Definition Of Shock – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level.
In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life.
Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Shock is a medical emergency in which the organs and tissues of the body are not receiving an adequate flow of blood. Shock can result in serious damage or even death.
Or,
Shock is defined as a pathophysiological state in which there is reduced oxygen consumption by the peripheral tissues produced by a reduction in delivery of oxygenated blood or reduced oxygen extraction by the peripheral tissues. It is an acute clinical syndrome by hypo-perfusion, resulting in severe dysfunction of the organs vital survival.
Or,
A shock is a condition of depression of all vital function due to sudden illness, injury, severe hemorrhage.
Or,
Shock is an abnormal physiological condition resulting from inadequate proportion of blood to the aorta thus causes inadequate blood flow per-fusing the capillaries of tissues and organs.
Or,
Shock is a life-threatening condition that occurs when the body is not getting enough blood flow. Many organs can be damaged as a result. Shock requires immediate treatment and can get worse very rapidly.
Definition Of Shock | CHAPTER 21 | Fundamentals of Nursing
Classification of Shock:
The following classifications are given below:
- Primary shock: This occur acting at the time of the accident or sudden illness.
- Secondary shock: This may not develop until several hours after the accident or sudden illness and is unusually very serious.
Another Classification
A. Oligaemic shock:
This occurs when the tissues have been damaged and there is loss of blood or fluid from the circulation. It is very commonly present in the following circumstances-
- Fracture
- Hemorrhage
- Burns and scalds
- After surgical operation
B. Neurogenic shock:
This may happen when no specific injury has taken place but when an emotional upset has occurred. It can occur in the following circumstances
- In state of fear
- In state of high emotion due to bed news
- Due to exposure
- Spinal or head injury
C. Hemorrhagic shock:
Loss of blood due to wounds, Loss of blood due to wounds, internal bleeding, multiple trauma and severe burns
D. Respiratory shock:
There is insufficient amount oxygen in the blood due to inadequate breathing or respiratory arrest.
- Spinal injury
- Obstruction of airways
- Chest trauma
E. Psychogenic shock:
Something psychological affects the patient death of loved one, accident etc.
F. Ardiac shock:
Cardiac muscle not pumping effectively due to injury or previous heart attack. The heart muscle no longer imparts sufficient pressure to circulate the blood
G. Metabolic shock:
Loss of body fluid with a change in biochemical equilibrium and insulin shock diarrhea.
H. Septic shock:
Septic shock is a serious condition that occurs when an overwhelming infection leads to low blood pressure and low blood flow
E. Anaphylactic shock:
Severe allergic reaction of the body to sensitization by a foreign protein.
Sign and Symptoms of All Types of Shock Includes:
- Rapid, shallow or gasping breathing
- Cold, pale, clammy skin.
- Rapid but weak pulse
- Dizziness or fainting
- Weakness, fainting or giddiness and discomfort.
- Eyes appear to stare.
- Pupil are dilated, lusterless of eyes
- Anxiety or restlessness/ agitation
- Seizures
- Confusion or unresponsiveness
- Low or no urine output
- Bluish lips and fingernails
- Profuse sweating, moist skin
- Shaking and trembling of arms and legsunl
- Chest pain
- Nausea, vomiting or extreme thirst
- Blood pressure falls
- Sunken eyes (Lusterless eyes)
- Shaking and trembling of arms and legs
- Generally the patient is very quiet and dustless but it the shock is caused hemorrhage in which patient will be restless and anxious
- Face pale and grey color
- Occasionally cyanosis
- Temperature will be subnormal
- Unconsciousness may be develop
- Evidence of associated external or internal bleeding
Causes of Shock:
A. Common cause
- Heart conditions (heart attack, heart failure)
- Heavy internal or external bleeding, such as from a serious injury or rupture of a blood vessel
- Dehydration, especially when severe or related to heat illness.
