Gastro-intestinal bleeding – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Gastro-intestinal bleeding
Gastro-Intestinal Bleeding:
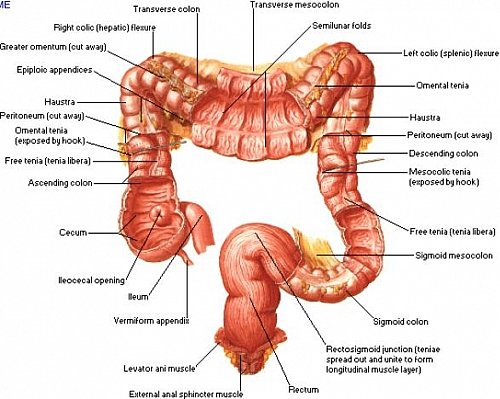
Gastrointestinal bleeding (GI bleed), also known as gastrointestinal hemorrhage, is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool.
Important Definition
Presentation of upper GI bleeding:
- 20% present with melaena
- 30% haematemesis
- 50% both haematemesis & melaena
Haematemesis:
- Vomiting out of blood (Above ligamentum teris) from stomach through oesophagus & mouth
- Indicates an upper GI source of bleeding
Melaena
- Passage of loose /semisolid foul-smelling dark, black tarry stool per rectum.
- Melaena indicates that blood has been present in the GI tract for at least 14 h.
- Melaena is suggestive upper Gl bleeding, small gut bleeding or right sided colonic bleeding.
Difference between Hematemesis and Hemoptysis:
| Points | Haematemesis | Haemoptysis |
| Definition | Vomiting of blood or blood clot. | Coughing out of blood |
| Colour of blood | Altered | fresh |
| Taste | Acidic | Alkaline |
| Contents | Mixed with food materials | Mixed with cough |
| Other symptoms | Symptom of Gl system | Symptom of respiratory systems |
| Reaction with litmus paper | Turn to red | Turn to blue |
Nice to know:
Basic elements of management of acute upper gastrointestinal bleeding include-
- Prompt patient resuscitation and stabilization.
- Assessment of the onset and severity of bleeding.
- Regional localization of bleeding site.
- Determination of the most likely cause of upper gastrointestinal bleeding.
- Preparation for emergent upper GI endoscopy.
- Control of active bleeding or treatment of lesions at high risk of rebleeding with therapeutic endoscopy.
- Minimization of treatment related complications.
- Treatment of re-bleeding episodes.
Common Causes of Upper Gastro-Intestinal Bleeding:
- Bleeding Peptic ulcer diseases (35-50%)
- Gastric erosions (10-20%)
- Oesophagitis (10%)
- Rupture of varices 2-9% (Oesophageal & gastric) (Liver diseases & Portal vein thrombosis).
- Mallory Weiss tear (5%)
- Vascular malformation. (5%
- Cancer of stomach or oesophagus (2%)
- Dieulafoy’s lesion-2%
- Aorto-duodenal fistula (0.2%)
The way of presentation of upper gastro-intestinal bleeding:
- Haematemesis and/or melaena (Mainly)
Causes of Haematemesis:
- Mallory Weiss tear
- Irritation or erosion of the lining of the esophagus or stomach
- vomiting of ingested blood after hemorrhage in the oral cavity, nose or throat
- Vascular malfunctions of the gastrointestinal tract such as bleeding gastric varices or intestinalvarices.
- Tumor of the stomach or esophagus.
- Radiation poisoning
- viral hemorrhagic fevers,
- Gastroenteritis
- Gastritis
- Peptic ulcer
- Chronic viral hepatitis
- Intestinal Schistosomiasis
- History of smoking
- latrogenic Injury (invasive procedure such as endoscopy or transesophageal echocardiography)
- Zollinger-Ellison Syndrome (severe peptic ulcer)
- Atrio-oesophageal fistula
Causes of Melaena:
a. Common:
- Diverticular disease
- Angiodysplasia
- Anal fissure
- Haemorrhoids
- Inflammatory bowel disease
b. Less common:
- Ischemic colitis
- Carcinoma
- Hook worm
- conditions of haematemesis
- Ulcerative colitis
- Crohns disease etc.
Management of Haematemesis:
Clinical features:
a. Symptoms:
- If bleeding is less: no systemic sign
- If bleeding is severe:
✔Weakness, faintness
✔Nausea, sweating
✔ Agitated, restless
✔ Disorientation
✔ Vomiting of coffee ground material or bright red blood
b. Signs:
- Patient is anxious and pale.
- Anemia in severe case
- Pulse: weak and rate is high
- BP: High
Investigations of haematemesis:
- Endoscopy of upper GIT
- Ba-meal X-ray
- Radionuclide scan with radio labeled red cells
- BT, CT and PT
- Full blood count
Treatment of haematemesis:
A. In case of bleeding from stomach and duodenum:
a. Conservative treatment:
- Bed rest
- Sedation (inj. morphine 15 mg IM or IV state)NG suction
- Liquid antacid 10-15 ml every hourly
- H₂ receptor blocker (IV cemetidine, ranitidine)
- IV infusion or blood transfusion
- Diet: Ice cold milk
b. Surgical treatment:
- Indications:
✔ Massive and continuous bleeding
✔ Recurrence of bleeding one has stopped
✔ Age over 60 years
✔ Previous H/O two/three times bleeding
✔ Continued bleeding
- Methods:
In chronic DU bleeding: Suturing of bleeding vessels with vagotomy and gastrojejunostomy/pyloroplasty.
✔ In gastric ulcer bleeding: Partial gastrectomy
✔ In acute gastric erosion: Gastrotomy with occlusion of bleeding vessels with ligation/diathermy, or partial gastrectomy
B. In case of bleeding from oesophageal varices:
a. Conservative treatment:
- Bed rest
- Sedation (cautiously)
- Nasogastric suction
- Enema
- Neomycin
- Vitamin K (15 mg IV)
- Vasoconstrictor drugs
- Mechanical compression with sengstaken tube
b. Surgical treatment:
- Ligation of varices
- Oesophageal transcetion and anastomosis
- Bypass operation to correct portal hypertension
Clinical Features:
a. Symptoms:
- Weakness
- Blurring vision
- Coldness of the body
- Fainting and syncope
- Black tarry stool or frank
- Blood may pass per rectum
b. Sing:
- Patient is anxious and pale
- Signs of dehydration
- Pulse rate: increase
- Low BP
Investigation: (same as haernatenesis)
Treatment: (same as haematemesis)
