Fat Embolism syndrome – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Fat Embolism syndrome
Introduction:
Fat embolism syndrome is a major cause of morbidity and mortality in trauma patients. It has been said that fat embolism is fatal in 10-15% of the cause. It is occurring within 72 hours of skeletal trauma. It usually manifests within 24-48 hours. But sometimes may be delayed. It synonym with acute respiratory distress syndrome. Vong Bergman first diagnosed fat embolism syndrome in 1873. He explain it as, when a major bone fracture occur, some fat particles are released from the bone marrow then they run over the blood as the name of emboli. Lastly it reaches pulmonary circulation and causes ARDS.
Fat embolism syndrome:
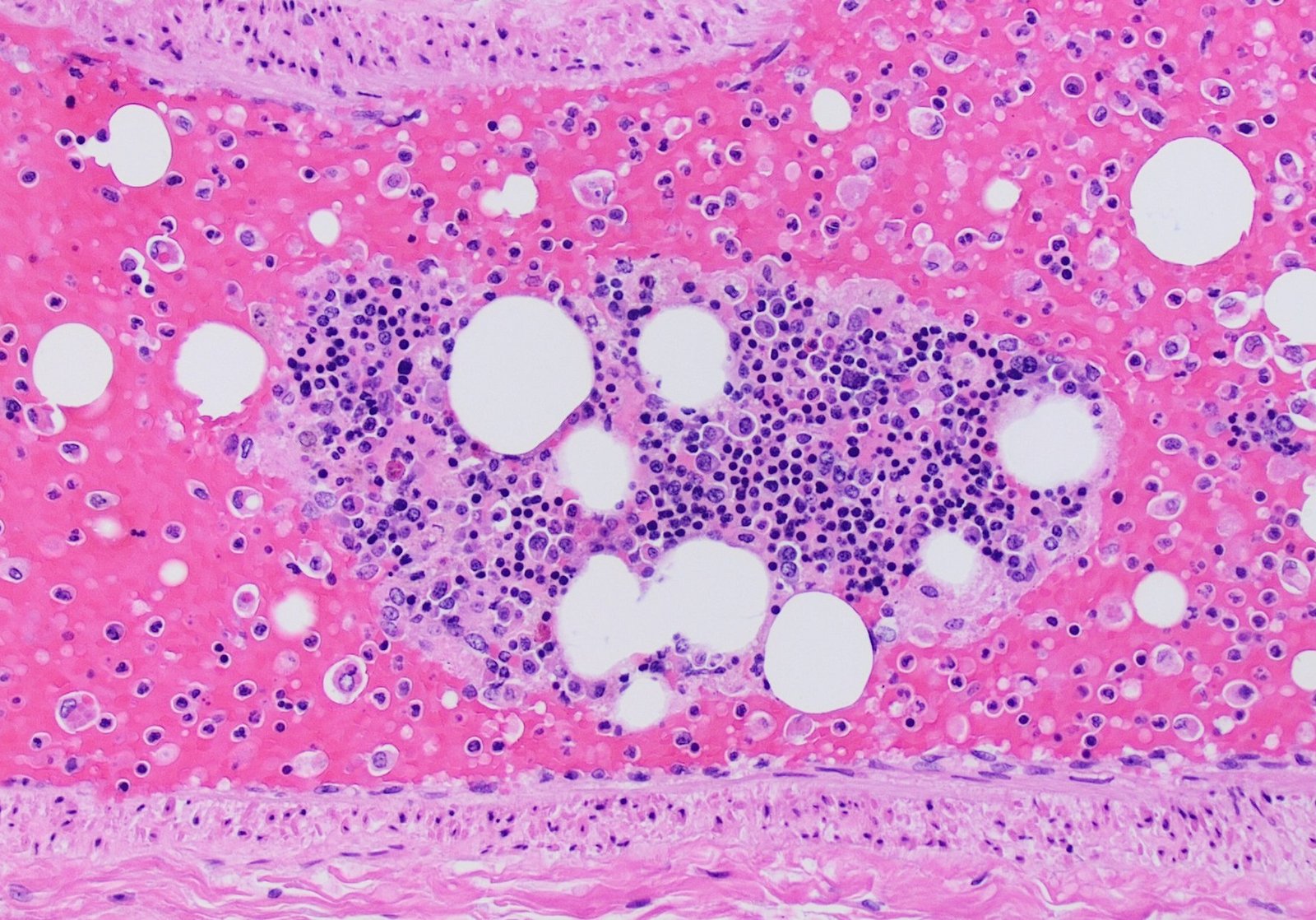
Fat embolism occurs when fat is released into blood from bone marrow, becomes entrapped in the lung capillaries and occluded the small vessels that supply brain, kidney and other organs.
Or
Fat embolism is a clinical condition in which fat released following bone injury giving rise to various clinical manifestation
Or
Fat embolism is a post traumatic distress syndrome occurring within 72 hours of skeletal trauma.