- Infection (septic shock)
- Severe allergic reaction (anaphylactic shock) de
- Spinal injuries (neurogenic shock)
- Burns
- Persistent vomiting or diarrhea
- Bleeding
B. Others cause
- Anaphylaxis
- Epidural hematoma
- Carbon monoxide poisoning
- Abdominal aortic aneurysm
- Meningococcemia
- Adult respiratory distress syndrome
- Hereditary angioedema
- Chronic poisoning
- Colitis
- Kwashiorkor
- Caffeine overdose
- Anthrax
- The plague
Complications of shock:
- Acute respiratory distress syndrome
- Acute renal failure
- Gastrointestinal complications
- Disseminated intravascular coagulation
- Multiple organ dysfunction syndrome
Management of Shock:
1. Rest and reassure the patient
2. Keep the person warm and comfortable place.
3. Loosen any tight clothing, remove belt and shoes and cover them with a blanket.
4. Check and control ABCDES:
A-Airway control
B-breathing and ventilation
C-Circulation
D-Disability
E-Exposure with environmental control.
5. If necessary, begin rescue breathing and CPR (Cardiac Pulmonary Resources)
6. If the person is conscious and does NOT have an injury to the head, leg, neck, or spine, place the person in the shock position. Lay the person on the back and elevate the legs about 12 inches (30 centimeters). Do NOT elevate the head. If raising the legs will cause pain or potential harm, leave the person lying flat.

7. Even if the person is able to breathe on his or her own, continue to check rate of breathing at least every 5 minutes until help arrives.
8. Do not move a person who has a known or suspected spinal injury.
9. Open an intravenous (I/V) channel in a large vein and give adequate fluid (normal saline, hartsole, dextrose)
10. If the casualty unconscious and in case of head injury or suspected internal bleeding do not give stimulate.
11. Do not give fluids by mouth, even if the person complain of thirst. There is a choking risk in the event of sudden loss of consciousness.
12. Control bleeding by direct pressure should be applied to any wounds that are bleeding significantly.
13. Give appropriate first aid for any wounds, injuries or illness.
14. Pain should be relieved as fast as possible.
15. Transport as soon as possible to hospital.
Cardiogenic Shock
Cardiogenic shock is a condition in which the heart suddenly can’t pump enough blood to meet the body’s needs. The condition is most often caused by a severe heart attack. Cardiogenic shock is rare, but it’s often fatal if not treated immediately.
Cardiogenic shock signs and symptoms include:
A. Symptoms
As many patients with cardiogenic shock have had an acute MI, symptoms can include:
a) Chest pain
b) Nausea and vomiting
c) Dyspnoea
d) Profuse sweating
e) Confusion/disorientation
f) Palpitations
g) Faintness/syncope
B. Signs
a) Pale, mottled, cold skin with slow capillary refill and poor peripheral pulses.
b) Hypotension (remember to check BP in both arms in case of aortic dissection).
c) Tachycardia/ Bradycardia.
d) Raised JVP/distension of neck veins.emid sugil
e) Peripheral oedema.
f) Heaves, thrills or murmurs may be present and may indicate the cause,
Causes of Cardiogenic Shock:
A. Due to an intrinsic heart problem:
- MI.
- Myocardial contusion (often from steering wheel impact).
- Acute dysrhythmia compromising cardiac output.
- Acute mitral regurgitation (usually as a complication of MI due to ruptured chordae tendinae).
- Ventricular septal rupture (usually occurring as post-MI complication).
- Cardiac rupture (rupture of the wall of the left ventricle can occur post-MI or due to cardiac trauma).
- Hypertrophic obstructive cardiomyopathy or end-stage cardiomyopathy of other cause.
- Myocarditis.
- Post-cardiac surgery requiring prolonged cardioplegia and cardiopulmonary bypass.
- Severe valvular heart disease, particularly aortic stenosis

B. Due to other causes:
- Acute, severe pulmonary embolism (PE).
- Pericardial tamponade or severe constrictive pericarditis.
- Tension pneumothorax.
- Myocardial suppression due to bacteraemia or sepsis (although, strictly speaking, this may be defined as septic shock).
Nursing Management of a Patient With Cardiogenic Shock:
A. Initial management:
a) Administer oxygen by face mask or artificial airway to ensure adequate oxygenation of tissues.
b) Adjust the oxygen flow rate to higher or lower level, as blood gas measurements indicate.
c) Asses vital signs strictly.
d) Assess functioning of ECG monitoring and readings.
B. Administering medications and IV fluids
a) Administer an osmotic diuretic, such as mannitol, if ordered to increase renal blood flow and urine output.
Medications in choice-
- Dobutamine
- Nitroglyserine))
- Dopamine
Vasoactive medications
- Epinephrine
- Nor-epinephrine) по
- Vasopressin
b) Monitor vitals before and after administering medications and IV fluids be Latim stuaA
c) Assess IV infusion site for bleeding or any allergic reaction
d) Monitor-
- Urine output
- BUNslam
- Serum creatinine
C. Strict monitoring-
a) Monitor and record blood pressure, pulse, respiratory rate, and peripheral pulse every 1 to 5 minutes until the patient stabilizes.
b) Record hemodynamic pressure readings every 15 minutes.
c) Monitor ABG values, complete blood count, and electrolyte levels.
d) During therapy assess skin color and temperature and note any changes. Cold and clammy skin may be a sign of continuing peripheral vascular constriction, indicating progressive shock
D. Limit myocardial oxygen demand by-
a) Administer analgesics, sedatives, and other agents as prescribedon • normous laciour.
b) Positioning the patient as comfort.
c) Limiting activities
d) Providing calm and quiet environment
E. Emotional support and health maintenance
a) To ease emotional stress, allow frequent rest periods as possible. a agenam nov lliw woH.O
b) Offering support to reduce anxiety
c) Teaching the patient about his condition.
d) Allow family members to visit and comfort the patient as much as possible.
Septic Shock
Definition of Septic Shock:
Septic shock is a clinical syndrome of life-threatening organ dysfunction caused by a dysregulated response to infection. In septic shock, there is critical reduction in tissue perfusion; acute failure of multiple organs, including the lungs, kidneys, and liver, can occur.
Early symptoms should not be ignored. These include:
- Fever usually higher than 101°F (38°C)usursuni batenim.
- Low body temperature (hypothermia)
- Fast heart rate
- Rapid breathing, or more than 20 breaths per minute
Symptoms of severe septic shock include:
- Noticeably lower amounts of urine
- Acute confusion
- Dizziness
- Severe problems breathing
- Bluish discoloration of the digits or lips (cyanosis)
- Low blood pressure, especially when standing hele biran latiqroli
- Palpitations
- Rapid heart rate
- Restlessness, agitation, lethargy, or confusion
- Shortness of breath
Causes of Septic Shock:
A. Causative organism
- Bacterial infection.
- Fungi, such as candida, and
- Viruses can also sometimes lead to sepsis, although this is rare.
- Bacterial infections that cause sepsis often develop while a person is in hospital. (Hospital Acquired infection)
- Gram-negative bacteria (i.e., Escherichia coli, Klebsiella, Enterobacter, Serratia, Pseudomonas, Bacteroides, Proteus) produce a substance called an endotoxin.
- Gram positive bacteria
B. Endocrine diseases-
- Diabetes
- Adrenal gland failure.
C. Drugs-
- Corticosteroid
- lowod
- Chemotherapy
- Long-use of antibiotics
- Injecting Recreational drugs
- Neuromuscular blocking agent
D. Immune System-
- Cancer AIDS Transplant patient
- Blood diseases
- Lymphoma
- Leukemia
- Disseminated intravascular coagulation (DIC)
E. GIT-
- Liver cirrhosis
- Billiary system infections
- Appendicitis
- Medical devices Drainage tubes
F. Cardiovascular system-
- Valvular heart diseases
G. Nervous system-
- Meningitis
H. Hospital acquired complications-
- DVT
- Lines sepsis
- Bed sores
- Air embolism
Complications of Septic Shock
Septic shock can cause a variety of very dangerous and life-threatening complications that can be fatal. Possible complications include:
- Heart failure
- Abnormal blood clotting
- Kidney failure
- Respiratory failure o
- Strokeruni
- Liver failure
- Loss of a portion of the bowel
- Loss of portions of the extremities

Nursing Management of Septic Shock:
1. Place the patient flat in the bed with the feet elevated if necessary until hypotension is resolved.
2. Avoid the use of Trendelenburg position, as it may increase afterload to the left ventricle and decrease stroke volume. Respiratory excursion is compromised in this position.
3. Maintain 30-45 degree head-of-bed elevation to prevent ventilator-associated pneumonia and aspiration.
4. Obtain a history, examine the patient and make a “best guess”
5. Provide a rapid, cursory initial head-to-toe physical assessment.
6. The initial assessment goal is to identify major problems and gross abnormalities
7. Perform focus assessment of specific injuries or problems after shock is stabilized.
8 . Perform a diagnostic measures .e.g.- ABGs, CBC, Blood culture among
9. Ensure that the airway is protected and maintain a patent airway B = Breathing
10. Assess for the presence of noisy respirations and check for airway obstruction.
11. Auscultate the lung sounds to determine adequate air movement
12. Respiratory rate is considered to be one of the most sensitive indicators of critical illness, yet it is
a vital sign that is often neglected (Stevenson, 2004).
13. Assess the respiratory rate and effort to evaluate the adequacy of breathing, Administer oxygen through face mask and, if intubated, commence mechanical ventilation
14. Restore circulating volume with fluid resuscitation, invasive monitoring and vasopressors if necessary.
15. Palpation of the radial or brachial pulse during deflation of the blood pressure cuff. When palpation is used, the first palpable pulse noted during deflation of the cuff is the systolic BP. Document the BP such as (e.g., 90/palp.)
16. Use of Doppler instrument.
17. By arterial line connected to continuous monitoring.
18. Place the ECG monitor electrodes on the patient’s shoulders than on the chest
19. Temperature monitoring:
- An indwelling flexible rectal probe connected to a continuous display monitor is more accurate and less traumatic than intermittent rectal temperature measurements with a standard thermometer
- Tympanic temperatures are commonly used in critical care setting
✓ Start empiric antimicrobials,. Antibiotics are often started before a diagnosis has been confirmed.
✓ Administer Drotrecoginalfa (activated protein C). It is an artificially produced human protein that can help to prevent inflammation and blood clotting, reducing the risk of death.
✓ Surgery In severe cases of sepsis or septic shock, surgery may be required to remove the dead tissues
Hypovolemic Shock
Definition of hypovolemic shock:
Hypovolemic shock is an emergency condition in which severe blood or fluid loss makes the heart unable to pump enough blood to the body. This type of shock can cause many organs to stop working.
Sign and Symptoms of Hypovolemic Shock:
Signs
A. Early sings litate
- Paleness, excessive sweating (diaphoresis)
- Dilated pupilsalon & mieniam ban batbetomania odiadi surende
- Increased heart rate (tachycardia; may not occur early in patients who take beta-blockers) wom
- Weak, wide pulse,
- Signs of gastrointestinal bleeding: blood in the nose, mouth, throat or rectum (rectal examination)
B. Late signs
- Early signs plus the following:
- Mottled, cyanotic skin
- Increase of tachycardia for at least 30/min upon standing 17 , or
- Decreased or absent urination (<20 mL/hour)
- Coma
Symptoms
A. Early symptoms
- Thirst due to hypovolemia (hypovolemic thirst) can appear after 15% blood loss
- Nausea
- Anxiety, irritability, agitation, sleepiness, confusion
B. Late symptoms
- Dizzinesstodita
- Weakness
- Confusion
- Lethargy
Causes of Hypovolemic Shock:
A number of conditions may cause hypovolemic shock, many of which are serious conditions. This may include:
- Decreased blood clotting ability
- Diarrhea or vomiting
- Excessive sweating (which can result from heat exposure)
- Extremes of age (infants and the elderly may be unable to take fluids)
- Kidney diseases resulting in increased urination
- Ectopic pregnancy (life-threatening pregnancy growing outside the uterus)
- Internal bleeding (often from the gastrointestinal tract, although it can develop elsewhere)
- Large burns
- Ruptured aortic aneurysm (bulging and weakened aortic artery wall that can burst and cause severe hemorrhage) or other vascular abnormalities
- Sepsis (blood infection)
- Serious injury or trauma
Nursing Management of Hypovolemic Shock:
1. Check for patent airway and adequate circulation.
2. Begin an I.V. infusion with normal saline solution or lactated Ringer’s solution delivered through a large bore.
3. Help insert a central venous line and pulmonary artery catheter for hemodynamic monitoring.
4. Insert an indwelling urinary catheter.
5. Draw an arterial blood sample to measure ABG levels.
6. Obtain and record the patient’s blood pressure, pulse and respiratory rates, and peripheral pulse rates.
7. Monitor the patient’s CVP, right arterial pressure, pulmonary artery pressure, and cardiac output at least hourly as ordered.
8. Measure the patient’s urine output hourly.
9. Monitor the patient’s ABG and electrolyte levels frequently as ordered.
10. Watch for signs of impending coagulopathy such as petechiae, bruising, bleeding or oozing from guns or venipuncture site.
11. Explain all procedures and their purposes to ease the patient’s anxiety.
12. Discuss the risk associated with blood transfusions to the patient and his family.
Neurogenic Shock
Neurogenic shock is a life-threatening condition caused by irregular blood circulation in the body.
or
Neurogenic shock is a distributive type of shock resulting in low blood pressure, occasionally with a slowed heart rate, that is attributed to the disruption of the autonomic pathways within the spinal cord.
The common cause of neurogenic shock includes the following
1. Injury or trauma to the spinal cord either blunt or penetrating or which may be caused by a dislocation, rotation and over extension or flexion of the cord. Trauma to the spinal cord may also occur as a result of sport injuries, vehicular accidents, falls and accidents, stab wound and gunshot wound.
2. Neurogenic shock may also occur as a result of regional anesthesia that is improperly liw wolH.O administered.
3. Drugs and medications that can affect the autonomic nervous system may also result in neurogenic shock
4. Improper administration of regional anesthesia can also cause neurogenic shock
Sign and Symptoms of Neurogenic Shock
Primary manifestation may include
- Hypotension
- Bradycardia
- Hypothermia
Other symptoms of shock include the following:
- A rapid and deep shallow breathing a
- Difficulty breathing
- Cold and clammy skin
- Pale skin appearance
- Nausea and vomiting
- Dizziness and lightheadedness
- Fainting
- Rapid and weak pulse
- Weakness is experienced as a result of insufficiency in the blood supply
Nursing Management of Neurogenic Shock:
1. The patient is examined carefully and his/her general condition is assessed thoroughly. Special attention is given to the patient’s airway, breathing pattern and circulation.
2. The patient is examined carefully and his/her general condition is assessed thoroughly.
3.It is important to immobilize the patient, especially the spinal region to prevent any further damage to the spinal cord.
4. Administration of IV fluids is done to stabilize the patient’s blood pressure.
5. Inotropic agents, such as dopamine may be infused for fluid resuscitation, if needed.
6. Atropine is given intravenously to manage severe bradycardia.
7. Patient with obvious neurological deficit can be given I.V. steroids, such as methyl-prednisolone in high dose, within 8 hours of commencement of neurogenic shock.
8.In spinal cord injury, general measures to promote spinal stability are initially used.
9.Definitive treatment of the hypotension and bradycardia involves the use of vasopressors and
atropine respectively. Mande nimaligans to mongine
10. Fluids are administered cautiously as the cause of the hypotension is generally not related to fluid loss.
11. The patient is monitored for hypothermia.hits) Inofail
12. The role of the nurse in neurogenic shock involves-
- Monitoring the patient’s ongoing physical and emotional status to detect subtlechanges in the patient’s condition;
- Planning and implementing nursing interventions and therapy;
- Evaluating the patient’s response to therapy;
- Providing emotional support to the patient and family; and
- Collaborating with other members of the health team when warranted by the patient’s condition.
13. Neurologic status, including orientation and level of consciousness, should be assessed every hour or more often.
14. Heart rate/rhythm, BP, central venous pressure, and PA pressures including continuous cardiac output (if available) should be assessed at least every 15 minutes and PAWP every 1 to 2 hours.
15. Hourly urine output measurements assess the adequacy of renal perfusion and a urine output of less than 0.5 ml/kg/hour may indicate inadequate kidney perfusion.qluq las 16. If a nasogastric tube is inserted, drainage should be checked for occult blood as should stools.
17. Oral care for the patient in shock is essential and passive range of motion should be performedluco testiny three or four times per day.
18. Anxiety, fear, and pain may aggravate respiratory distress and increase the release of catecholamines.
19. The nurse should talk to the patient, even if the patient is intubated, sedated, and paralyzed or appears comatose
Anaphylactic Shock
Anaphylaxis can also be called anaphylactic shock. It is an allergic reaction that can be life-threatening. In most cases, anaphylaxis will mean patient needs to take a trip to the emergency room.
Causes of Anaphylactic Shock:
Common causes include foods such as peanuts, tree nuts (e.g. almonds, walnuts, cashews, and Brazil nuts), sesame, fish, shellfish, dairy products and eggs.
Non-food causes include wasp or bee stings, natural latex (rubber), penicillin or any other drug or injection.
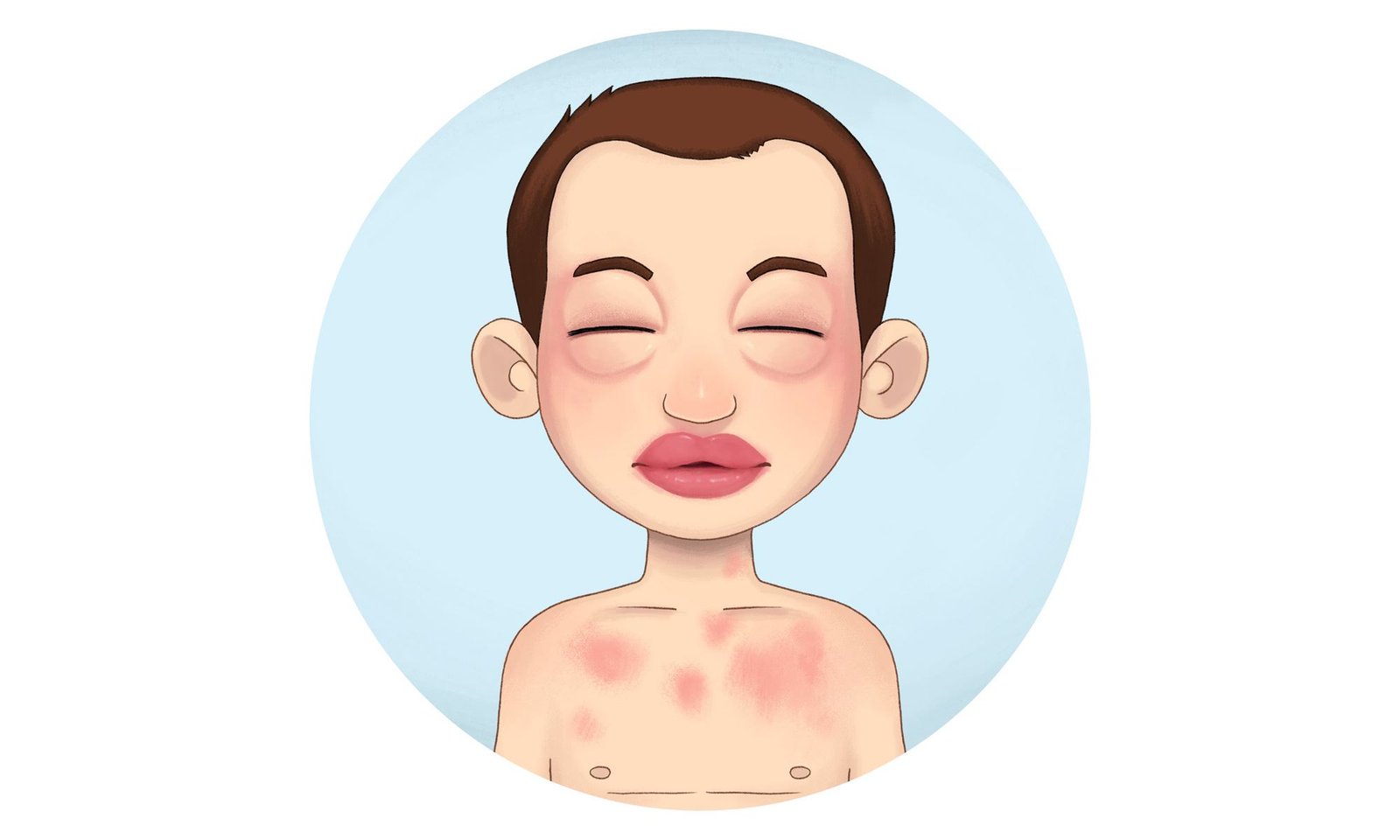
Clinical features/Signs and Symptoms of Anaphylactic shock:
The first signs of an anaphylactic reaction may look like typical allergy symptoms: a runny nose or a skin rash. But within about 30 minutes, more serious signs appear. There is usually more than one of these:
1. Coughing; wheezing; and pain, itching, or tightness in your chest
2. Fainting, dizziness, confusion, or weakness
4. Runny or stuffy nose and sneezing
5. Shortness of breath or trouble breathing and rapid heartbeat
6. Swollen or itchy lips or tongue
7. Swollen or itchy throat, hoarse voice, trouble swallowing, tightness in your throat
8. Vomiting, diarrhea, or cramps
9. Weak pulse, paleness.