Diarrheal diseases – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Diarrheal diseases

Diarrhea, also spelled diarrhea, is the condition of having at least three loose or liquid bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin with loss of the normal stretchiness of the skin and irritable behavior.
This can progress to decreased urination, loss of skin color, a fast heart rate, and a decrease in responsiveness as it becomes more severe. Loose but non-watery stools in babies who are breastfed, however, may be normal.
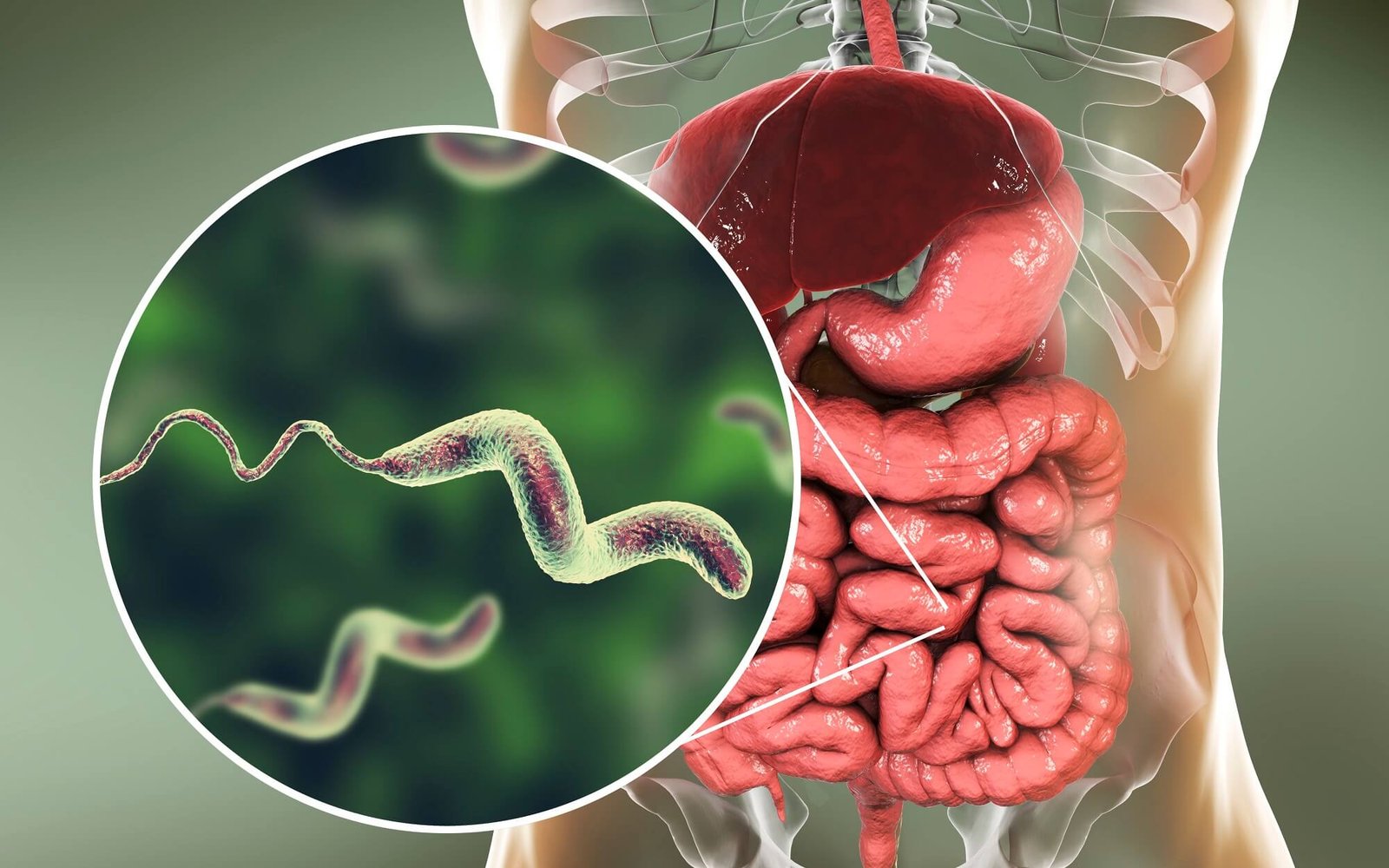
The most common cause is an infection of the intestines due to either a virus, bacteria, or parasite; a condition known as gastroenteritis. These infections are often acquired from food or water that has been contaminated by stool, or directly from another person who is infected.
