Definition of Implantation – Introduction to fundamental concepts of Biological Science including the organization and common characteristics of living matters, cell structures and functions, food production by photosynthesis, harvesting energy, mechanism of cells reproduction, genetics, evolutions, and Human Biology. Introduction to general chemistry including basic concepts about matter, atomic structure, chemical bonds, gases, liquid, and solids, solutions, chemical reactions, acid, bases, and salt;
organic and biochemistry including hydrocarbons and their derivatives, carbohydrates, lipids, proteins, enzymes, vitamins, and minerals, nucleic acids; principles of physics and applications to nursing including gravity and mechanics, pressure, heat and electricity; nuclear chemistry and nuclear physics, effects of radiation on human beings, and protection and disposal. The aim of the course is to acquire knowledge and skills in general biological science, general chemistry and physics.
Definition of Implantation
Implantation (human embryo) is the process or an event that occurs early in human pregnancy in which the human embryo adheres to the wall of the uterus. It occurs 6th or 7th day after fertilization.
Sites of implantation:
Normal site- Posterior wall of the uterus close to the fundus. But implantation anywhere in the upper part the uterine cavity is considered as normal.
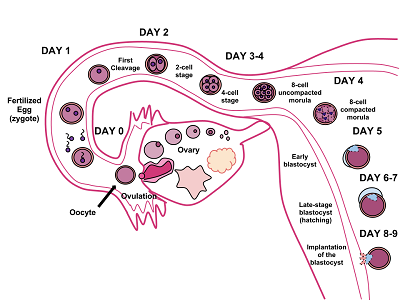
Figure: Implantation
Vagina
Definition of Vagina:
The vagina is a fibromusculo-membranous sheath communicating the uterine cavity with the exterior at the vulva.
- It constitutes the excretory channel for the uterine secretion and menstrual blood.
- It is the organ of copulation and forms the birth, canal of parturition
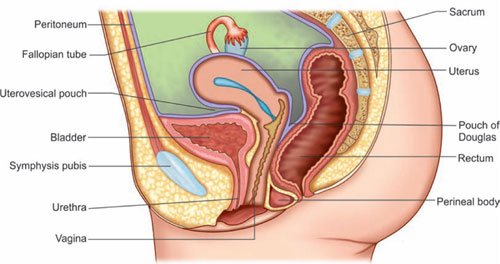
Figure: Mid-sagittal section of the female pelvis showing relative position of the pelvic organs.
Anatomy of the Vagina:
A. Direction: The canal is directed upwards and backwards forming an angle of 45° with the horizontal in erect posture.
B. Diameter: About 2.5 cm, being widest in the upper part and narrowest at its introitus.
C. Walls: An anterior, a posterior and two lateral walls. The length of the anterior wall is about 7 cm and that of the posterior wall is about 9 cm.
D. Fornices: These are the clefts formed at the top of vagina (vault) due to the projection of the uterine cervix through the anterior vaginal wall.
There are four fornices one anterior, one posterior and two lateral; the posterior one being deeper and the anterior is most shallow one.
E. Relations:
a) Anterior: The upper one-third is related with base of the bladder and the lower two-thirds are with the urethra.
b) Posterior: The upper one-third is related with the pouch of Douglas, the middle- third with the anterior rectal wall separated by rectovaginal septum and the lower- third is separated from the anal canal by the perineal body.
c) Lateral walls: The upper one-third is related with the pelvic cellular tissue at the base of broad ligament in which the ureter and the uterine artery lie approximately 2 cm from the lateral fomices. The middle-third is blended with the levator ani and the lower-third is related with the bulbocavernous muscles, vestibular bulbs and Bartholin’s glands.
F. Structures: Layers from within outwards are –
a) Mucous coat.
b) Sub-mucous layer.
c) Muscular layer.
d) Fibrous coat derived from the endopelvic fascia and is highly vascular.
G. Blood supply:
a) Arterial supply:
- Cervicovaginal branch of the uterine artery.
