Hydatidiform Mole – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Hydatidiform Mole
Hydatidiform mole:
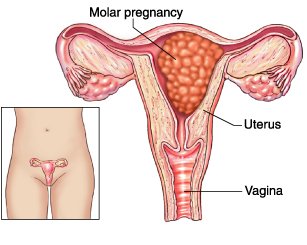
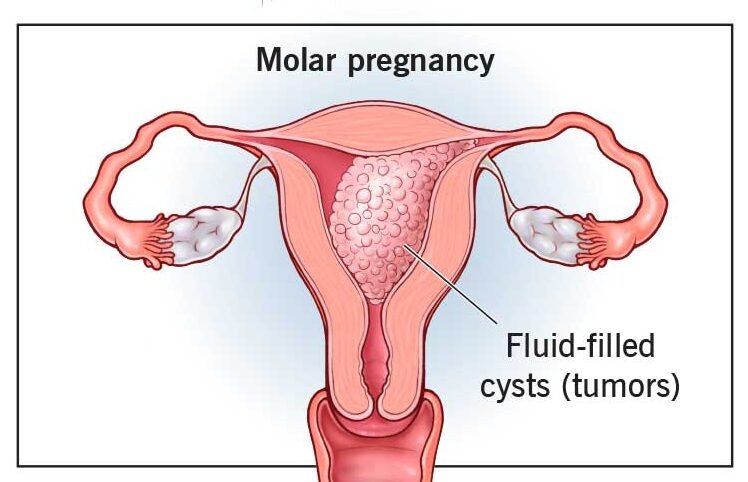
Hydatidiform mole is a rare mass or growth that forms inside the womb (uterus) at the beginning of a pregnancy. It is a type gestational trophoblastic disease (GTD). A cancerous form of GTD is called choriocarcinoma.
Or
It is an abnormal condition where there is hydropic degeneration of core (connective tissue stroma) with neoplastic proliferation of trophoblastic layer of chorionic villi.
Or
A hydatidiform mole is a growing mass of tissue inside the womb (uterus) that will not develop into a baby. It is the result of abnormal conception. It may cause bleeding in early pregnancy and is usually picked up in an early pregnancy ultrasound scan.
Classification of Hydatidiform mole:
1. Complete mole/classical mole:
The complete hydatidiform mole is characterized by lack of identifiable embryonic or fetal
tissues, gross vesicular swelling involving all the placental villi, and diffuse cytotrophoblastic
and syncytiotrophoblastic hyperplasia. Cellular anaplasia may also be present.
Complete hydatidiform moles usually have a 46,XX karyotype entirely of paternal origin. Complete mole appears to arise from an empty or inactivated ovum that has been fertilized by a single sperm carrying 23 chromosomes.
2. Incomplete mole/partial mole:
Partial hydatidiform mole is invariably associated with an embryo or fetus, cord, or membranes. Although the embryo usually dies by 9 weeks’ gestation, it may survive to the second and rarely even to the third trimester.
The characteristic pathologic features are chorionic villi of varying size with focal hydatidiform swelling and cavitations; marked villous scalloping; focal trophoblastic hyperplasia, usually limited to the syncytial trophoblastic cells; development of functioning capillaries manifested by the presence of erythrocytes; and prominent stromal trophoblastic inclusions.
Partial hydatidiform moles usually have a triploid karyotype (69 chromosomes), containing two sets of paternal and one set of maternal chromosomes. Partial moles may be confused with triploid embryos with a diploid set of maternal DNA and haploid set of paternal DNA.5 Until these cytologic differences became recognized, incidence rates were probably falsely elevated, because inclusion of triploid abortus cases resembling partialhydatidiform moles was likely.
Features of Complete And Partial Hydatidiform Moles:
| Feature | Complete Mole | Partial Mole |
| Synonyms | Classic, true | Incomplete |
| Fetal or embryonic tissue or membranes | Absent | Usually present |
| Villous capillaries | Usually absent; when present no fetal blood cells | Usually present; may contain fetal blood cells |
| Hydatidiform swelling of chorionic villi | Diffuse | Focal |
| Trophoblastic hyperplasia | Usually present | Mild and focal |
| Malignant potential | 15%-25% | 5%-10% |
| Karyotype | 46,XX;46,XY | 69,XXX;69,XXY |
[Ref-Dewhurt’s 7th/118]
Causes of Hydatidiform Mole:
Several risk factors for hydatidiform mole may be contributing causes but increase the chances of getting molar pregnancy very little. These include:
- diets low in protein, fat and vitamin A
- age – most often affecting women of childbearing age
- an earlier molar pregnancy
- prior miscarriages
- A or AB blood types, compared to B or O blood types.
Macroscopic feature:
A mass of grape like structures (each attached by a fine stalk) of varying sizes filling the uterus.