Etiology of fat embolism syndrome:
1. Young adult ( 20-30 years of age)
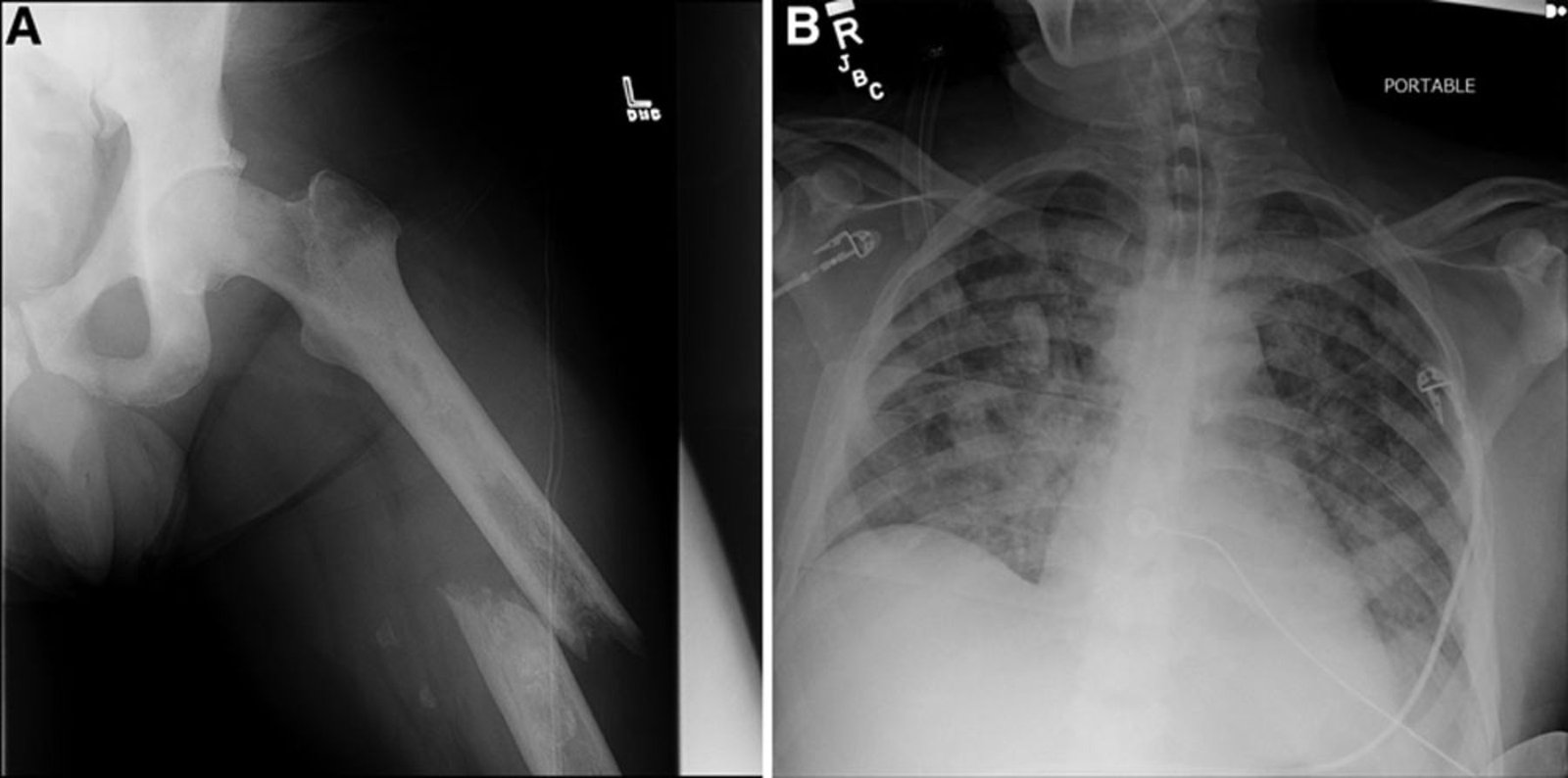
2. Pelvic fracture.
3. Fat released from the bone marrow:
a) Mechanical theory: During mechanical injury fat globule released from bone marrow.
b) Biochemical theory:-
- Obstructive theory: From plasma by agglutination of chylomicrons which acts as an
embolus. - Toxic theory: Free fatty acid destroys the pneumocytes and causes ARDS.
Types of Fat Embolism Syndrom: Types of fat embolism: According to Servitts fat embolism has three types:
1) Classical type: In this variety of onset is less than 24 hours. Common presenting features are tachycardia, tachypnea, pyrexia and petechial rashes.
2) Fulminating type: Here sequence of events are very fast and there is no time for rashes to develop. Patients is comatose within hours and throws repeated seizares. Patients rapidly collapse and death supervenes.
3) Incomplete type: Manifestation is between the two types. Unexplained tachycardia, fever, and rash are its features.