- Vaginal artery a branch of anterior division of internal iliac or in common origin with the uterine artery.
- Middle rectal artery.
- Internal pudendal artery.
b) Venous drainage: Drain into internal iliac veins and internal pudendal veins.
H. Lymphatic drainage: On each side, the lymphatics drain into –
a) Upper one-third: Internal iliac group.
b) Middle one-third up to hymen: Internal iliac group.
c) Below the hymen: Superficial inguinal group.
I. Nerve supply: Sympathetic and parasympathetic from the pelvic plexus. The lower part is supplied by the pudendal nerve.
j. Development:
a) Upper 4/5th, above the hymen: The mucous membrane is derived from endoderm of the canalized sino-vaginal bulbs. The musculature is developed from the mesoderm of two fused Mullerian ducts.
b) Lower 1/5th below the hymen: Is developed from the endoderm of the urogenital sinus.
c) External vaginal orifice: Is formed from the genital fold ectoderm after rupture of the urogenital membrane.
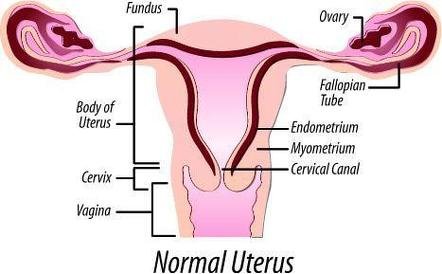
Uterus
Definition of Uterus:
The uterus is a hollow pyriform muscular organ situated in the pelvis between the bladder in front & the rectum behind.
Anatomy of Uterus:
A. Position: Its normal position is one of the anteversion & anteflexion.
B. Measurement: It is about 8 cm long & 5 cm wide at the fundus and its walls are about 1.25 cm thick.
C. Parts: It has got 3 parts:
➤ Body or corpus:
- Fundus.
- Body proper.
➤ Isthmus.
➤ Cervix.
D. Structures; The wall consists of 3 layers, from outside inwards:
a) Perimetrium: It is the serous coat which invests the entire organ except on the lateral borders. The perimetrium is intimately adherent to the underlying muscles.
b) Myometrium.
c) Endometrium.
E. Blood supply:
a) Arterial supply;
- Uterine artery: One on each side arises from the anterior division of the internal iliac artery either directly or as a branch of the hypogastric artery.
- Ovarian and vaginal arteries: It anastomoses with uterine arteries.
b) Venous drainage: The venous channels correspond to the arterial course and drain into internal iliac veins.
F. Lymphatic drainage:
a) Body:
- From the fundus and upper part of the body of the uterus – Aortic and lateral groups of glands.
- Cornu -Superficial inguinal gland along the round ligament.
- Lower part of the body-External iliac groups.
b) Cervix:
- External iliac, obturator lymph nodes either directly or through para-cervical lymph
- nodes.
- Internal iliac groups.
- Sacral groups.
G. erve supply:
a) Sympathetic supply: T5 & T6 (motor) and T10-L1 spinal segments (sensory).
b) Parasympathetic supply: S2-S4 spinal segments (mixed).
Cervix
It is the lower most part of the uterus which extends from the histological internal os & ends at. external os which opens into the vagina after perforating the anterior vaginal wall.
Anatomy of the cervix:
➤ Length: 2.5 cm.
➤ Parts: It has two parts:
- Supravaginal cervix: It is the upper half, lies above the vagina. It is surrounded by pelvic fascia except in its posterior aspect where it is covered with the peritoneum of the pouch of Douglas. It is lined by simple columnar epithelium.
- Vaginal cervix or portio-vaginalis: It is the lower half and lies in the vagina. It is bounded above by the internal os and below by the external os, through which it communicates to the uterine canal and vagina respectively. The vaginal part is covered with stratified squamous epithelium continuous with that of the vagina. The columnar epithelium of the cervical canal and the stratified squamous epithelium of the portio-vaginalis join each other at the external os, the site being known as the squamo-columnar junction.
