All About Viscerotropic – Basic microbiology, parasitology, and immunology; nature, reproduction, growth, and transmission of common microorganisms and parasites in Bangladesh; prevention including universal precaution and immunization, control, sterilization, and disinfection; and specimen collections and examination. Students will have an understanding of common organisms and parasites caused human diseases and acquire knowledge about the prevention and control of those organisms.
Dengue Fever
Dengue is a mosquito born infection which is caused by dengue virus.
Or
Dengue is a viral fever caused by dengue virus
Epidemiological features:
1. Agent: Dengue virus
2. Reservoir: Man and mosquito
3. Transmission cycle: Man mosquito →→ Man
4. Host factors: Age and sex – All ages and both sexes are susceptible
5. Environmental factors: Epidemics often during rainy season and post monsoon.
6. Vector: Mosquito (species of Aedes)
7. Mode of transmission: Female Aedes aegypti mosquito transmits the disease.
8. Incubation period: 2-7 days.
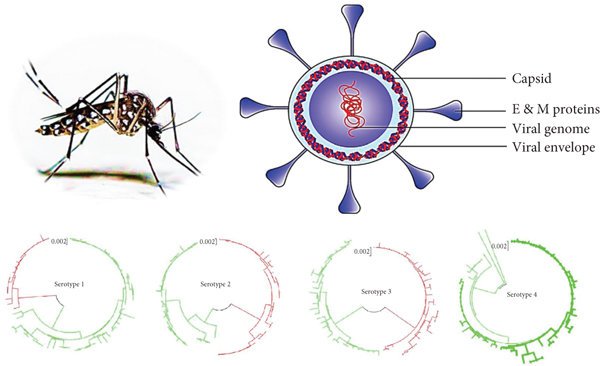
dengue viruses
4 serological types:
1. DEN-1,
2. DEN-2,
3. DEN-3 &
4. DEN-4.
Important Characteristics of Dengue Virus
- RNA virus.
- Enveloped.
- human are reservoir.
- Incubation period 2-7 days
- Cytoplasmic replication.
- Female Aedes aegypti mosquito transmits the disease.
- Viraemia is present at the time of fever.
Prevention of Dengue:
1. Mosquito control: the vectors of DF and DHF breed in and around the house,
A. Anti-larval measures
a) Environment control (source reduction): The environment should be cleaned up and got rid of water holding containers such as discarded tins, empty pots, and broken bottles and similar other artificial collection of water.
b) Chemical control: Larviciding – temophos (abate) can be freely used in water collection
B. Anti-adult measures: Residual sprays
C. Protection against mosquito bites:
a) Use of Mosquito net
b) Use of Mosquito repellents (Diethyltolenamide)
2. Notification: Occurrence of epidemics needs to be reported
3. Appropriate treatment of DF and DHF.
4. Vaccine:
A. A live attenuated vaccine effective against all 4 strains of the dengue virus
B. Clinical traits in adult volunteers have shown the vaccine to be safe and the immunological response to be encouraging.
Outcomes of Dengue Virus Infection:
1. Infection may be asymptomatic
2. Spontaneous recovery
3. Dengue haemorrhagic fever.
4. Dengue shock syndrome.
5. Other complications –
- DIC.
- Hepatitis.
- Encephalitis.
- Myocarditis.
- Cerebral haemorrhage or oedema,
Dengue Haemorrhagic Fever:
It is a much more severe disease than classical dengue fever, with a fatality rate that approaches 10%.
Clinical Picture:
Dengue haemorrhagic fever (DHF) is characterized by –
- Initially the picture is same as classical dengue.
- Then haemorrhage (especially skin and GIT) and shockim
Laboratory Findings
- Thrombocytopenia (platelet count < 1, 00,000/ cu mm of blood).
- Rise of the haematocrit > 20%.
Pathogenesis of Dengue Fever;
1. Classical dengue fever (First exposure of dengue virus);
gniti Dengue infection by one of the four serotypes -> Antibody is formed -> ation of immune complex & activation of complement -> Increased vascular permeability and thrombocytopenia.
