Definition of Pain – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Definition of Pain
“Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
Or
An unpleasant sensation that can range from mild, localized discomfort to agony. Pain has both physical and emotional components. The physical part of pain results from nerve stimulation. Pain is a subjective feeling or individual response to noxious stimuli on the sensory nerve endings.

Classification of Pain:
A. According to time:
a) Acute pain; Occurs abruptly after an injury or disease. Persists until healing occurs and often is intensified by anxiety or fear. Examples-Bone fractures, bums, surgery, sickle cell crisis, tension headache, delivery.
b) Chronic pain: Pain lasts for a prolonged period of time. Cannot amenable to specific treatment. It is two types-
1. Chronic nociceptive pain.
- Prolong tissue pathology.
- Stable angina.
- Gastritis.
- Pancreatitis.
- Gout.
2. Chronic neuropathic pain.
- Abnormalities in the PNS or CNS.
- Low back pain.
- Diabetic neuropathy.
B. According to pathophysiology:
a) Nociceptive pain: Pain resulting from activation of primary afferent nociceptors by mechanical, thermal or chemical stimuli.
b) Neuropathic pain: Pain resulting from damage to peripheral nervous or central nervous system tissue or from altered processing of pain in the CNS.
C. According to the origin:
a) Superficial pain: Originate in the skin and subcutaneous tissue.
b) Deep somatic pain: Pain arises from ligament, tendon, blood vessels etc.
c) Visceral pain: Stimulation of pain receptor in the abdominal cavity, cranium and thorax.
D. According to where it is experienced in the body:
a) Radiating pain.
b) Referred pain.
c) Phantom pain.
d) Shifting pain
Factors Influencing Pain in Children:
Physical factors: Many physical factors influence the pain experience, including the individual’s pain threshold, pain tolerance, age, physical activities, nervous-system integrity
Psychological factors: Along with physical factors, several psychological factors can influence the response to pain, including culture, religion, past experience with pain, anxiety and situation factors
Methods of Pain Assessment:
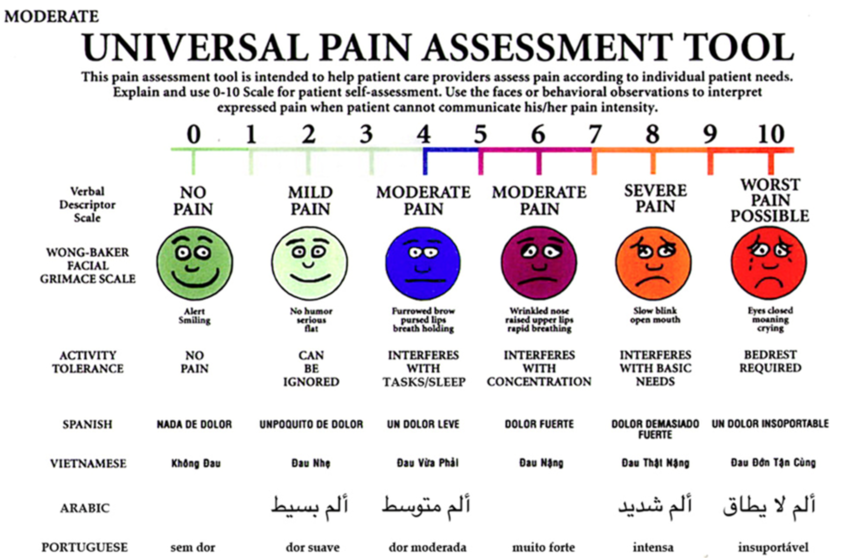
Because pain is both a sensory and an emotional experience, using several assessment strategies provides quality and quantitative information about pain.
QUEST is the best way to assess pain of a children.
Q-Question the child
U- Use a pain rating scale
E- Evaluate the behaviour and physiological changes
S-Secure parents involvement
T – Take cause of pain into account
T – Take action and evaluate results
Management of Pain:
Nurses are essential in pain diagnoses and treatment in all health care settings. They are closest to the patients and their families and provide constant emotional, spiritual and personal support. They have important role in assessing and monitoring pain management.
Methods of pain management;
There are two methods of pain management:
1. Pharmacological method
2. Non-pharmacological method
Pharmacological method;
- Physician should prescribe pharmacologic drugs and nurse should maintain four ‘rights’ right drugs, right dose, right route and right time.
- Non opioids like paracetamol and Non-steroidal anti-inflammatory drugs (NSAIDs) are suitable for mild to moderate pain
- Opioids like morphine is considered-the gold standard for the management of severe pain.
- When morphine is not suitable dromophone, fentanyl can be used.
Non-pharmacological method:
- Pain is often associated with fear, anxiety and stress.
- A variety of non-pharmacologic methods, such as distraction, relaxation, guided imagery and cutaneous stimulation may help reduce pain perception. These techniques enhance comfort, reduce the perceived threat of pain, promote rest and sleep. These methods are safe, noninvasive and inexpensive and nursing functions.
Nursing management of pain:
- The assessment of pain is important to provide an appropriate care.
- Establish relationship between nurse and child
- Nurse should evaluate the pain. Some children may not complain about the pain due to fear of the doctor, drugs or injection.
- AR SONG Observation of children’s behavior changes is important to understand their pain and its cause. An irritability, a specific adopted position, repeated touch to the area, rigid movements and facial expressions of the children give clues about the nature of pain.
- Mother should be stay with their children is very important during the painful state of their children; this may help to reduce stress and discomfort of children.
- To avoid pain nurses should touching, talking, showing television and playing with toy, playing music
- Vital pain should be record after administration.
- Nurses should reposition, support body parts
- Visitor should be restricted.
- Promote rest and Sleep
- Light should lower and noise should be reduced
- Administer medication as order, early in the pain episode
- Medication-Analgesic, NSAIDs eg. Ibuprofen, and analgesic such as morphine, Demerol etc.
- Nurses should assess side’ effect of pain medication, nausea, constipation, respiratory statu urinary retention, and hypotension
- Chronic pain requires a comprehensive approach to manage it effectively
