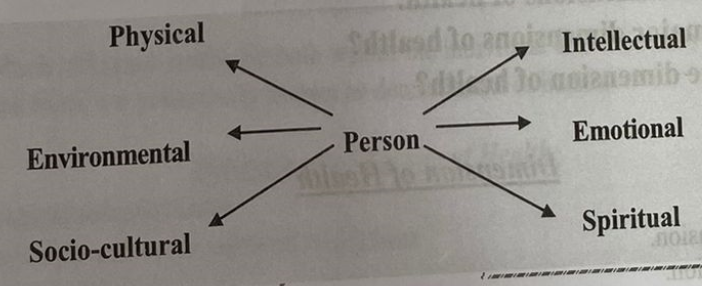
Figure: Factors affecting health and illness
C. Environmental dimension: It has many influences on health and illness. Housing, sanitation, climate and pollution of air, food and water are aspects of the environment, which causes illness.
D. Intellectual dimension: It encompasses cognitive abilities, educational background and past experiences. These influence client responses to teaching about health and reactions to nursing care during illness. They also play major role in health behaviors.lev bevise
E. Socio-cultural dimension: It includes individual’s economic level, educational status, lifestyle, family, and culture. These are all with influence on the health and illness of the people.
F. Spiritual dimension: Spiritual and religious beliefs and values are the important components of how a person behaves in the health and illness. It is important that nurse respects these values and understand their importance to the individual client.
New Philosophy of Health:
In recent years, we have acquired a new philosophy of health, which may be stated as below –
- Health is a fundamental human right.
- Health is the essence of productive life & not the result of ever increasing expenditure on medical care.
- Health is intersectoral.
- Health is an integral part of development.
- Health is central to die concept of quality of life.
- Health involves individuals, state and international responsibility.
- Health and its maintenance is a major social investment.
- Health is world-wide social goal.
Dimension of Health
Major Dimension:
- Physical dimension.
- Mental dimension.
- Social dimension.
- Spiritual dimension.
Minor dimensions;
- Emotional dimension
- Vocational dimension
Others:
✔ Philosophical dimension.
✔ Cultural dimension.
✔Socio-economic dimension.
✔ Educational dimension.
✔ Environmental dimension.
✔ Nutritional dimension.
✔ Curative dimension.
✔ Preventive dimension.
Positive Health:
The state of positive health implies the notion of “perfect functioning” of the body & mind. It conceptualizes health biologically, psychologically and socially. A person who enjoys health at three planes i.e. good physical, mental and social well-being is said to be in a state of positive health.
Determinants of Health:
The factors which influence health lie both within the individual and externally in the society in which he or she lives, are collectively known as determinants of health.
Determinants/Factors of Health:
1. Biological determinants
2. Behavioral and socio-cultural conditions
3. Environment
4. Socio-economic conditions
5. Health services
6. Aging of the population
7. Gender
8. Other factors.
A. Biological determinants: The physical and mental traits of every human being are to some extent determined by the nature of his genes at the time of conception.
B. Behavioral and socio-cultural conditions:
a) The way people live,
b) Cultural pattern.
c) Personal habits.
d) Life style.
C. Environment:
a) Physical environment: Air pollution, water pollution, soil pollution. Food, excreta, refuse.
b) Biological: Human being, plants, animal, micro-organisms, insects, housing.
c) Psychosocial: Customers, occupation, religion, education.
D. Socio-economic conditions:
a) Economic status.
b) Education.
c) Occupation.
d) Political system.
E. Health and family welfare services:
a) Immunization of children.
b) Provision of safe water supplying
c) Maternal and child health care.
F. Gender: Women’s health is an important issue for the society.
Indicators of Health:
1. Mortality indicator
- Crude death rate.
- Expectation of life.
- Infant mortality rate
- Under-5 proportionate mortality rate.
- Maternal mortality rate
- Disease specific mortality
- Proportional mortality rate
2. Morbidity indicators;
- Incidence and prevalence
- Notification rates.
