Embryo and foetus – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Embryo and foetus
Definition of embryo:
An unborn or unhatched offspring in the process of development, in particular a human offspring during the period from approximately the second to the eighth week after fertilization (after which it is usually termed a fetus).
or
An organism in the early stages of growth and differentiation, from fertilization to the beginning of the third month of pregnancy (in humans). After that point in time, an embryo is called a fetus.
Definition of foetus
The developing young in the uterus, specifically the unborn offspring in the post embryonic period, which in humans is from the third month after fertilization until birth.
or
An unborn offspring, from the embryo stage (the end of the eighth week after conception, when the major structures have formed) until birth.
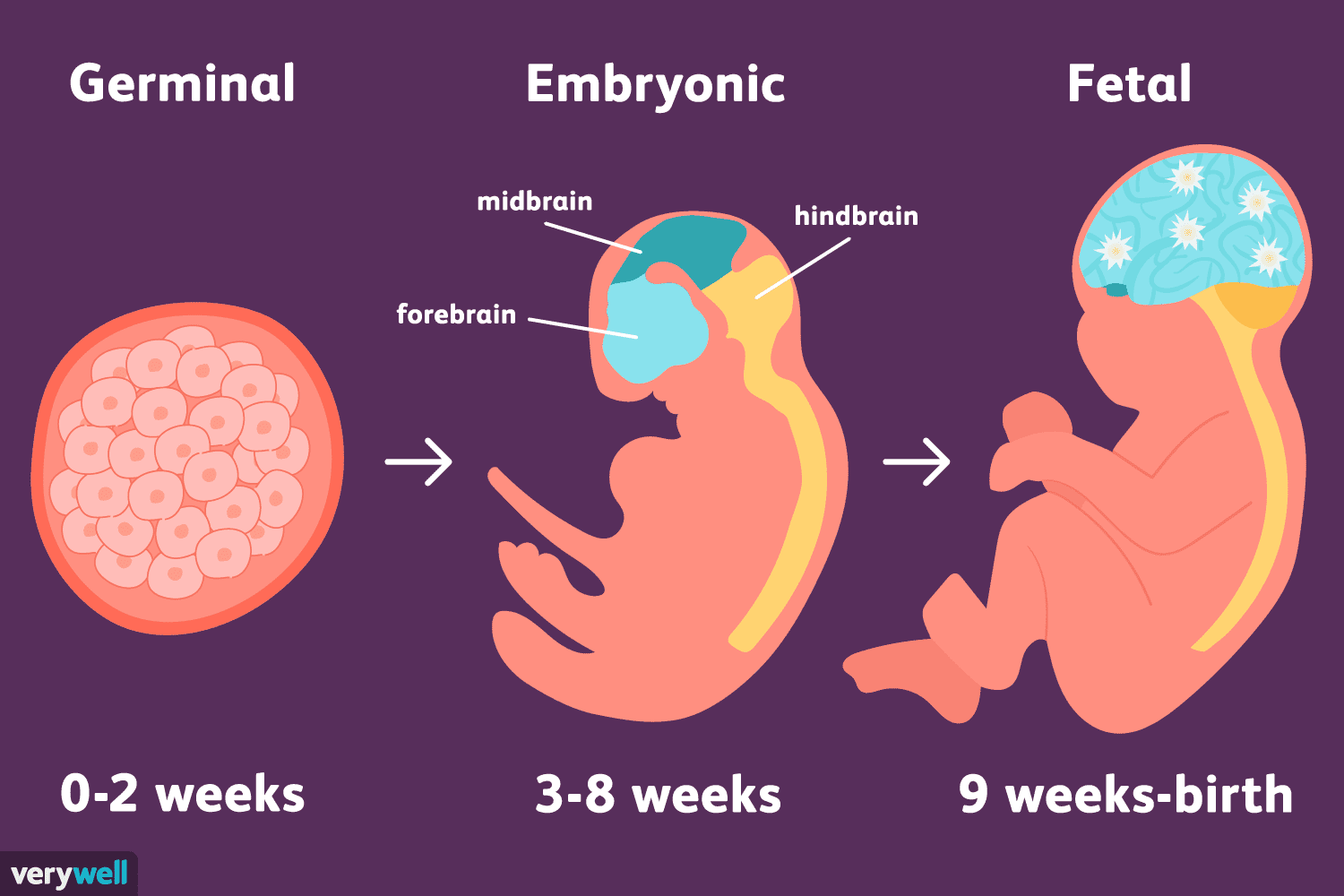
Figure: Embryo and foetal growth
Stages of fetal development:
Pre-embryonic stage:
1. from fertilisation to 2 weeks post- fertilisation (this is the same as 3 to 4 weeks pregnancy/gestational age)
2. As per previous lesson: at fertilisation a spermatozoon (sperm) penetrates the oocyte (ovum) and the two join together. The fertilised ovum is now called the zygote.
3. Over the next few days, the zygote goes through a period of rapid cellular division by mitosis; from 2 cells, to 4, then 8,16; after several days the zygote has 32 cells.
4. This cluster of cells is called the morula as it resembles a mulberry!
5. the morula develops a fluid filled cavity or blastocele, and the developing fertilised ovum is now known as a blastocyst;
6. The blastocyst has a fluid filled core, an outer layer of single cells called the trophoblast & an inner cell mass clumped at one end;
7. The trophoblast will form the placenta and chorion; the inner cell mass will become the embryonic dise and form the fetus, the umbilical cord, and amnion.
8. Implantation; by the day, tiny finger-like projections from the trophoblast become ‘sticky’ and it burrows into the endometrium; by day 10, it is completely embedded in uterine lining (see later section on development of placenta).
9. At fertilisation, each parent provides chromosomes, so when the baby is bom it will have 46 chromosomes, 23 pairs.
Embryonic stage:
1. From 3 to 8 weeks after fertilisation (this is the same as 5 to 10 weeks pregnancy/gestational age).
2. The developing conceptus is now called an embryo;
3. The cells still multiply, and differentiation occurs; that is, tissues begin to assume specific characteristics and functions, and thus rudimentary organs and organ systems are formed. Cells in the embryo seem to know where and when to change shape to assist in the embryonic development.
4. By the 3rd week, the embryo has 3 germ layers ectoderm (outer layer, which will form skin, hair, nails, nervous system)
a) mesoderm (middle layer, will form skeletal, muscular, circulatory systems)
b) Endoderm (inner layer, which will form glands, lungs, urinary, digestive systems.
5. By 8 weeks after fertilisation, all of the organ systems and major structures are present, and embryo has a human form.
[Ref-DMW, Lesson Plan volume 1/page 16-17]
Or (Another Answer)
Stages of fetal development:
There are 3 major stages of fetal development. These are –
A. Pre-embryonic period: It start with ovum fertilization to the end of the 3rd weeks of development.
B. Embryonic period: Week 4th through 7th week of gestation.
C. Fetal period: week 8th through birth.
A: Pre- embryonic stages/period:
1. Development of fertilized ovum/zygote:
Cell division takes place and the fertilized cell or zygote mitotic division into 24 →8→16 and it consist of a ball of cells like a mulberry known as the marula. 3 to 4 days are required for the journey along the tube to the uterus. The first cell division ends 30 hours after fertilization occur rapidly.
2. Embedding of the ovum/zygote:
Six to seven days may elapse before the fertilized ovum, the structure is now called a trophoblast/ blastocyst, which develops into fetal membrane and its form the embryo.
3. Getting attached (Blastocyst and endomotrium):
The blastocyst stays within the zona pellucida (Inner membrane of the ovum) unattached to the uterus. 1st week after fertilization the blastocyst attaché the endometrium and 2 contact with the endometrial lining proliferates the endometrium. The next week, the endometrial surface restores the attached blastocyst/ fertilized ovum.
4. Development of blastocyst / Fertilized ovum:
When the ovum burrows in to the implantation cavity or uterus, the endometrial cells heal the opening and embedding of the ovum is complete.
B. Embryonic stage
During the embryonic period (4 to 7 week)the developing zygote starts to take on a human shape and is now called an embryo.
There primitive layers in the ovum can be differentiated and from each each layer particular parts of the develop.
These layers are
1. Ectoderm
2. Mesoderm &
3. Endoderm
1. Ectoderm, the outermost layer and it develops into the –
➤ Epidermis
➤ Nervous system
➤ Pituitary gland
➤ Tooth enamel
➤ Salivary glands
➤ Optic Lens
➤ Hair
2. Mesoderm, The middle layer and it develop into
➤ Connective and supporting tissue
➤ Blood and vascular system.
➤ Musculostructure
➤ Teeth
➤ Pericardial, pleural and peritoneal cavities
➤ Kidney and ureters
3. Endoderm, the innermost layer and develops into
➤ Pharynx and trachea
➤ Auditory cannal
➤ Liver
➤ Pancreas
➤ Bladder and urethra
➤ Prostate
➤ Lung
C. From embryo to fetus stage
Significant growth and development take place within the first 3 months following conception.
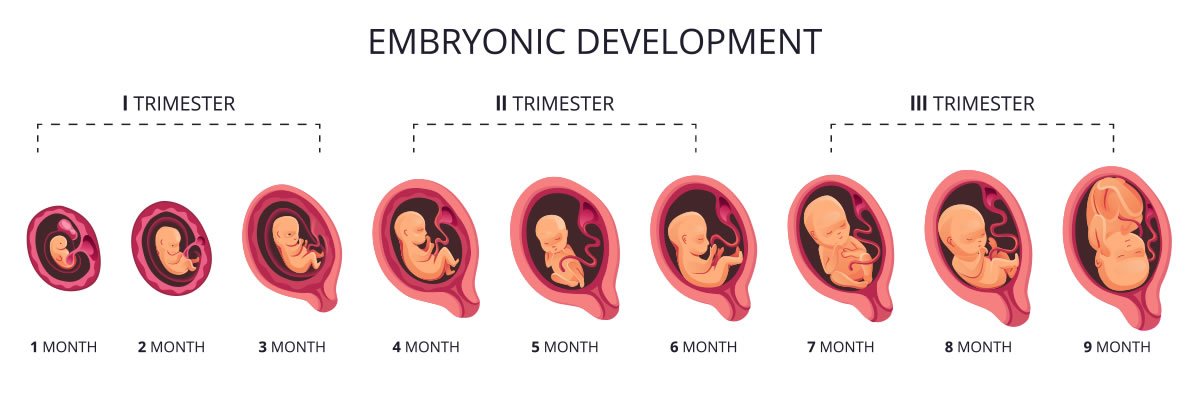
Figure: Fetal growth and development
Fetal presentation and position:
Foetal presentation:
In obstetrics, the presentation of a fetus about to be born refers to which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
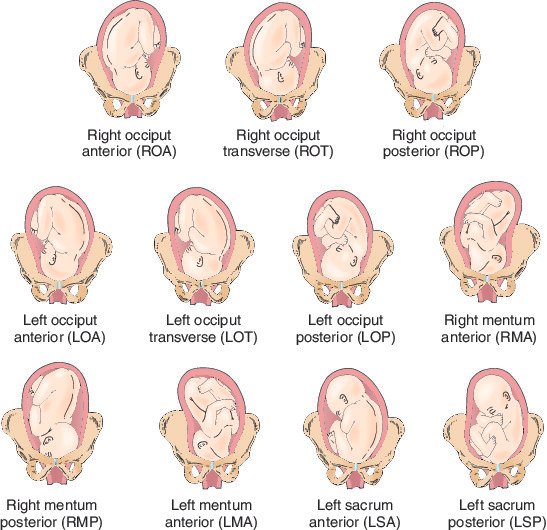
Figure: Foetal presentation
Foetal position:
The relationship of the part of the fetus that presents in the pelvis to the four quadrants of the mat ernal pelvis, identified byinitial L (left), R (right), A (anterior), and P (posterior). The presenting part is also identified by initial O (occiput), M(mentum), and S (sacrum). If a fetus presents with the occiput directed to the posterior aspect of the mother’s right side, the fetal position is right occ iput posterior (ROP).
Foetal presentation and position:
Foetal presentation:
In obstetrics, the presentation of a fetus about to be born refers to which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation. A malpresentation is any presentation other than a vertex presentation (with the top of the head first). Thus the various presentations are:
A. cephalic presentation (head first):
➤ vertex (crown) – the most common and associated with the fewest complications
➤ sinciput (forehead)
➤ brow (eyebrows)
➤ face
➤ chin
B. breech presentation (buttocks or feet first):
➤ complete breech
➤ footling breech
➤ frank breech
C. shoulder presentation:
➤ arm
➤ shoulder
➤ trunk
Foetal Position:
Definition: Relationship of presenting part to maternal pelvis: and based on presentation: Note fetus enters pelvis in occipito-transverse plane (left or right), descent and flexion then rotates 90 degrees to occipito-anterior (most commonly)
Common position in Cephalic presentation:
A. Vertex presentation with longitudinal lie:
➤ Left occipitoanterior (LOA) the occiput is close to the vagina (hence known as vertex presentation) faces anteriorly (forward with mother standing) and towards left. This is the most common position and lie.
➤ Right occipitoanterior (ROA) the occiput faces anteriorly and towards right. Less common than LOA, but not associated with labor complications.
➤ Left occipitoposterior (LOP)-the occiput faces posteriorly (behind) and towards left.
➤ Right occipitoposterior (ROP)-the occiput faces posteriorly and towards right.
➤ Occipitoanterior the occiput faces anteriorly (absolutely straight without any turning to any of the sides)
➤ Occipitoposterior the occiput faces posteriorly (absolutely straight without any turning to any of the sides)
➤ Face presentation
B. Breech presentation with longitudinal lie:
➤ Left sacrum anterior (LSA)-the buttocks, as against the occiput of the vertex presentation, like close to the vagina (hence known as breech presentation), which like anteriorly and towards the left.
➤ Right sacrum anterior (RSA) the buttocks face anteriorly and towards the right. Left sacrum posterior (LSP)-the buttocks face posteriorly and towards the left.
➤ Right sacrum posterior (RSP) the buttocks face posteriorly and towards right.
➤ Sacrum anterior(SA)-the buttocks face anteriorly.
➤ Sacrum posterior (SP)-the buttocks face posteriorly!
C. Shoulder presentation with transverse lie are classified into four types, based on the location of the scapula (shoulder blade); note: this presentation needs to be delivered by cesarean section.
➤ Left scapula-anterior (LSA)
➤ Right scapula-anterior (RSA)
➤ Left scapula-posterior (LSP)
➤ Right scapula-posterior (RSP)