Definition of Hemorrhoids – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Definition of Hemorrhoids
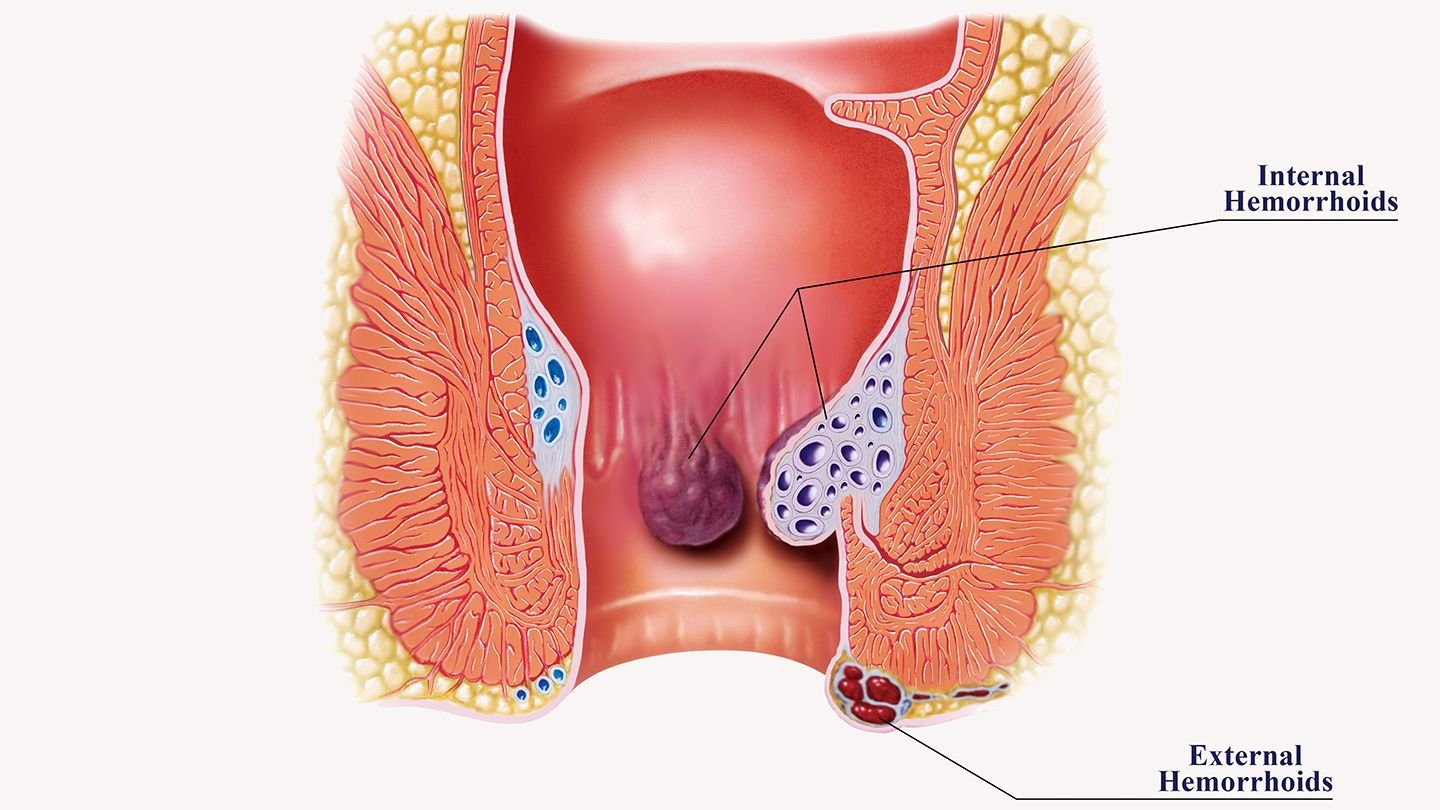
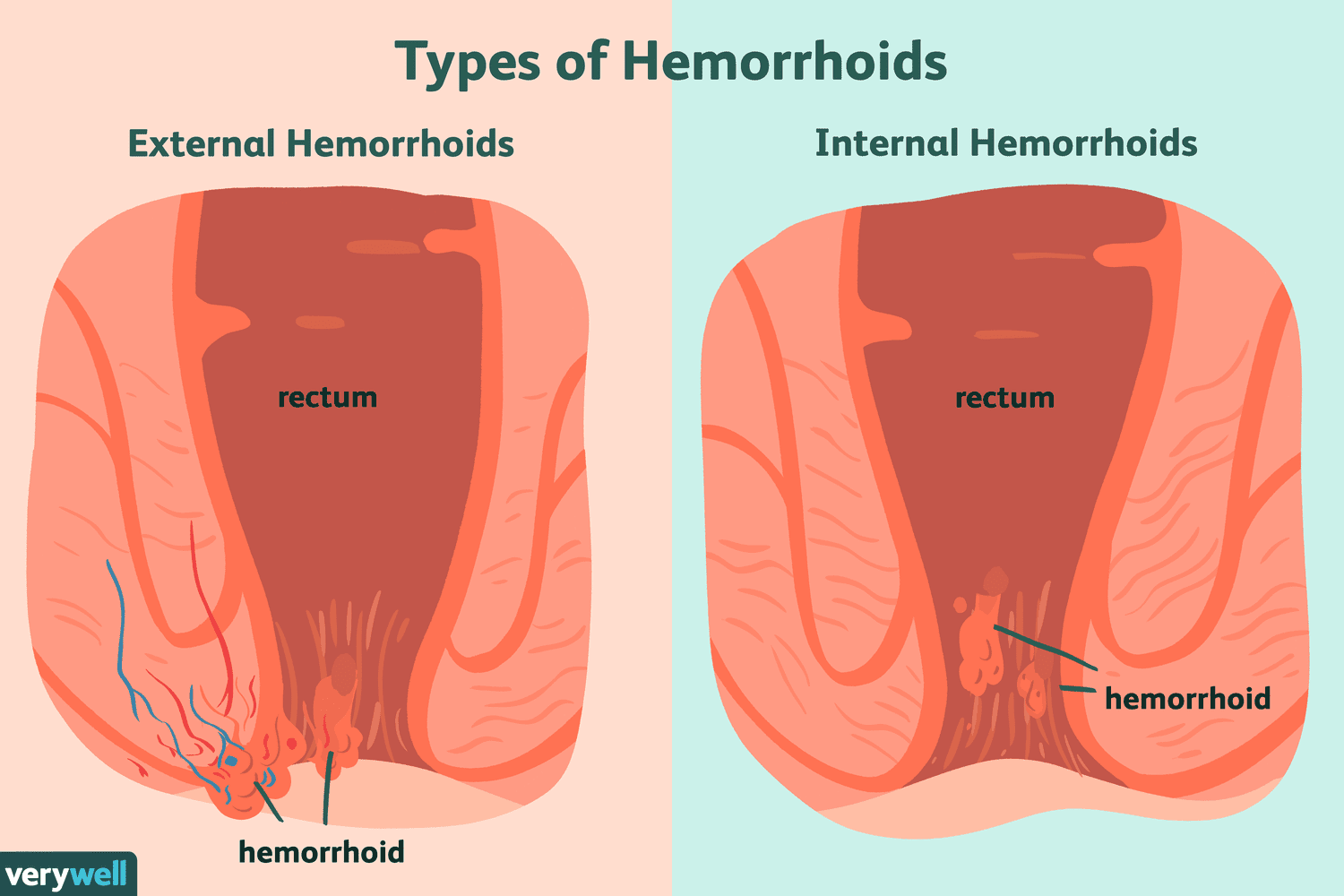
Hemorrhoids also called piles, are swollen veins in the anus and lower rectum, similar to varicose veins.
or,
Hemorrhoids are vascular masses that protrude into the lumen of the lower rectum or perianal area.
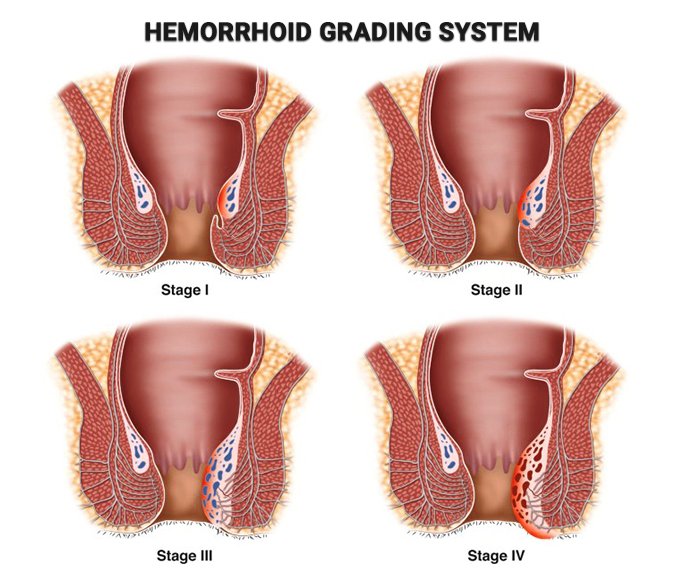
Hemorrhoids, also called piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term “hemorrhoid” is often used to refer to the disease.
Causes of Hemorrhoids:
The veins around the anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements
- Sitting for long periods of time on the toiletChronic diarrhea or constipation
- Obesity
- Pregnancy
- Anal intercourse
- Low-fiber diet
Clinical Feature of Hemorrhoids:
Signs and symptoms of hemorrhoids may include:
- Painless bleeding during bowel movements patient might notice small amounts of bright red blood on the toilet tissue or in the toilet
- Itching or irritation in anal region
- Pain or discomfort
- Swelling around anus
- A lump near the anus, which may be sensitive or painful (may be a thrombosed hemorrhoid)
Prevention
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
⇒ Eat high-fiber foods: Eat more fruits, vegetables and whole grains
⇒ Drink plenty of fluids: Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
⇒ Consider fiber supplements: Most people don’t get enough of the recommended amount of fiber -25 grams a day for women and 38 grams a day for men in their diet.
⇒ Don’t strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
⇒ Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that
may be contributing to your hemorrhoids.
⇒ Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
Complications
Complications of hemorrhoids are very rare but include:
1. Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don’t have enough healthy red blood cells to carry oxygen to your cells.
2. Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be “strangulated,” another cause of extreme pain.
Management of Hemorrhoids:
Assessment
1. Pain (more so with external hemorrhoids), sensation of incomplete fecal evacuation, constipation, and anal itching. Sudden rectal pain may occur if external hemorrhoids are thrombosed.
2. Bleeding may occur during defecation; bright red blood on stool caused by injury of mucosa covering hemorrhoid.
3. Visible and palpable masses at anal area.
Diagnostic Evaluation
1. External examination with anoscope or proctoscope shows single or multiple hemorrhoids.
2. Barium edema or colonoscopy rules out more serious colonic lesions causing rectal bleeding such as polyps.
Primary Nursing Diagnosis
- Pain (acute or chronic) related to rectal swelling and prolapse
Therapeutic Intervention/Medical Management
1. High-fiber diet to keep stools soft.
2. Warm sitz baths to ease pain and combat swelling.
3. Reduction of prolapsed external hemorrhoid manually.
Surgical Interventions:
1. Injection of sclerosing solutions to produce scar tissue and decrease prolapse is an office procedure.
2. Cryodestruction (freezing) of hemorrhoids is an office procedure.
3. Surgery may be indicated in presence of prolonged bleeding, disabling pain, intolerable itching, and general unrelieved discomfort.
Pharmacologic Intervention
1. Stool softeners to keep stools soft and relieve symptoms.
2. Topical creams, suppositories or other preparation such as Anusol, Preparation H, and witch- hazel compresses to reduce itching and provide comfort.
3. Oral analgesics may be needed.
Nursing Intervention
1. After thrombosis or surgery, assist with frequent repositioning using pillow support for comfort.
2. Provide analgesics, warm sitz baths, or warm compresses to reduce pain and inflammation.
3. Apply witch-hazel dressing to perianal area or anal creams or suppositories, if ordered, to relieve discomfort.
4. Observe anal area postoperatively for drainage and bleeding.
5. Administer stool softener or laxative to assist with bowel movements soon after surgery, to reduce risk of stricture.
6. Teach anal hygiene and measures to control moisture to prevent itching.
7. Encourage the patient to exercise regularly, follow a high fiber diet, and have an adequate fluid intake (8 to 10 glasses per day) to avoid straining and constipation, which predisposes to hemorrhoid formation.
8. Discourage regular use of laxatives; firm, soft stools dilate the anal canal and decrease stricture formation after surgery.
9. Tell patient to expect a foul-smelling discharge for 7 to 10 days after cryodestruction.
10. Determine the patient’s normal bowel habits and identify predisposing factors to educate patient about preventing recurrence of symptoms.
Documentation Guidelines
1. Physical findings:
- Rectal examination,
- Urinary retention,
- Bleeding, and
- Mucous drainage
2. Wound healing: Drainage, color, swelling
3. Pain management: Pain (location, duration, frequency), response to interventions
4. Postoperative bowel movements: Tolerance for first bowel movement
Discharge and Home Healthcare Guidelines
1. Teach the patient the importance of a high-fiber diet, increased fluid intake, mild exercise, and regular bowel movements.
2. Be sure the patient schedules a follow-up visit to the physician.
3. Teach the patient which analgesic applications for local pain may be used.
4. If the patient has had surgery, teach her or him to recognize signs of urinary retention, such as bladder distension and hemorrhage and to contact the physician at their appearance.
Hemorrhoidectomy Postoperative Complications
Most patients are satisfied with the results of the surgery and recover without any problems. Complications associated with hemorrhoidectomy are rare and include:
- Anal fistula or fissure
- Constipation
- Excessive bleeding
- Excessive discharge of fluid from the rectum
- Fever of 101°F or higher
- Inability to urinate or have a bowel movement
- Severe pain, especially when having a bowel movement
- Severe redness and/or swelling in the rectal area
- Side effects of anesthesia (e.g., spinal headache)
Postoperative Nursing Management and Care of Hemorrhoidectomy Surgery:
Postoperative care
A. Post-operative note and orders: The patient should be discharged to the ward with comprehensive orders for the following:
- Vital signs
- Pain control
- Rate and type of intravenous fluid
- Urine and gastrointestinal fluid output
- Other medications
- Laboratory investigations
The patient’s progress should be monitored and should include at least:
- A comment on medical and nursing observations
- A specific comment on the wound or operation site
- Any complications
- Any changes made in treatment
B. Aftercare: Prevention of complications
- Encourage early mobilization:
✓ Deep breathing and coughing
✓ Active daily exercise
✓ Joint range of motion
✓ Muscular strengthening
✓ Make walking aids such as canes, crutches and walkers available and provide instructions for their use
- Ensure adequate nutrition
- Prevent skin breakdown and pressure sores:
✓ Turn the patient frequently
✓ Keep urine and faeces off skin
- Provide adequate pain control
C. Discharge note: On discharging the patient from the ward, record in the notes:
- Diagnosis on admission and discharge
- Summary of course in hospital
- Instructions about further management, including drugs prescribed.
Ensure that a copy of this information is given to the patient, together with details of any follow-up appointment
Postoperative Management
If the patient is restless, something is wrong.
Look out for the following in recovery:
- Airway obstruction
- Hypoxia
- Haemorrhage: internal or external
- Hypotension and/or hypertension
- Postoperative pain
- Shivering, hypothermia
- Vomiting, aspiration
- Falling on the floor
- Residual narcosis
The recovering patient is fit for the ward when:
- Awake, opens eyes
- ExtubatedBlood pressure and pulse are satisfactory
- Can lift head on command
- Not hypoxic
- Breathing quietly and comfortably
- Appropriate analgesia has been prescribed and is safely established
Nursing Responsibilities:
- The patient should be kept on nothing by mouth according to doctor’s order.
- IV fluid should be given according to doctor’s order.
- Maintain input and output chart.
- Maintain patency of NG tube. Notify physician if tube becomes dislodged
- Provide oral hygiene on a regular, frequent basis, including petroleum jelly for lips.
- Auscultate for resumption of bowel sounds and note passage of flatus.
- Monitor tolerance to fluid and food intake, noting abdominal distension, reports of increased pain, cramping, nausea and vomiting.
- Avoid milk and high-carbohydrate foods in the diet.
- Note admission weight and compare with subsequent readings.
- Administer IV fluids, TPN, and lipids as indicated.
- Monitor laboratory studies (Hb and Het, electrolytes, and total protein, prealbumin).
- Progress diet as tolerated, advancing from clear liquid to bland diet with several small feedings.
- Administer medications as indicate
✓ Anticholinergics: atropine, propantheline bromide (Pro-Banthine)
✓ Fat-soluble vitamin supplements, including vitamin B12, calcium
✓ Iron preparations
✓ Protein supplements
✓ Medium-chain triglycerides (MCT)
- Care of the surgical area
- Care of IV cannel
- Care of the bowel and bladder
- Patient and their family members assured and informed about patient condition.