Sign and syndrome of fat embolism:
1. H/O open fracture.
2. Increase in respiratory rate/Tachypnea >25 beat/ minute.
3. Tachycardia > 100 beat/minute.
4. Temperature > 37.8° C.
5. Dyspnea, pallor, exhaustion and collapse.
6. Abnormal behavior:
- Agitation.
- Confusion,
- Muscle weakness to delirium (disordered mental state with excitement & delusion) to coma due to
- hypoxia
- Drowsiness,
7. Petechial rach: Commonly finding in
- Axilla
- Chest
- Neck
- Conjunctiva.
8. Change level of consciousness.
Characteristics of petechial rash in ARDS:
1. Presents acres the nicely in
- Axilla
- Chest
- Neck
- Conjunctiva
2. Fades rapidly
3. Occurs periodically with anak of co
4. Ratiomal rashes ans pulpmics
Importance of petechial rash:
Conjunctiva of lower lid/ retina rashes is sure sign of fat embolism syndrome.
Investigation of fat embolism syndrome:
1. X-ray of the chest:
a)lt may snow storm appearance( pathognomic)
b) Increased pulmonary marking.
c) Dialatation of Rt side of heart.
2. PaO2: 60 mm of Hg.
3. Serum lipase level: Increased.
4. Platelet count: 1.5 lach. (Thrombocytopenia)
5. ECG: Prominent s-wave
6. Gurd test: Isolation of fat emboli from the blood.
7. Hb: (Anemia)
8. CT Scan, MRI of the brain helps to grate the severty of fat embolism.
9. Fat in the sputum, urine.
Diagnostic criteria of fat embolism syndrome:
Gurd describe the fat embolism syndrome on the basis of ranking in major criteria and minor criteria That is given below:
A. Major criteria:
1. Axillary and subconjuntival petechial.
2. PaO2 <60 mm of Hg
3. CNS depression.
B. Minor criteria:
1. Pulse 110 b/min.
2. Pyrexia 38.5 с
3. Retinal embolism
4. Raised ESR
5.-Platelet count.
6. Fat globules in sputum
7. Fat in urine.
C. Diagnostic criteria:
1. At least 1 from major criteria and 4 from minor criteria are required to make diagnosis of f embolism syndrome.
Medical management of fat embolism syndrome:
There are two important steps of management of FES/ARDS.
A. Non specific management.
B. Specific management.
A. Non specific management:
It consists of 3 important steps:
1. Keep:
- Airway patient.
- Fracture immobilized by plaster of paris.
2. Restore:
- Blood volume
- Fluid volume
- Electrolyte balance.
3. Avold:
- Unnecessary transportation
- Careless handling of injured
B. Specific management:
1. Respiratory support:
- 02 inhalation,
- Ventilator support.
2. Drugs:
a. Hydrocortisone- 6 hourly for 3 days.
b. Heparin
c.Antiplatelet.
d. Dexfran
e. Intravenous alcohol( not used today)
f. Antibiotics.

Complication of fat embolism syndrome:
1. Minute and micro- haemorrhage in the lung capillaries.
2. Corpulmonale.
3. Interstinal hemorrhage.
4. Edema.
5. Heart failour.
6. Chemical pneumonitis
7. Hypovolumic shock
Effects of arterial embolism:
1. Brain: Blockage at middle cerebral artery causes hemiplegia, ttreatment ischaemic attacks (TIA), visual disturbances.
2. Blockage at central retinal artery causes amaurosis fugas, or permanent blindness.
3. Blockage at mesenterie vessels causes intestinal gangrene.
4. Blockage at renal artery leads to haematuria, loin pain.
5. Blockage at limb vessels causes pain, pallor, pulseless, paresis, ulceration. gangrene
Note: Commonest site of arterial emboli is common femoral artery.
[Ref-Sriram Bhat M “SRB’s Surgery for Nurses” 1″ page-135]
Nursing management of fat embolism syndrome:
1. Airway care:
- Assess the sign and symptoms of airway obstruction.
- Clear the airway.
- Correct positioning
- Attach ventilator to monitor 02 saturation.
- Check the colour of the pts to detect pallor, cyanosis.
- Monitor respiratory rate
- Auscultate the lung sounds.
- Monitor ventilator functioning.
2. Promotre circulatory volume:
- Constant monitoring of BP, pulse.
- Administer intravenous fluid.
- Monitor any fluid overload.
3. Immobilized fracture site:
- Splinting and stabilizing long bone fractures as soon as possible.
4. Reduce body temperature:
- Assess body temperature
- Note down in the chart
- Cold sponging
- Antipyretic
- Good environment of the room.
5. Prevent risk of infection:
- A fracture site is good concern.
- Regular dressing if internal fixation.
- Maintain hygiene.
- Regular changes bed linen, wet cloths.
- Administer antibiotic according to doctors order.
6. Prevent bed sore:
- Change position 2 hourly
- Back massage on bony prominence.
- Apply powder on the bone prominence.
7. Frequent monitoring:
- Pulse
- Blood pressure
- Skin colour
- Mental state
- Urine
- PaO2
- Respiratory effort.
Read more: