Today our topic of discussion is ” Hemostasis Blood vessel “. The cardiovascular system is a marvel of engineering, a network that ensures continuous circulation of blood throughout the body. An integral part of this system is the blood vessel network, which can face potential damage, both external and internal. When these damages occur, a critical process known as hemostasis springs into action to prevent excessive bleeding. This article sheds light on the intricate relationship between blood vessels and hemostasis in the cardiovascular system.

Hemostasis Blood vessel – The Cardiovascular System: Blood
1. Hemostasis: A Brief Overview
Hemostasis is a multi-step process designed to stop bleeding and ensure blood remains within the circulatory system following vessel injury. It involves the coordinated action of the vascular system, platelets, and various proteins found in plasma to form a stable clot.
2. Blood Vessels: The Transport Channels
Blood vessels form the transportation channels for blood, nutrients, oxygen, and waste. They vary in size and function, ranging from large arteries and veins to minute arterioles, venules, and capillaries.
3. The Interplay of Hemostasis and Blood Vessels
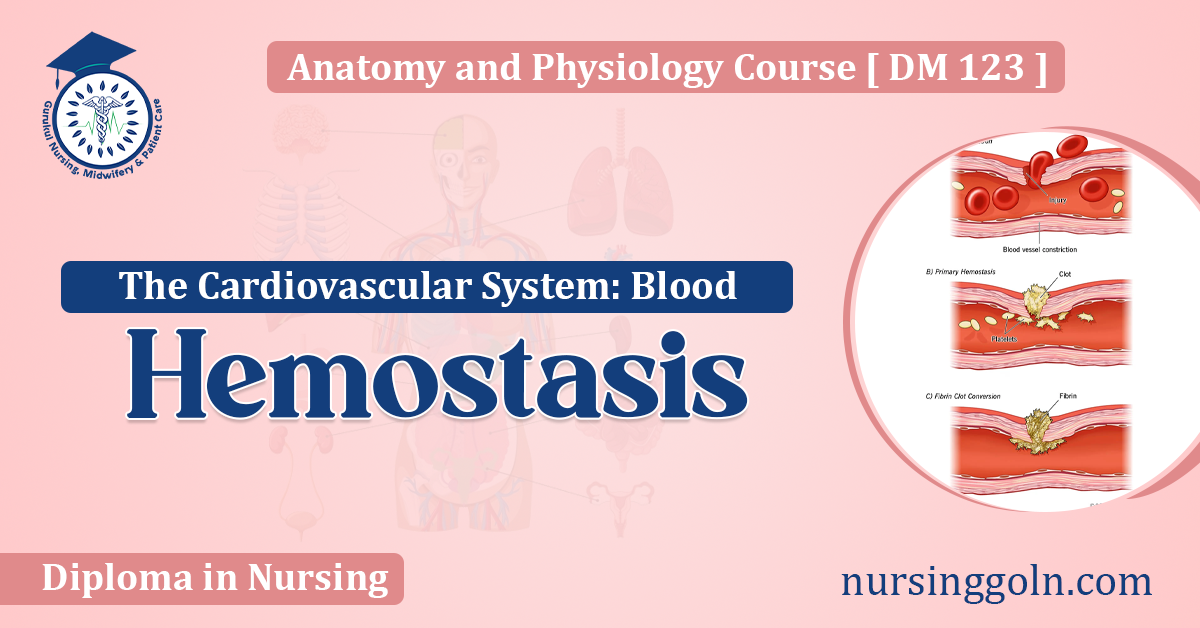
When a blood vessel is injured, the hemostatic response involves several stages:
a. Vascular Spasm (Vasoconstriction): The immediate response to blood vessel injury is a brief and spontaneous constriction of the vessel, which helps reduce blood flow and loss.
b. Platelet Plug Formation: Platelets adhere to the exposed collagen of the damaged vessel. They become activated, releasing chemicals that attract more platelets to the site. This aggregation forms a temporary “platelet plug.”
c. Coagulation: In this phase, a series of complex biochemical events occur, leading to the conversion of the plasma protein fibrinogen into fibrin threads that weave through the platelet plug, solidifying and stabilizing the clot.
d. Clot Retraction and Repair: Over time, the clot contracts to reduce its size (clot retraction). Simultaneously, tissue repair mechanisms, such as the proliferation of fibroblasts and smooth muscle cells, begin the repair process.
e. Fibrinolysis: Once the vessel is sufficiently healed, the clot needs to be removed. Plasminogen, which was incorporated into the clot, is activated to plasmin, which digests fibrin and dissolves the clot.
4. Disorders of Hemostasis and Blood Vessels
a. Thrombosis: Sometimes, blood clots form in vessels without an apparent injury, leading to blockages. If these occur in coronary arteries, it could lead to a heart attack.
b. Hemophilia: This genetic disorder affects the body’s ability to control blood clotting. Hemophiliacs lack or have low levels of specific clotting factors, leading to prolonged bleeding.
c. Atherosclerosis: Chronic injury to the vessel walls, combined with lipid deposits, can lead to plaque formation. These plaques can rupture, triggering clot formation and potential vessel blockage.
d. Vasculitis: An inflammation of blood vessels can weaken and damage walls, potentially leading to aneurysms or impaired blood flow.

5. Blood Vessels, Hemostasis, and Modern Medicine
a. Anticoagulants: Drugs like heparin and warfarin inhibit clot formation and are used to treat or prevent thrombosis.
b. Antiplatelet Drugs: Medications like aspirin interfere with platelet function, reducing the risk of thrombus formation.
c. Vascular Surgeries: Modern medicine can repair or replace damaged blood vessels, often using grafts or stents.
d. Hemostatic Agents: In surgeries, agents like gelatin sponges or fibrin glues can be applied to a bleeding site to promote hemostasis.
6. Current Research and Future Perspectives
With advancing technology, our understanding of hemostasis and its relationship with blood vessels is deepening. Techniques like bioengineering aim to create artificial vessels, while nanotechnology might offer solutions to targeted drug delivery for clot dissolution.

Conclusion
The intricate dance between blood vessels and hemostasis is fundamental to human survival. The self-sealing property of the vascular system, orchestrated by platelets, clotting factors, and the vessels themselves, ensures that we don’t bleed excessively from minor injuries. However, when this balance is disturbed, it can lead to life-threatening conditions. By understanding the delicate balance between hemostasis and the integrity of blood vessels, we are better equipped to address cardiovascular disorders, benefiting from the combined might of biology and modern medicine.