Ectopic pregnancy – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Ectopic pregnancy
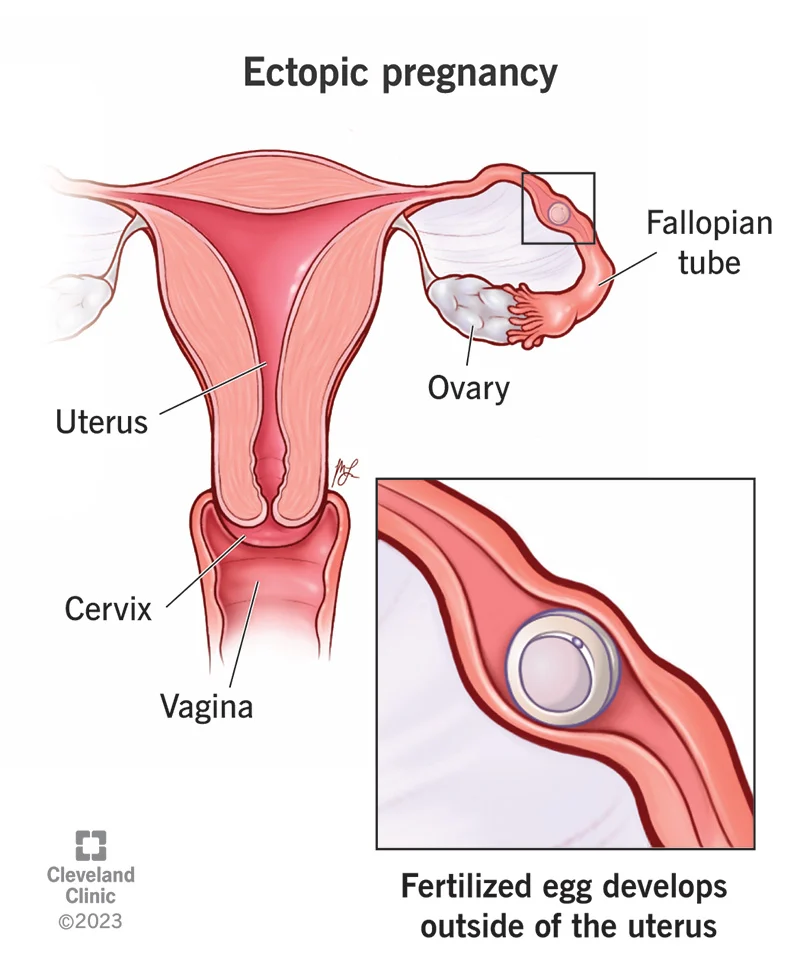
An ectopic pregnancy is on in which the fertilized ovum becomes implanted in a site other than the normal uterine cavity.
Or
Implantation of fertilized ovum in a location outside of the uterine cavity, including the fallopian tubes, cervix, ovary, cornula region of the uterus, and the abdominal cavity.
Or
Ectopic pregnancy, also known as tubal pregnancy, is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically. include abdominal pain and vaginal bleeding.
Or
An ectopic pregnancy occurs when a fertilized egg implants somewhere other than the main cavity of the uterus. Normally, the fertilized egg attaches itself to the lining of the uterus.
Common sites of ectopic pregnancy:
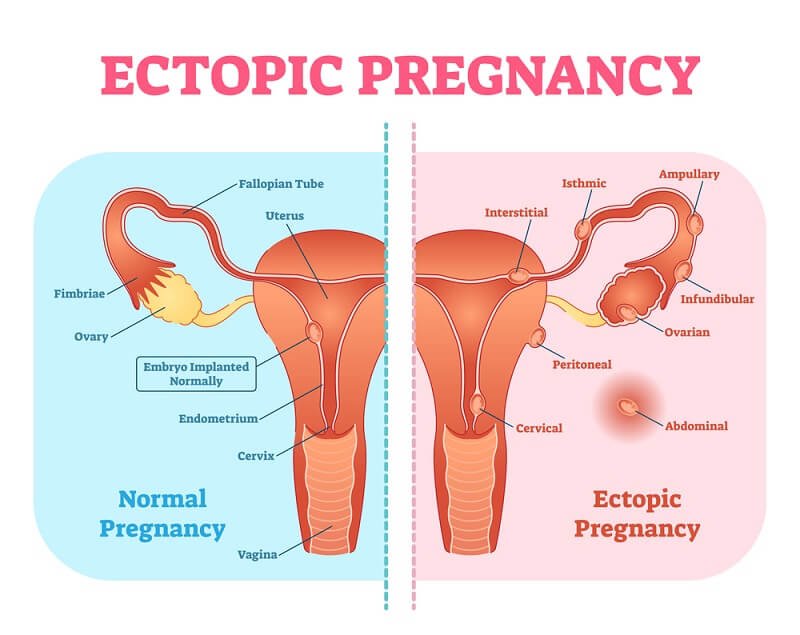
Fig: Sites of ectopic pregnancy. Sites and frequencies of ectopic pregnancy. (By Donna M. peretin, RN.)
a. Ampullary, 80%;
b. Isthmic, 12%;
c. Fimbrial, 5%;
d. Cornual/Interstitial, 2%;
e. Abdominal 1.4%
f. Ovarian, 0.2%;
g. Cervical, 0.2%.