It may be divided into three types: short duration watery diarrhea, short duration bloody diarrhea, and if it lasts for more than two weeks, persistent diarrhea. The short duration watery diarrhea may be due to an infection by cholera, although this is rare in the developed world.
If blood is present it is also known as dysentery. A number of non-infectious causes may also result in diarrhea, including lactose intolerance, irritable bowel syndrome, non-celiac gluten sensitivity, celiac disease, inflammatory bowel disease, hyperthyroidism, and a number of medications. In most cases, stool cultures are not required to confirm the exact cause.
Definition of Diarrhea
Diarrhea is defined as the passage of loose, liquid or watery stools, more than three times per day.
Or
Diarrhea is defined as the passages of loose watery stool more than 3 times a day.
Or
Diarrhea can be defined as increased stool frequency and lose of watery stool.
(Ref; Paediatric Nursing, Parul Datta/3/274)
Type of Diarrhea
A. According to duration
Acute diarrhea (<2 weeks)
Chronic diarrhea (<2 Weeks or longer)
B. Clinical classification
- Acute watery diarrhea (lasting for few hour to day)
- Invasive diarrhea (visible blood with stool)
- Persistent diarrhea: (<2 weeks or longer)
C. According to causative agent
- Infective
- Non-infective
D. Pathological diarrhea
- Osmotic diarrhea
- Secretory diarrhea
- Inflammatory diarrhea
- Abnormal motility
(Ref by-Davidsons/22nd/306)
FOR SAQ
Causes of Acute Watery Diarrhea in Young Children Arc-
- Rota virus.
- Vibrio cholerae
- Salmonella.
- Enterotoxegenic E. Coli.
- Shigella.
- Campylobacter jejuni.
- Entero-pathogenic E. coli
- Cryptosporidium
(Ref-M. R. Khan 156/3rd/edition)
FOR EQ
Common Causes of Diarrhea
A. Invasive
a) Bacterial
- Shigella species
- Entero-hemorrhagic E – Coli
- Entero invasive E-coli
- Salmonella typhi
- Vibro parahaemolyticus
- Escherichia enterocolitica
b) Parasitic
- E-Histolytica
- Giardia intestinalis
- Cryptosporidium
B. Non-invasive
a) Bacterial
- V. cholera:
- Entero-toxigenic E. coli
- Enterophathogenic E. coli
- Enterotoxin of staphylococcus aureus
- Enterotoxin of bacillus cereus
- Enterotoxin of clostridium perfringens type A
b) Viral
- Rota virus
- Norwalk
Signs and Symptoms of Diarrhea
Kids often get crampy abdominal pain first, followed by diarrhea that usually lasts no more than a few days. Infections with the viruses, bacteria, and parasites that lead to diarrhea also can cause:
- Peeing less often (fewer wet diapers)
- Acting fussy or irritable
- Dry mouth
- No tears when he cries
- Unusual drowsiness or sluggishness
- Sunken soft spot on the top of the baby’s head
- Skin that isn’t as elastic as usual (doesn’t spring back when you gently pinch and release it)
- Fever of 102°F degrees or higher
- Belly pain
- Blood or pus in his poop, or poop that’s black, white, or red
- Sluggishness
- Vomiting
Management of Diarrhea:
Principle the management of acute diarrhoea
1. Fluid replacement
2. Antibiotics/antimicrobial therapy
3. Adjunctive antidiarrheal therapy.
4. Give the child plenty of food to prevent under-nutrition:
A. Fluid replacement
Replacement of established deficit.
- Replacement of ongoing loses.
- Replacement of normal daily requirement (1 – 1.5 litres/day) or provide breast feeding.
B. Management of dehydration
1. Prevention by Home-based fluids
2. Rehydration by
a) Oral Rehydration Therapy (ORT):
- Oral Rehydration Salts (ORS)
- New Formulation
b) Intravenous rehydration :
Initial management of severe dehydration
Failure of ORT:
✓ Intractable vomiting
✓ High purging rate
✓ Inability to drink
- Continued Feeding
- Administration of zinc
C. Antimicrobial agents: According to cause
1. Amoebic dysentery – Metronidazole or Tinidazole, Diloxanide furoate.
2. Vibrio cholerae – Tetracycline or doxycycline
3. Bacillary dysentery – Ciproflaxacin, azithromycin.
D. Antidiarrhoeal, antimotility and antisecretorv agents
1. Not recommended in acute infective diarrhoea and their use may even be contraindicated
E. Give the child plenty of food to prevent under-nutrition:
1. Continue to breast-feed frequently.
2. If the child is not breast-fed, give the usual.milk.
3. If the child is 5 months or older, or already taking solid food:
- Also give cereal or another starchy food mixed, if possible, with pulse-vegetables and meat or fish
- Add 1 or 2 tea spoon full of vegetable oil to each serving.
- Give fresh fruit juice or mashed banana to provide potassium.
- Give fresh the prepared foods.
- Encourage the child to eat: offer food at least 6 times a day.
- Give the same food after diarrhea stops, and give an extra meal each day for two weeks.
Nursing Interventions of Diarrhea:
1. Restoring fluid and electrolyte balance by ORS, IV fluid therapy, intake and output recording and checking of vital signs.
2. Prevention of spread of infection by good hand washing practices, hygienic disposal of stools, care of diapers, general cleanliness and universal precautions,’
3. Preventing skin breakdown by frequent change of diaper, keeping the perianal area dry and clean, avoiding scratching and rubbing of irritated skin and use of protective barrier cream.
4. Providing adequate nutritional intake by appropriate dietary management.
5. Reducing fear and anxiety by explanation, reassurance, answering questions and providing necessary information
6. Giving health education for prevention of diarrhea home management of diarrheal diseases, importance of ORS, dietary management, hygienic practices, medical help, etc.
(Ref by: Paediatric Nursing, Parul Datta/3/277)
Complications of Diarrhea;
- Electrolyte imbalance
- Growth failure
- Renal shut down
Prevention of Diarrhoea;
1. Sanitation:
- Improved water supply
- Improved excreta disposal
- Improved domestic and food hygiene.
2. Breast feeding and weaning practice:
- Encouragement to other for giving colostrum to the new born infant.
3. Use of sanitary latrine:
- Human faeces contain various kinds of bacteria and parasite. So for proper disposal everyone should use sanitary latrine.
4. Personal hygiene;
- Compulsory washing of hands before handing food items and after defecation to protect family member.
5. Water for drinking and domestic-use: It should be free from faecal contamination.
6. Vaccine against rotavirus
7. Immunization against measles
8. Health education
9. Fly control.
ORS. (ORAL REHYDRATION SALTS)
Definition of ORS:
Oral rehydration salts or ORS is a solution of glucose-based salt solution used in oral rehydration therapy.
Composition of ORS:
| NaCI | 1.30 g |
| KCI | 0.75 g |
| Trisodium citrate | 1.45 g |
| Glucose anhydrose | 6.75 g |
Use of ORS:
- Correction of ‘No sign’ dehydration &
- Some sign dehydration.
Roles of ORS in Diarrheal Disease:
1. It has a vital role for correction of dehydration.
2. Glucose facilities absorption of Na* and water in the intestine.
3. Water is required to prevent dehydration.
4. Na and K’ needed to replace the body loss of these ions during diarrhea.
5. Bicarbonate and citrate corrects acid base balance
Composition of Rice Saline:
| Rice powder | 50 g |
| NaCI | 3.5 g |
| KCI | 1.5 g |
| NaHCO3 | 2.5 g |
| Water | 1100 m |