Hemolytic disease of the newborn – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Hemolytic disease of the newborn
The term HDN (hemolytic disease of the newborn) is describe bleeding in early neonatal period (under one week) which occurs due to fall in vitamin K (VK) dependent coagulation factors.
[Ref-Suraj Gupta/11/542]
Or,
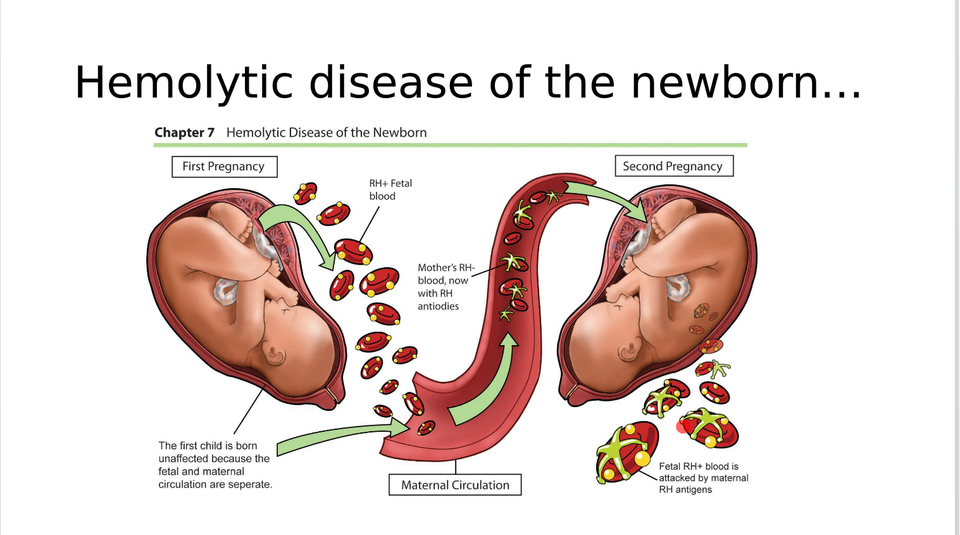
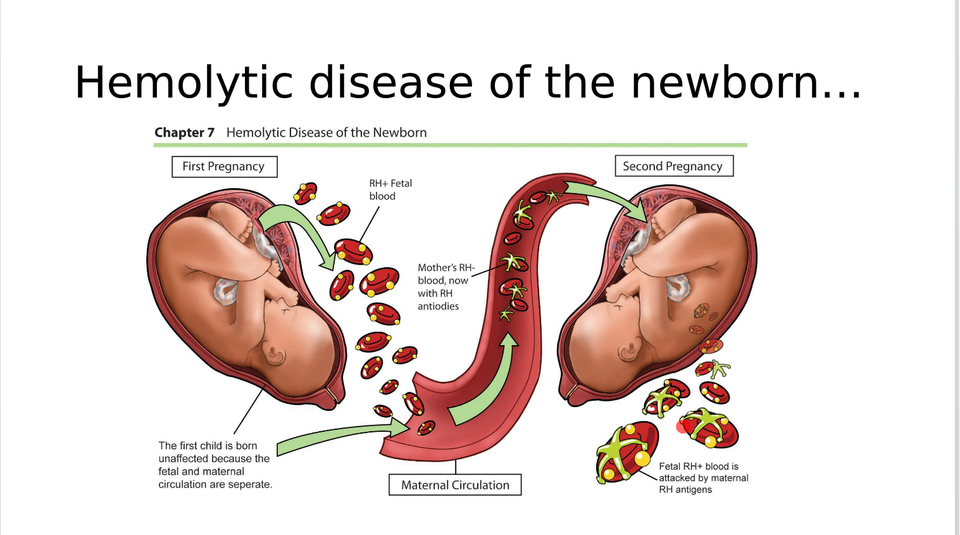
The term HDN (hemolytic disease of the newborn) is a severe form of anaemia caused in a fetus or newborn infant by incompatibility with the mother’s blood type, typically when the mother is rhesus negative and produces antibodies which attack rhesus positive fetal blood through the placenta.