Common Sites of Ectopic Pregnancy:
The common sites of ectopic pregnancy are:
1. Fallopian tube-most common
- Ampulla
- Isthmus
- Fimbria
- Interstitial
2. Ovary
3. Abdominal cavity
- Primary- when fertilized ovum is primarily implanted into the abdominal cavity
- Secondary- when tubal rupture occur and implantation occur in the abdominal cavity
4.. Cervix
5. Broad ligament
6. Very rarely in different sites of uterus like– corneal, rudimentary horn, angular, intramural
Causes/Aetiology of Ectopic/Tubal Pregnancy:
Multiple factors contribute to the relative risk of ectopic pregnancy. In theory, anything that hampers the migration of the embryo to the endometrial cavity could predispose women to ectopic gestation. The most logical explanation for the increasing frequency of ectopic pregnancy is previous pelvic infection; however, most patients presenting with an ectopic pregnancy have no identifiable risk factor. 40% of EPs have an unknown etiology.
The Aetiological Factors:
A. Tubal factors:
1. Pelvic inflammatory disease causing tubal adhesion
2. Tubal pathology
◊ Tubular infection-
- Chlamydia trachomatis infection
- STD
- Post abortal (septic abortion)
- Post puerperal 5. Tubercular
- Post-operative
- Abnormal peristalsis of the tube
- Salpingitis isthmicanodosum
◊ Abnormal peristalsis
3. Congenital abnormality of the tube:
- Undue tortuosity
- Diverticula
- Accessory lump
- Hypoplasia
4. Endometriosis
5. Surgery of the tube:
- Tubal ligation
- TAH within 48 hour of coitus
- Tuboplasty
6. Distortion of the tube by adjacent large tumor
7. Operation in pelvis in and around uterus/ovary
B. Ovarian factor:
1. Fertilization of an un-extruded ovum
2. Ovarian enlargement due to prolong use of ovulation induction drug like clomiphene
C. Zygote abnormalities:
1. Chromosomal abnormalities
2. Abnormal spermatozoa
D. Exogenous hormones:
1. Progesterone only pill
2. Morning after pill
E. Others:
1. Cigarette smoking
2. Hamper tubal motility
3. Hamper cilliary motility
4. In vitro fertilization
5. IUCD
6. External migration of ovum
7. Increasing age
[Ref by-Jeffcoate/7th]
Outcome of Tubal Pregnancy:
Tubal abortion:
Discharge of ovum into the lumen after rupture of the fallopian tube. It may result in the following
- Complete abortion
- Incomplete abortion
- Complete absorption
- Missed abortion- tubal mole
Tubal rupture:
- Intra peritoneal rupture
- Extra peritoneal rupture
For fetus Death:
After death fetus may be –
- Absorbed completely
- May be mummified
- May be calcified
- May be infected
- Adipocerous formation may occur
Survival to term: Very rare
Risk Factors of Ectopic Pregnancy:
1. Pelvic inflammatory disease (6 fold increased risk)
2. Use of IUCDs (3-5% increased risks)
3. Smoking (2.5% increased risks)
4. ART pregnancies (3-5% increase risks)
5. Tubal damage (surgical occlusions or cilial damage)
6. Tubal surgery (5.8% increased risks)
7. Salpingitis isthimica nodesa (3.5% increased risk)
8. Prior ectopic pregnancy (10 fold increased risks)
9. Age risk of ectopic is 3 fold greater in women of 35-44 years as compared to 18-24 years)
10. Non-white race (1.5 fold increased risk)
Management of Acute Rupture Ectopic Pregnancy:
A. Diagnosis:
Clinical features:
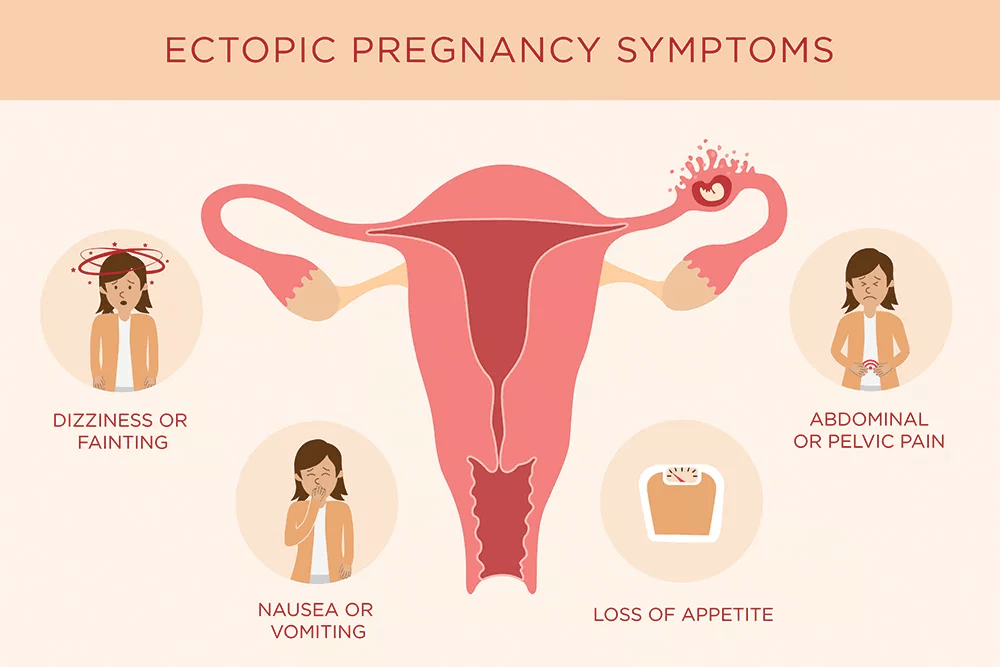
a) Symptoms:
1. A short period of amenorrhea
2. Severe lancinating pain in one iliac fossa or in the hypogastrium immediately followed by profound collapse
3. Slight, sanguineous or dark colored vaginal bleeding
4. Feeling of nausea, vomiting and dyspnoea
b) Sings:
1. General: There may be anemia, fever (2% of cases) and sings of shock
2. Per abdominal examination:
- Abdomen is tense and tender and tenderness more in lower abdomen
- Shifting dullness may be elicited
- Gut may be distended
3. Per vaginal examination: Usually not done due to fear of precipitating more bleeding and extreme tenderness.
- Vaginal mucosa blanched white
- Extreme tenderness on palpation of the fornix or movement of the cervix
- No mass usually felt through the cervix
c) P/A examination: On palpation:
1. Exhibits abdominal or pelvic tenderness during palpation.
2. Tenderness in patients with EP may be generalized (45%), located bilaterally in the lower quadrants (25%), or located unilaterally in a lower quadrant (30%)
3. Rebound tenderness may or may not be present.
4. A palpable adnexal mass or mass in the cul-de-sac is reported in approximately 40% of cases; absence of a palpable mass does not rule out EP
5. Additional signs include shoulder pain (15%) and low-grade fever (less than 10%).
d) P/V examination:
1. Should not be done due to tenderness.
e) Lab. Investigation:
Blood
1. TC, DC (Neutrophilic leukocytosis)
2. Hb% below normal
3. ESR raised
4. Blood grouping ar and Rh typing – should be done for management ẞ- HCG
USG:
1. TVS (Transvaginal sonograph is the choice)- can detect an EP greater than 2 cm.
2. USG can show:
3. Empty uterus
4. Cystic or solid adnexal masses,
5. Dilated and thick-walled fallopian tubes,
6. Free echogenic fluid in pelvis; hematosalpinx, and
7. Extra uterine gestational sac that contains a yolk sac, with or without an embryo.
Laparoscopy: it is confirmatory. If USG is not conclusive then laparoscopy is the choice as it is both diagnostic and therapeutic.
B. Management:
a) General:
1. Immediate hospitalization
2. Two large bore intravenous canuulas
3. Indwelling catheter placed to monitor urine output
4. Blood is sent for grouping and cross matching
5. IV fluid infusion (Hartman solution)
6. Blood transfusion if needed generally 4-8 bags blood should be kept ready
7. Analgesics
8. Antibiotics
9. Sent the patient to OT room as soon as possible
b) Specific:
1. Laparoscopy
2. Laparotomy under G/A (after resuscitation)
3. Anti D immunoglobulin in Rh (-ve) mother (within 72 hours)
Complication of Ectopic Pregnancy:
1. Maternal death due to hemorrhage of untreated or mistreated ruptured ectopic
2. Chronic salpinigitis
3. Sterilityinfertility – Who have undergone surgery
4. Intestinal obstruction
5. Fistula
Preparation of a Patient of Rupture Ectopic Pregnancy:
After immediate hospitalization the patient should be prepared in the following way- If the patient is haemodynamically unstable then:
1. Open I/V channel and IV infusion should start
2. Immediate analgesia a by Inj. Pethidine 10 mg/IM
3. Catheterization of the patient
4. Start appropriate antibiotic
5. Inform the party about the need of blood transfusion and tell them to manage 4 bag bloods.
Treatment of Unruptured Tubal Pregnancy:
In case of unruptured tubal pregnancy there are two options of treatment.
A. Waiting for spontaneous resolution: In this Case when pregnancy test is negative, symptoms are mild and subsiding gynaecologists prefer to wait for spontaneous resolution to take place.
B. Surgery: In this case doctors don’t want to take risk and they prefer to go for surgery and the choice is unilateral salpingectomy or sulpingo-oophorectomy
D/D of Ectopic Pregnancy:
1. Acute appendicitis
2. Renal colic
3. Torsion of an ovarian cyst
4. Torsion of a pedunculated leiomyoma
5. Acute or subacutesalpingitis
6. Abortion complicated by salphingitis
7. Retroverted gravid uterus
8. Rupture of an endometriotic cyst
9. Dysmenorrheat
10. A reaction of an intra-uterine contraceptive device
11. Intraperitoneal haemorrhage