- Attendance rates at out-patient departments, health centers etc.
- Admission, re-admission & discharge rates.
- Duration of stay in hospital.
- Spells of sickness or absence from work of school
3. Disability rates
- Event-type indicators;
✓ Number of days of restricted activity.
✓ Bed disability days.
✓ Work loss days within a specific period.
4. Nutritional status indicators:
- Anthropometric measurements of pre-school children e.g. weight & height, mid-arm circumference.
- Heights (sometimes weights) of children at school entry.
- Prevalence of low birth weight.
5. Health care delivery indicators;
- Doctors-population ratio.
- Doctors nurse ratio.
- Population bed ratio
- Population per health center/sub-center.
- Population per traditional birth attendant.
6. Utilization rates
- Proportion of infants who are “fully immunized” against the 6 EPI diseases
- Percentage of the population using the various methods of family planning.
- Bed-occupancy rate in hospital.
- Average length of stay in hospital.
- Patient turnover ratio
7. Indicators of social & mantel health:
- Homicide rate.
- Suicide rate.
- Drug and alcohol abuse rate.
- Family violence rate.
- Battered baby and battered wife syndromes rate
- Road traffic accidents rate.
- Smoking rate
8. Environmental indicators:
- Proportion of population having access to safe water supply.
- Proportion of population having access to safe sanitation
- Indicators relating to pollution of air & water, radiation, solid wastes etc.
9. Socio-economic indicators:
- Rate of population increase
- Per capita GNP (gross national product)
- Level of unemployment.
- Dependency ratio.
- Literacy rates especially female literacy rates.
- Family size.
- Housing- the number of persons per room.
- Per capita calorie availability.
10. Health policy indicators
- Proportion of GNP spent on health services.
- Proportion of GNP spent on health related activities.
- Proportion of total health resources devoted to primary health care.
11. Indicators of quality of life
- Infant mortality rate.
- Life expectancy at age one.
- Literacy
12. Other indicators:
- Social indicators- population, family formation, families etc.
- Basic needs indicators- calorie consumption, access to water, life expectancy etc.
- Health for all indicators.
Definition of Illness:
Illness is a subjective state of the person who feels aware of not being well.
or
Illness is a broad term that defines the poor state of mind, body, and, to a certain extent, spirit. It is the general feeling of being sick or unwell (outside the person’s belief of good health).
Health & Illness Continuum:
- The individual’s state of health is one of continual change. He moves back and forth from health to illness and back to health again. His condition is rarely constant. He may wake up feeling great, develop a headache mid-morning, and feel fine again by noon.
- The health-illness continuum (see figure 2-1) illustrates this process of change, in which the individual experiences various states of health and illness (ranging from extremely good health to death) that fluctuate throughout his life.
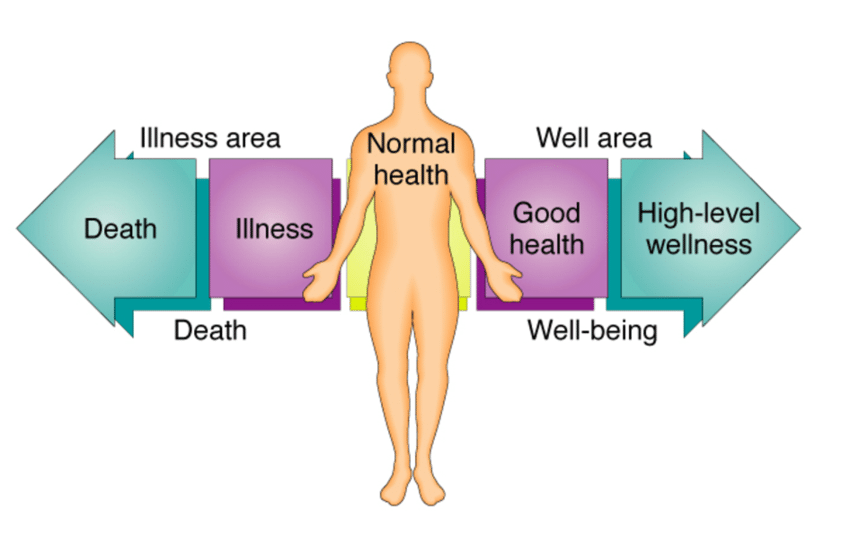
Figure 2.1. The health-illness continuum.