➤ Relation:
- Anteriorly: Base of the bladder from which it is separated by the pubocervical fascia.
- Posteriorly: It is covered with peritoneum & forms the anterior wall of the pouch of Douglas containing coils of intestine.
- Laterally: Uterus lies just 1 cm lateral to the supravaginal part of the cervix.
➤ Blood supply:
- Arterial supply:
✓ Uterine artery on each side.
✓ Also from ovarian and vaginal arteries.
- Venous drainage: In to the internal iliac veins.
➤ Lymphatic drainage
Uterine Tube/Fallopian Tube
The fallopian tubes are two tortuous ducts which extend from the ovaries to the cornua of the uterus, one on either side.
Anatomy of the fallopian tube/ Uterine tubes/Oviduct:
➤ Length: 10 cm.
➤ Situation: Each lies in the free upper border of the broad ligament of the uterus.
➤ Extension: Its lumen communicates with the uterine cavity at its inner end and with the peritoneal cavity at its outer end.
➤ Parts: The fallopian tube is divided into four parts:
- Interstitial or intramural part: This is about 1.25 cm in length and is the part which traverses the uterine wall. It has no peritoneal coat.
- Isthmus: This is the straight and narrow portion adjacent to the uterus and measures 2.5cm in length.
- Ampulla: This is wider thin walled and tortuous outer portion approximately 5 cm in length which leads to the infundibulum.
- Infundibulum: It is the trumpet shaped outer end of the tube with an opening into the peritoneal cavity (abdominal ostium). The ostium is surrounded by fimbriae, which moves freely and are devoid of broad ligament and pick up ovum when released from ovary.
➤ Structure:
- Serous layer: It is derived from peritoneum.
- Muscular layer: Outer longitudinal and inner circular layer of involuntary muscle.
- Submucous layer: A delicate connective tissue which separates the muscle zone from the mucosa lining of the lumen (Endosalpinx).
- Mucosa: It is lined by ciliated columnar epithelium. The mucous membrane is thrown into complicated folds which fill up the lumen of the tube..
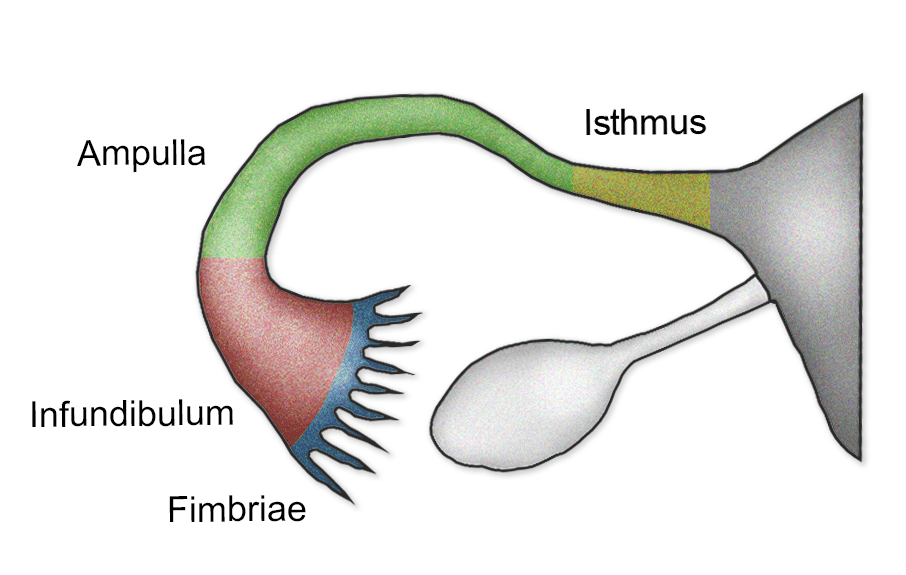
Figure: Parts and cut sections of uterine tube.
➤ Blood supply;
- Arterial supply:
✓ Uterine artery (medial 2/3rd).
✓ Ovarian artery (lateral 1/3rd).
- Venous drainage: Into the pampiniform plexus of the ovary and into the uterine veins.
- Lymphatic drainage: Into aortic and para-aortic nodes.
- Nerve supply;
✓ Sympathetic: From ovarian and superior hypogastric plexus.
✓ Parasympathetic: From vagus.
➤ Development:
- Mucosa: From cranial vertical and middle horizontal part of the para-mesonephric ducts.
- Muscle and serous coat: From surrounding mesenchyma.
➤ Functions:
- Transport of sperm and ovum.
- Site of fertilization.
- Helps in development, survival and transport of zygote
Ovary
Functions of Ovary:
➤ Production of oocytes: During reproductive life about 30 years (from puberty to menopause), the ovaries produce alternately one oocyte per month (per ovarian cycle of 28 days).
➤ Production of hormones (steroidogenesis):
- Oestrogen is secreted by the follicular & paraluteal cyst.
- Progesterone by the luteal cyst.
Anatomy of ovary:
Morphology:
➤ Each gland is oval in shape and pinkish grey in colour and the surface is scarred during reproductive period.
➤ It measures about 3 cm in length, 2 cm in breadth & 1 cm in thickness
➤ Each ovary has 2 ends tubal & uterine, 2 borders mesovarium and free posterior border, and 2 surfaces – medial & lateral.
Structure: The Ovaries have two zones:
➤ Cortex (outer zone): The cortex is covered with germinal epithelium which consists of a single layer of low cuboidal cells but is only seen in earlier life. Later the ovary is coated only by the connective tissue tunica albuginia.
The cortex consists of fibrous tissue stroma with spindle-shaped cells. The primordial and graafian follicles lie there in different stages of development with their derivatives such as corpus luteum and corpus albicantia. Each follicle contains one oocyte. One follicle matures every month and sheds an oocyte. Total 400 oocytes are ovulated in the reproductive life.
➤ Medulla (inner zone): The medulla consists of blood vessels and nerves with a loosely packed fibrous stroma
Blood supply of ovary:
➤ Arterial supply: Is from the ovarian artery, a branch of the abdominal aorta.
➤ Venous drainage: Is through pampiniform plexus, to form the ovarian veins which drain into inferior vena cava on the right side and left renal vein on the left side. Part of the venous blood from the placental site drains into the ovarian veins and thus may become the site of thrombophlebitis in puerperium.
➤ Lymphatic drainage of ovary; Through the ovarian vessels drain to the para-aortic lymph nodes.
➤ Nerve supply of ovary; Sympathetic supply comes down along the ovarian artery from T10 segment. Ovaries are sensitive to manual squeezing
➤ Development of ovary: The ovary is developed from the cortex of the undifferentiated genital ridges by about 9th week; the primary germ cells reaching the site migrating from the dorsal end of yolk sac.
Physiology Of Reproductive System
Sex Hormones:
- Follicular stimulating hormone (FSH) from pituitary gland
- Luteinizing hormone (LH)
- Prolactin
- Estrogen
- Progesterone
- Testosterone
(Ref by: Current Diag & Treatment/13th/135)
Hormones of the Ovary:
- Estrogen
- Progesterone
- Relaxin
- Activin
- Inhibin
- Follistatin
Ref: Current Diag & Treatment/13th/136)
Sources of Estrogen in Female:
- Graaffian follicle
- Corpus luteum
- Adrenal cortex 4. Placenta
(Ref: Current Diag & Treatment/13th/136)
Functions of ovary
A. Production of ovum:
The ovary is associated with the function of maturation, storage and release of ovum
B. Hormone production:
Ovary is associated with a few hormone production like- estrogen, progesterone etc.
(Ref by: D. C. Dutta’s Gynae/7th/11)