Definition of Pancreatitis – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Definition of Pancreatitis
Disease of Pancreas
A. Congenital:
- Aplasia, Hypoplasia, Hyperplasia, Hypertrophy, Dysplasia
- Variations and anomalies of the duct: Pancreas divisum, Rotation anomalies
- Annular pancreas
- Pancreatic gallbladder
- Polycystic disease
- Congenital pancreatic cysts, cystic fibrosis
- Ectopic pancreatic tissue, accessory pancreas
- Vascular anomalies
- Choledochal cysts
- Horseshoe pancreas
B. Acquired:
- Trauma-penetrating, blunt, iatrogenic
- Pancreatitis: Acute and chronic pancreatitis
- Pancreatic tumors
Definition of Pancreatitis:
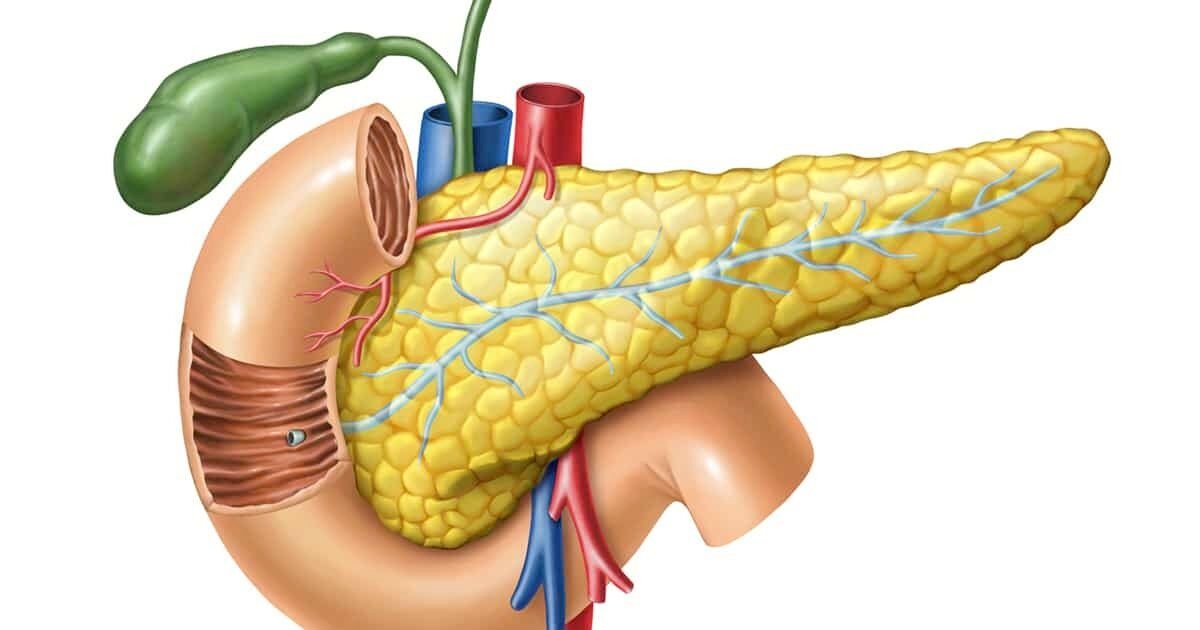
Pancreatitis is inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types, acute pancreatitis and chronic pancreatitis. Signs and symptoms of pancreatitis include-
- Pain in the upper abdomen,
- nausea and vomiting
Or,
Pancreatitis, which is the inflammation of the pancreas, can be acute or chronic in nature. It may be caused by edema, necrosis or hemorrhage.
Causes of Acute Pancreatitis:
A. Major causes:
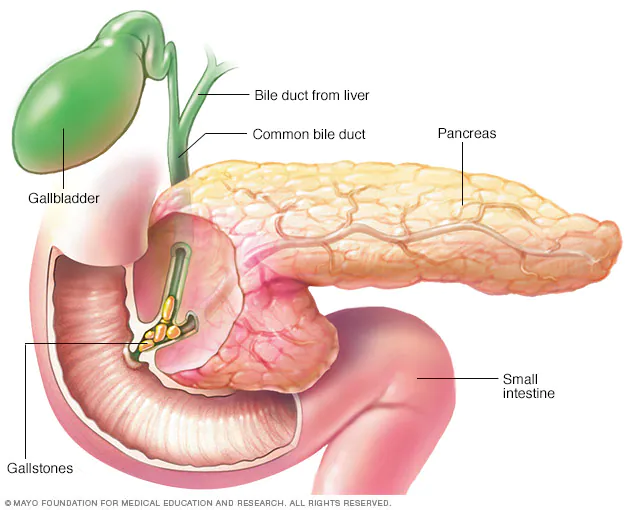
a) Biliary calculi (50-70% causes)
b) Alcohol abuse (25% cases)
B. Rare causes:
a) Gallstone:
- Bile reflux (common channel)
- Pancreatic duct hypertension or obstruction
- Reflux of infected fluid
- Reflux of activated enzyme
b) Ischemia:
- Hypoxaemia
- Free radical production
- Vascular endothelial injury
c) Drug induced: Direct toxicity, Altered secretions
d) Hyperparathyroidism: Accelerated conversion of trypsinogen to trypsin
e) Hyper-calcaemia: Calculus formation, Direct toxicity, Disordered secretion
f) Trauma: Disruption of parenchyma or ducts
g) ERCP: Ductal disruption and enzyme disruption
h) Mechanical obstruction: Ductal hypertension
i) Pancreas divisum: Ductal obstruction
j) Hereditary: Abnormal trypsinogen stability
Classification of Pancreatitis:
The most basic classification system divides the disorder into acute and chronic forms.
1. Acute pancreatitis. Acute pancreatitis does not usually lead to chronic pancreatitis unless complications develop.
2. Chronic pancreatitis. Chronic pancreatitis is an inflammatory disorder characterized by progressive destruction of the pancreas.
Pathophysiology of Pancreatitis:
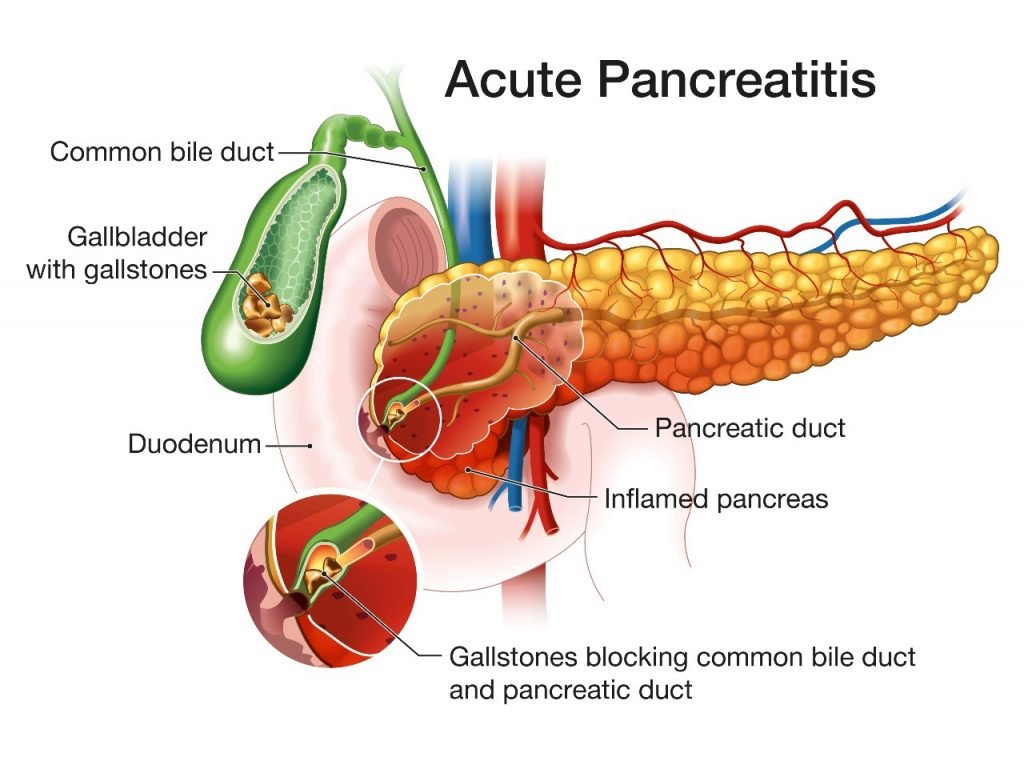
Self-digestion of the pancreas caused by its own proteolytic enzymes, particularly trypsin, causes acute pancreatitis.
- Entrapment. Gallstones enter the common bile duct and lodge at the ampulla of Vater.
- Obstruction. The gallstones obstruct the flow of the pancreatic juice or causing a reflux of bile from the common bile duct into the pancreatic duct.
- Activation. The powerful enzymes within the pancreas are activated.
- Inactivity. Normally, these enzymes remain in an inactive form until the pancreatic secretions reach the lumen of the duodenum.
- Enzyme activities. Activation of enzymes can lead to vasodilation, increased vascular permeability, necrosis, erosion, and hemorrhage.
- Reflux. These enzymes enter the bile duct, where they are activated and together with bile, back up into the pancreatic duct, causing pancreatitis.
Management of Acute Pancreatitis:
Clinical features:
a. Symptoms:
- Sudden onset of upper abdominal
- Nausea, vomiting, fever
b. Sign:
- Patient is toxic and lies in Mohammedans praying position
- Bruise or ecchymosis in the loin
- Upper abdomen is tender and rigid
- Jaundice may be present
- Sign of left sided pleural effusion
- Signs of shock in severe cases, eg.
✔ Sweating
✔ Tachycardia
✔ Hypotension
✔ Arrhythmia
✔ Renal failure
Investigation:
- Routine blood examination
- Serum amylase – High level is diagnostic
- 24 hours urinary amylase
- Plain X-ray of abdomen
- X-ray of chest (may show pleural effusion 5-10%)
- USG (confirmatory) defect
- CT scan
- HIDA scan
- Peritoneal aspiration
- Laparatomy
Treatment:
a. Treatment of shock (if present):
- IV fluid
- Plasma
- Blood (according to input output cahrt)
b. Supportive treatment:
- Complete bed rest
- Nothing per oral (NPO)
- Nasogastric suction
- Intravenous fluid
- Electrolyte replacement
- Analgesic
- Nutritional support
- Antibiotic
c. For rest of pancreas:
- Restriction of all food by moth
- NG suction
- Inj. atropine to reduce secretion
d. Surgery: The options are –
- Sphincterotomy by ERCP – If obstruction in the ampulla of vater
- Pancreatic lavage – In necrotizing pancreatitis
- Laparotomy-total or partial pancreatectomy
Nursing Management of Pancreatitis:
Nursing Assessment
Nursing assessment of a patient with pancreatitis involves:
- Assessment of current nutritional status and increased metabolic requirements.
- Assessment of respiratory status.
- Assessment of fluid and electrolyte status.
- Assessment of sources of fluid and electrolyte loss.
- Assessment of abdomen for ascites.
Nursing Diagnosis
Based on the assessment data, the nursing diagnoses for a patient with pancreatitis include:
- Acute pain related to edema, distention of the pancreas, and peritoneal irritation.
- Imbalanced nutrition: less than body requirements related to inadequate dietary intake, impaired pancreatic secretions, and increased nutritional needs.
- Ineffective breathing pattern related to splinting from severe pain, pulmonary infiltrates, pleural effusion, and atelectasis.
Planning & Goals
Planning and goals developed for a patient with pancreatitis involves:
- Relief of pain and discomfort.
- Improvement in nutritional status.
- Improvement in respiratory function.
- Improvement in fluid and electrolyte status.
Nursing Interventions
Performing nursing interventions for a patient with pancreatitis needs expertise and efficiency.
- Relieve pain and discomfort. The current recommendation for pain management in this population is parenteral opioids including morphine, hydromorphone, or fentanyl via patient- controlled analgesia or bolus.
- Improve breathing pattern. The nurse maintains the patient in a semi-Fowler’s position and encourages frequent position changes.
- Improve nutritional status. The patient receives a diet high in carbohydrates and low in fats and proteins between acute attacks.
- Maintain skin integrity. The nurse carries out wound care as prescribed and takes precautions to protect intact skin from contact with drainage.
Evaluation
Evaluation of a successful plan of care for a patient with pancreatitis should include:
- Relieved pain and discomfort.
- Improved nutritional status.
- Improved respiratory function.
- Improved fluid and electrolyte status.
Discharge and Home Care Guidelines
A prolonged period is needed to regain the strength of a patient who has experienced pancreatitis and to return to the previous level of activity.
- Teaching. Teaching needs to be repeated and reinforced because the patient may have difficulty in recalling many of the explanations and instructions given.
- Prevention. The nurse instructs the patient about the factors implicated in the onset of pancreatitis and about the need to avoid high-fat foods, heavy meals, and alcohol.
- Identification of complications. The nurse should give verbal and written instructions about the signs and symptoms of pancreatitis and possible complications that should be reported promptly to the physician.
- Home care. The nurse would be able to assess the patient’s physical and psychological status and adherence to the therapeutic regimen.
Complication of Acute Pancreatitis:
A. Systemic complication: (more common in 1″ weeks)
a. Cardiovascular system (CVS): Shock, arrhythmia
b. Pulmonary: ARDS (adult respiratory distress syndrome)
c. Renal failure
d. Hematological: DIC
e. Metabolic: Hypocalcaemia, Hyperglycemia, Hyperlipidemia
f. Gastrointestinal: Ileus
g. Neurological:
- Visual disturbance
- Confusion, irritability
- Encephalopathy
h. Miscellaneous:
- Subcutaneous fat necrosis
- Arthralgia
B. Local complication (usually develop after the 1″ weeks): B
- Acute fluid collection
- Sterile pancreatic necrosis
- Infected pancreatic necrosis
- Pancreatic abscess
- Pseudocyst
- Pancreatic ascites
- Pleural effusion
- Portal/splenic vein thrombosis
- Pseudoaneurysm