Causes of Haemolytic Disease of Foetus And Newborn:
1. Rh-incompatibility:
Rh-isoimmunization is also called as erythroblastosis fetalis, a major cause of severe hyperbilirubinemia. It occurs in Rh-negative mother, who is carrying an Rh-positive fetus. The antigen of fetal RBCs may invoke antibody response in the maternal immunologic system.
2. ABO-incompatibility:
It occurs commonly in ‘O’ group mother and “A” or ‘B’ group fetus. It is milder than Rh- hemolytic disease and may occur even in first born baby. The history of increasing severity of disease in subsequent pregnancies is generally not present.
3. Minor groups-incompatibility:
Isoimmunization can occur for minor groups like the Kell, Duffy M and N, etc.
Symptoms of HDN in a newborn
Symptoms can occur a bit differently in each pregnancy and child.
During pregnancy, you won’t notice any symptoms. But your healthcare provider may see the following during a prenatal test:
♦ A yellow coloring of amniotic fluid. This color may be because of bilirubin. This is a substance that forms as blood cells break down.
♦ The baby may have a big liver, spleen, or heart. There may also be extra fluid in his or her stomach, lungs, or scalp. These are signs of hydrops fetalis. This condition causes severe swelling (edema).
After birth, symptoms of the baby may include:
♦ Pale-looking skin. This is from having too few red blood cells (anemia).
♦ Yellow coloring of baby’s umbilical cord, skin, and the whites of his or her eyes (jaundice). Baby may not look yellow right after birth. But jaundice can come on quickly. It often starts within 24 to 36 hours.
♦ Newborn may have a big liver and spleen.
♦ A newborn with hydrops fetalis may have severe swelling of their entire body. They may also be very pale and have trouble breathing.
Clinical features of hemolytic disease of the newborn:
1. Gastrointestinal bleeding-hematemesis and/or melena.
2. Bleeding from injection or puncture sites.
3. Umbilical bleeding commonly occurs.
[Ref-Suraj Gupta/11/543]
Determine Hemolytic disease of the new born:
In a child with bleeding manifestations, initial diagnostic work-up includes a check on the platelet count and PT and PTT estimation.
1. In VKDB, PT (Prothrombin time) and PTT are prolonged.
2. Platelet count is normal.
3. The activity of VK dependents factors (II, VII, IX, X) is decreased.
4. Levels of fibrinogen are normal.
Treatments of VKDB in newborn:
1. As in all deficiency states, replacement is the treatment required.
2. Replacement VK therapy needs to be rapidly effective as L-VKDB is often associated with potentially life threatening intracranial bleeding.
3. In a child suspected to have the disease intravenous or subcutaneous administration is recommended.
4. Intramuscular (i/m.) administration is avoided to prevent hematoma formation.
5 . The effect of VK administration is rapid but some severe cases may require plasma, fresh frozen plasma or prothrombin complex transfusion.
6. Whole blood transfusion may be required in cases with significant blood loss.
7. Meticulous supportive care is needed particularly in cases with intracranial bleeding.
[Ref-Suraj Gupta/11/544]
Preventive measures of hemolytic disease of the newborn:
1. VK is administered i.m. though oral administration has also been found to be effective as far as prevention of VKDB in the first week is concerned.
2. Oral administration does not consistently eliminate L-VKDB.
3. ITP must be differentiated from purpura secondary to aplastic anemia, leukemia, and other infiltrative processes of the bone marrow.
4. In infants, it needs to be distinguished from genetically determined thrombocytopenias.
5. In order children, SLE, lymphomas and AIDS (when they manifest with thrombocytopenic purpura is accompanied by significant splenomegaly, congestive splenomegaly secondary to primary liver disease, lipidosis, and reticuloendotheliosis must be excluded.
Poor prognostic indicators are:
1. Prothrombin time (PT) 1.5 times.
2. Activated partial thromboplastin time (APTT) > 2.5 times
[Ref-Suraj Gupta/11/544]