2. Dengue haemorrhagic fever (Re-exposure of dengue virus);
Patient infected with another serotype of dengue virus -> An anamnestic, heterotypic response occurs -> arge amount of cross-reacting antibody to the first serotype are produced -> There are two hypotheses about what happens next-
- Immune complexes composed of virus and antibody are formed that activate complement, causing increased vascular permeability and thrombocytopenia. Ultimately shock and haemorrhage result.
- Antibodies increase the entry of virus into monocytes and macrophages with the consequent liberation of a large amount of cytokines. Ultimately shock and haemorrhage result.
Dengue Shock Syndrome;
Dengue shock syndrome is a presentation of dengue syndrome when a case of dengue manifests circulatory failure with one or more of following features:
1. Hypotension for age
2. Cold clammy skin, restless, rapid weak pulse
3. Narrow pulse pressure
4. Profound shock
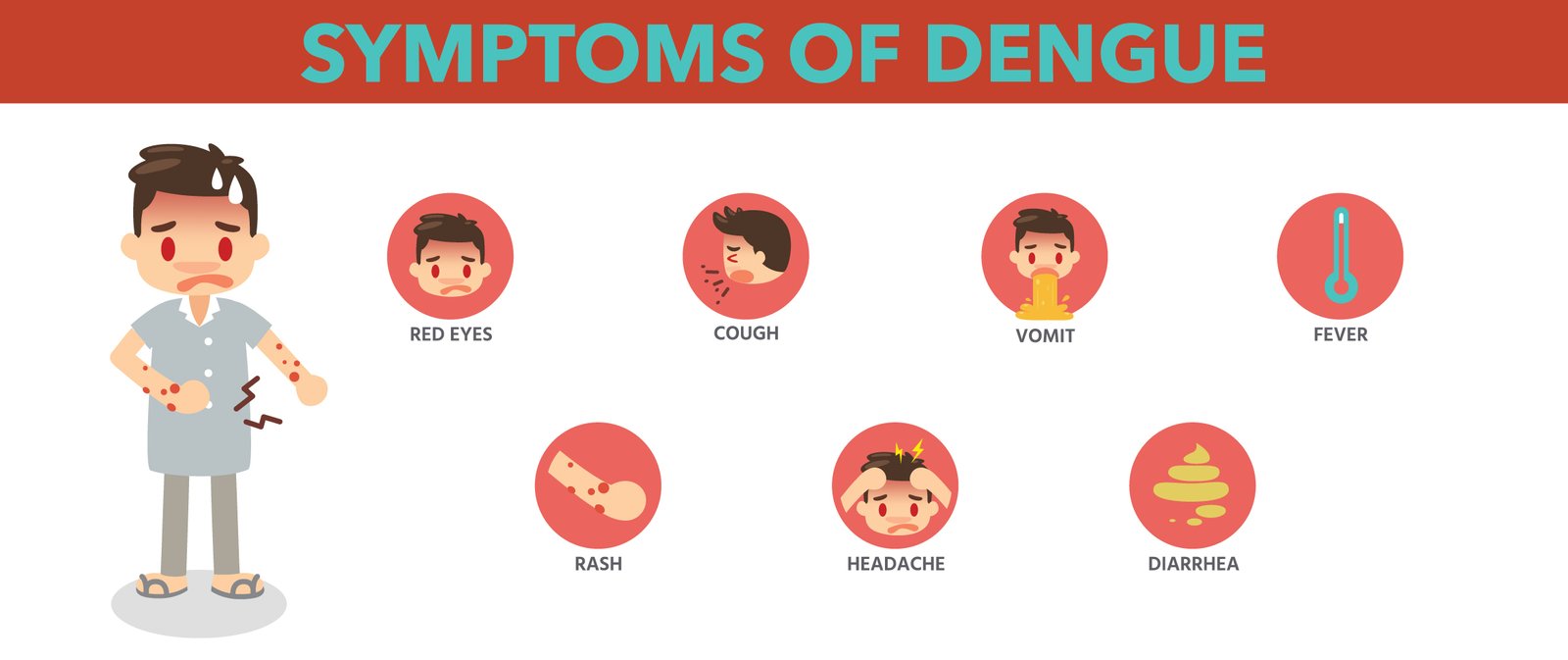
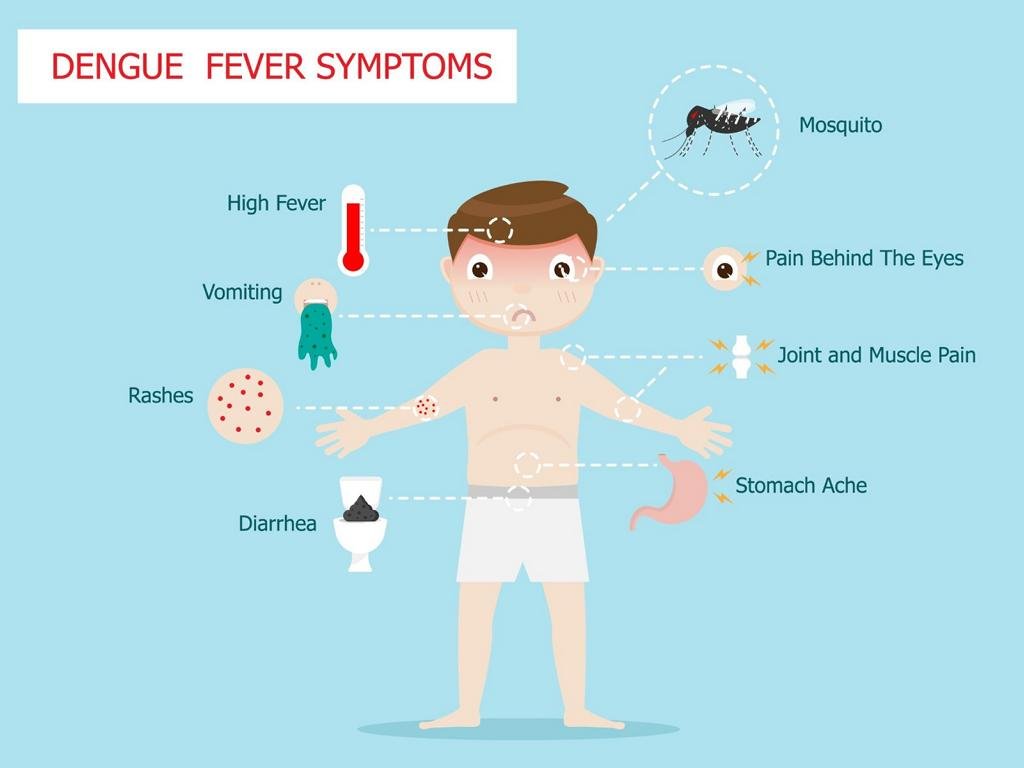
Clinical Features:
A. Prodromal (2 days): Malaise, Headache
B. Acute:
- Fever: Acute onset, high, continuous or, saddle back, with break on 4-5th day and lasting 2-8 days
- Headache, backache, arthralgia
- Generalized pain-break bone fever
- Pain on eye movement, lacrimation
- Anorexia, nausea, vomiting
- Depression
- Relative bradycardia
- Lymphadenopathy
- Rash transient macular in first 1-2 days
- Maculopapular, scarlet
- From 3-5th day on trunk, spreading centrifugally sparing palm and sole
- May desquamate on resolution
- Prostration
- Scleral injection fitna
C. Convalescence – slow
D. Any of the following hemorrhagic manifestation: Petechiae, purpura, echymosis, epistaxis,gum bleeding and haematemesis
E. Features of shock – manifested by
- Sweating on forehead
- Rapid thread pulse
- Hypotension
- Shallow breathing
- Cold clammy skin
- Restlessness
- Oliguria
Management of DHF:
a) Management of DHF during the febrile phase is similar to that of DE
b) Oral electrolyte solution of fruit juice is recommended during the febrile phas
c) Monitor
- Platelet count and HCT value should be estimated at least daily.
- Frequent recording of vital signs is recommended for adjusting replacement avoiding over hydration
d) Fluid therapy: A rise of hematocrit of 20 or more indicates the need for IV fluids therapy
- Ringers lactate solution
- 0.9% W/V normal saline
- 5% dextrose in half strength normal saline solution
e) lood transfusion: In case of significant severe bleeding
f) Shock: In case of shock give oxygen
g) Acidosis: For acidosis use sodium bicarbonate
h ) Evaluation of patients condition
- Frequent recording of vital signs
- Pulse, BP, respiration and temperature every 30 minutes
- Monitoring of urine output
- Platelet court and haematocrit determination
- Haematocrit level 2 hours for first 6 hours then every 4 hours
- Fluid balance sheet
Nursing Interventions of Dengue Fever
Nursing interventions appropriate for a patient with DHF include:
- Blood pressure monitoring: Measure blood pressure as indicated
- Monitoring pain: Note client report of pain in specific areas, whether pain is increasing, diffused, or localized.
- Vascular access: Maintain patency of vascular access for fluid administration or blood replacement as indicated.
- Medication regimen: There must be a periodic review of the medication regimen of the client to identify medications that might exacerbate bleeding problems.
- Fluid replacement: Establish 24-hour fluid replacement needs.
- Managing nose bleeds: Elevate position of the patient and apply ice bag to the bridge of the nose and to the forehead.
- Trendelenburg position: Place the patient in Trendelenburg position to restore blood volume to the head.
Complications:
➤ High fever
➤ Damage to the lymphatic system
➤ Damage to blood vessels
➤ Bleeding from the nose
➤ Bleeding under the skin
➤ Internal bleeding
➤ Bleeding from the gums
➤ Liver enlargement
➤ Circulatory system failure

Grading the severity of the DHF:
1. Grade-I: Fever accompanied by nonspecific constitutional symptoms the only hemorrhagic manifestation is appositive tourniquet test.
2. Grade-II: Above sign plus spontaneous bleeding
3. Grade-III: Above sign plus circulatory failureoid
4. Grade -IV: Profound shock: undetectable BP and pulse
(Grade III and Grade IV known as DSS)
Clinical laboratory investigation in DHF
- Haematocrit – increase 20%
- Platelet count – Thrombocytopenia
- WBC count and DC
- Coagulograme: PT, partial thromboplastin time, fibrinogen level and fibrinogen egradate products
- Serum protein particularly albumin
- Liver function tests.
- Serum electrolyte particularly sodium
- Blood gas analysis
- Renal function and urine examination
- Serum complements
- Stool examination OBT
- ECG
- Chest X-ray
- USG of abdomen
- CSF. Plus
- Diagnosis for dengue – virus isolation and serology (IgM and IgG)
Laboratory Diagnosis of Dengue Haemorrhagic Fever:
Principle:
The diagnosis can be made in the laboratory either by isolation of the virus in cell culture or by serologic tests that demonstrate the presence IgM antibody or a fourfold or greater rise in antibody titer in acute and convalescent sera. A PCR assay that detects virus in the blood is also available.
Routine blood test is also helpful.
Specimen collection:
➤ Blood
Isolation: By cell culture.
Scrological test:
➤ Antibody detection:
- ELISA.
- ICT (Immuno chromatography test).
- Immuno blot (western blot).
➤ Antigen detection :
- Fluorescence microscopy in tissue.
- EIA in blood and plasma.
➤ Nucleic acid based technique:
- Polymerase chain reaction (PCR).
➤ Routine blood test:
- Platelet count: Reduced
- Haematocrit: Low or high