- As we previously stated, health, just as life itself is a process of continual change. And we must continually adapt to these changes in our lives in order to maintain good health and well-being. It is our adaptation or response to that change, rather than the change itself, that affects our health. .
- For example, two students just found out about a big test tomorrow, for which they are completely unprepared. One student responds to this stressful situation (stressor) by going home, getting his books out, and starting to study. The other student breaks out into a sweat, and spends most of the evening fretting over this outrage and imagining what will happen to him if he doesn’t pass the test. No doubt, this student is doing more damage to his health than is his friend. And, considering the time and energy he is expending on worrying (and not studying), he may experience even more stress when they receive their grades!
- Adaptation and effective functioning, even in the presence of chronic disease, can be considered a state of wellness. A person may be in perfect physical condition, but feel too tired and “blue” to go to work, while his co-worker, a diabetic, is at work, functioning fully and accomplishing his job.
- NOTE: Death occurs when adaptation fails completely, and there is irreversible damage to the body.
Client-Centered Care
Definition of Client Centered Care:
Client centered care starts with the client perspective and is designed to meet his or her distinctive needs.
Or
Client centered care is an approach in which clients are viewed as whole persons; it is not merely about delivering services where the client is located. Client centered care involves advocacy, empowerment and respecting the client’s autonomy, voice, self-determination, and participation in decision-making.
Attributes of Client-Centered Care:
In order to provide client- centered care, the nurse has certain attributes and will demonstrate in her action as the followings:
1. Appreciate that each person is a unique product of heredity, environment, culture and spirituality. This indicates that the nurse interacts with clients on an individual basis, even though their health care needs may appear to be similar.
2. Believe that person strive for their highest potential, Nurses’ function is to assist persons to achieve growth in relation to their health needs.
3. Respects the growth of each individual recognizes that even the sickest or poorest of persons have strengths that can be mobilized to meet their needs and achieve their potentials.
4. Recognize our own humanity, Nurses are human too with unique strengths and needs. To care effectively for other, nurses must have self-awareness to recognize both what they can offer others and what their own personal limitation.
5. Be genuine.
6. Encourage the client to retain control.
7. Recognize that person have basic needs and are motivated to fulfill these needs.
8. Realize all behavior has meaning. Nurses appreciate that a person’s action communicates messages about his or her feelings, beliefs or physical function. The nurse respect the meaning of a person’s behavior and avoids such as wrong, bad or worried even through behavioral manifestation may be perplexing or difficult.
Ways to Develop Client Centered Care:
There is no one way to approach a client and no single interpersonal strategy that works equally well with every client. Nurses who carry or believe in client centered care bring about knowledge and skills to each client involuntary. Novice nurses or nursing students can develop client centered care and holistic (Physiological, Psychological & Spiritual) nursing through the following guidelines:
1. Study and analyze the concepts.
2. Determine if one use a bio-psycho-social-spiritual model to guide our clinical practice.
3. Determine whether there are areas of fragmentation in our personal life.
4. Explore the steps that increase our commitment to our holistic development process.
5. Integrate the standards of holistic into clinical practice. These standards include-
- Client centered care include family and significant others.
- Nurses-focused concepts (committed to personal development).
- Cultural care.
- Health education and mutual decision making.
- Health promotion.
- Spiritual care.
- Care of the environment.
- Use of nursing process.
- Use of research to guide clinical practice.