Microscopic feature:
1. Marked proliferation of syncytial or cytotrophoblastic epithelium.
2. Marked thinning of the stromal tissue due to accumulation of fluid.
3. Absence of blood vessel.
4. The villus pattern is distinctly maintained.
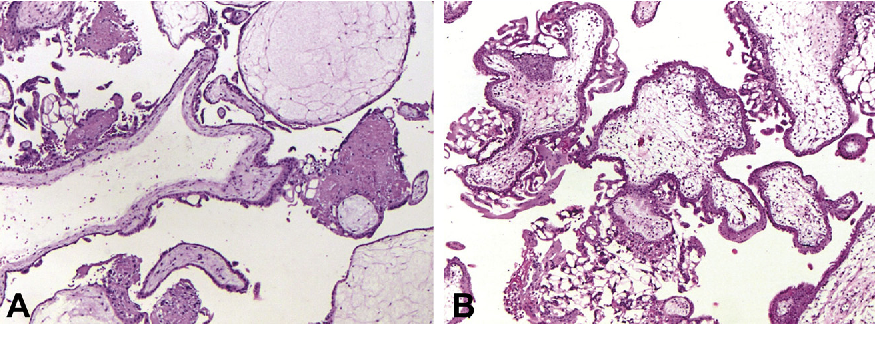
[Note: Hydropic degeneration Fig: Partial hydatidiform mole. Labyrinthine vascular pattern. with formation of central cisterns and prominent circumferential (Courtesy Dr. Ilana Ariel, Hadassah Medical Center, Jerusalem.) trophoblastic hyperplasia. (Courtesy Dr. Ilana Ariel, Hadassah Medical Center, Jerusalem.)]
Diagnosis:
1. C/F:
Symptoms:
- Short period of amenorrhoea.
- Exaggerated symptoms of early pregnancy. eg. excessive vomiting.
- Irregular vaginal bleeding which may be heavy.
- H/O per vaginal – grape like vesicle expulsion (50%).
- Wt. loss, fatigue, malaise.
- Pre-eclampsia (20%)
Signs:
1. General examination: III looking, weight loss, anaemia, features of toxaemia, oedema, HTN, proteinuria.
2. P/A examination:
- Size of uterus may be larger than the gestational age. (in some cases smaller)
- Uterus is doughy in consistency & does not contract.
- No fetal movement.
- Absence of fetal parts & fetal heart sound.
- Pelvic mass due to thicker luteal cyst.
3. P/Vexamination:
- Bilateral cystic enlargement of the ovaries through the fornices.
- If cervical os is open, molar tissue may be found.
B. Investigation:
- USG reveals snowstorm appearance of the mole, (diagnostic)
- Serum level B-HCG is markedly elevated, (less than 1,00,000/ 24 hours)
- X-ray chest: to exclude metastatic choriocarcinoma.
- Urine:
✓ (B-HCG-elevated (24 hrs)
✓ Pregnancy test – +ve. - Biopsy
4. Treatment:
- Suction curettage of the mole when no mole has been expelled out.
- Blood transfusion is to given simultaneously.
- Send the evacuated material for histopathology.
- D & C if there is no facility of suction curettage. After 7 days the procedure should be repeated because there is chance of attach something with the wall.
- If there is spontaneous expulsion of the mole, evacuation & curettage is to be done to remove the residual mole.
- Oxytocin:
✓ At the beginning in suction curettage
✓ At the half way in D & C. - Antibiotics
- Hysterectomy if >40 yrs& complete family.
[Role of hysterectomy in H. mole: No role; even in choriocarcinoma. Tumor is 100% curable. But it is indicated in pt. got perforated invasive mole, old pt. with completed family.]
Follow up of H. mole:
- Follow up of a pt. with H. mole after evacuation:
A. Advises of pt. after evacuation:
- She must be followed up for 2 yrs.
- She must not be pregnant within 2 yrs.
- Contraception should be barrier method for 1st 4 n…ths & then oral contraceptive method should be used.
B. Follow up schedule:
- Come after 15 days – History taking & S. HCG level is seen.
- Every month for 1st 6 months.
- 3 monthly for next 6 months.
- Then 6 monthly for 1 yr.
C. Following history should be taken:
- H/O menstruation (Amenorrhoea)
- H/O irregular P/V bleeding.
H/O metastasis:
- Haemoptysis, dyspnoea, chest pain.
- Paresis & paralysis, headache, visual disturbance.
- Nodule in the vulva & vagina.
- Haematemesis, abdominal pain.
- Haematuria.
Following clinical exam, should be done:
- G/E: Anaemia, pulse, BP, wt.
- P/A/E: enlargement. exclude to uterine
- P/V/E:
- Speculum exam to see any deposits over the vulva, vagina, fornix & urethra.
- Bimanual exam, to see-
✓ Size of the uterus
✓ Lutein cyst of the ovary.
Following lab inv. should be done:
a. B-HCG level in serum
- Weekly for 1st month (till 3 consecutive levels are found to normal. Normally -ve within a week)
b. Every month in 1styr.
- Chest x-ray for metastasis (cannon ball appearance, if metastasize)
F. Prophylactic Rx: Chemotherapy:
- Methotrexate with folinic acid.
- Methotrexate for 4 days. Then folinic acid for 4 days.
Indication of chemotherapy during follow up:
- Raised hCG level 6 months after evacuation (even if falling).
- hCG plateau in three consecutive serum samples.
- hCG>20,000 IU/I more than 4 weeks after evacuation.
- Rising hCG in two consecutive serum samples.
- Pulmonary, vulval or vagínal mets unless the hCG level is falling.
- Heavy PV bleeding or Gl/intraperitoneal bleeding.
- Histological evidence of choriocarcinoma.
- Brain, liver, Gl metastases or lung metastases >2 cm on CXR.
[Ref by-D. C. Dutta’s Obs/9th]
Complications of H.M:
Immediate complications:
➤ Bleeding & shock leading to death.
➤ Electrolytes imbalance.
➤ Infection
➤ DIC
Late complications:
➤ Choriocarcinoma (2-4%) in future.
➤ Metastasis to lung and other organs of the body.
➤ Perforation of uterus due to-
➤ Invasiveness of mole
➤ Evacuation of mole by instruments.
[Ref by-D. C. Dutta’s Obs/9th]