Induction of Labour – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.

Induction of Labour
Induction of labour:
Induction of labour means deliberate termination of pregnancy beyond 28wks by any method which aims at initiation of labour and a vaginal delivery.
Or
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing labor can be accomplished with pharmaceutical or non-pharmaceutical methods.
[N.B. When the termination is done for maternal interest, the induction is to be done ignoring the gestational period.
When the induction is done for fetal interest, a fair idea about the maturity of fetus has to be obtained with available parameters prior to induction.]
Indications of induction of labour:
A.Fetal:
Continuation of pregnancy may adversely affect the foetal prognosis without affecting the mother.
- Post maturity.
- Previous H/O unexplained IUD.
- DM
- Chronic placental insufficiency leading to growth retardation of foetus (IUGR).
- Rh-immunization.
- Unstable lie-after correcting into longitudinal lie.
B. Maternal:
Continuation of pregnancy may adversely affect the mother without affecting the foetus.
- Hypertensive disorder of pregnancy
✓ Eclampsia
✓ Pre-eclampsia - IUD of foetus.
- Disorder of the amniotic fluid)
✓ Polyhydramnios
✓ Oligohydramnios - Chronic hydramnios with maternal distress.
- Antepartum haemorrhage.
- Congenital malformation of the foetus.
- Uncontrollable choriogravisarum.
C. Combined:
Continuation of pregnancy adversely affects both the mother & the baby.
- Pre-eclampsia & eclampsia.
- Lesser degree of placenta previa.
- Abruption placenta.
- Premature rupture of membranes.
- Chronic HΙΝ.
- Chronic renal disease.
Contra-indication of induction of labour:
- Contacted pelvis.
- Cephalo-pelvic disproportion.
- Persistent malpresentation
✓ Transverse lie
✓ Oblique lie
✓ Breech presentation - Pregnancy with previous Caesarean section.
- Elderly primigravida specially associated with complicating factors.
- Heart disease.
- High risk pregnancy with compromised fetus.
- Pelvic tumors.
- History of previous hysterectomy.
- Umbilical cord prolapse.
- Cervical carcinoma.
Monitoring a patient after medical induction:
Monitoring of maternal condition:
General examination:
- Pallor for anaemia (for rupture of uterus or any haemorrhage).
- State of hydration (dehydration / oedema).
- Blood pressure (for both hypotension & hypertension).
- Pulse rate (rate, regularity & volume).
- Temperature.
- Respiratory rate.
- Cyanosis.
- Urine output.
Progress of the labour: By strict monitoring of partograph (mandatory).
Per-abdominal:
- Any sign of rupture uterus (sudden onset, sharp, agonizing tearing lower abdominal pain or even cessation of pain).
- Number, intensity of uterine contraction & duration in between them.
Per-vaginal:
- Any P/V discharge.
- Any P/V bleeding (even a small amount).
Respiratory:
- Lung field auscultation (for signs of bronchospasm) to evaluate any sort of dyspnoea.
- Any signs of respiratory failure.
CNS:
- Any signs of CNS depression (J alertness, mentation, concentration, orientation or confusion or even coma).
- Glasgow-coma scale (GCS) score.
CVS:
- Any signs of ischaemic chest pain &/or arrhythmia.
- Any signs of heart failure (dyspnoea, leg oedema, crepitations over lung base, cyanosis etc).
Others:
- Any signs of drug hypersensitivity.
- Any signs of limb ischaemia or gangrene (for ergot derivatives).
Monitoring of fetal condition:
- FHR- frequently checked to detect fetal distress.
- Colour of liquor amnii. (Clear, green, meconium or blood stained).
Complications of induction of labour
A. Complication for mother:
- Uterine inertia &prologedlabour.
- Obstructed labour.
- Intrauterine infection.
- Increase chance of operation.
- Increase purperial complications.
- PPH.
B. Complication for fetus:
- Risk of pre-maturity if EDD has been inaccurately calculated.
- Physical injury due to precipitous delivery.
- Prolapse of the cord may follow amniotomy
- Injurious administration of oxytocin or inadequate observation during induction could lead to fetal damage or delivery of a baby with poor APGAR score.
Factors for mother &foetus counted in the successful inductions of labour:
1. Period of gestation: The uterus is more sensitive nearer to term or post term.
2. Case profile: The induction is more successful in parous women or in cases with premature rupture of the membrane. The uterus is likely to be less responsive in elderly primigravida or in cases of prolonged retention of dead fetus.
3. Sensitivity of the uterus: The induction is likely to be successful if:
- The uterus readily contracts on massaging.
- By employing oxytocin sensitivity test the response occurs with 0.04 units or less of oxytocin. Positive oxytocin sensitivity test is more favorable.
4. Pre-induction scoring: Amongst many a scoring system, Bishop’s scoring still maintains popularity. The scoring system takes into consideration of cervical factor and station of the head. The dilatation of the cervix, however the single factor of great importance.
Bishop’s score:
It is a scoring system by which assessment for induction of labour is done.
This is an accepted method of recording the degree of ripening of cervix before labour. It considers the length, dilataion, consistency and position of the cervix as well as the level of the fetal head that is station.
Components:
- Cervical factors
- Station of the head
Bishop’s pre-induction cervical scoring system:
| Factors | Score | |||
| 0 | 1 | 2 | 3 | |
Cervix
|
|
|
|
|
Head
| -3 | -2 | -1,0 | +1,+2 |
Interpretation:
- Total score=13
- Favorable score-6-13
- Unfavorable = 0-5
Types of induction of labour:
Medical induction:by
- Oxytocin
- Prostaglandins
✓ PGE1
✓ PGE2
✓ PGF2a - Steroid receptor antagonists: Mifepriston
Surgical induction:
- Artificial rupture of membranes (ARM)
✓ Low rupture of the membranes
✓ High rupture of the membranes act - Stripping the membranes
Combined: Both medical and surgical induction:
Oxytocic drugs:
- Oxytocin
- Ergot derivatives: Ergometrine, methergin
- Prostaglandins:PGE2, PGE2
Medical uses:
Commonly accepted medical reasons for induction include:
❖ Post term pregnancy, i.e. if the pregnancy has gone past the end of the 41st week.
❖ Intrauterine fetal growth restriction (IUGR).
❖ There are health risks to the woman in continuing the pregnancy (e.g. she has pre- eclampsia).
❖ Premature rupture of the membranes (PROM); this is when the membranes have ruptured, but labor does not start within a specific amount of time.
❖ Premature termination of the pregnancy (abortion).
❖ Fetal death in utero and previous history of stillbirth.
❖ Twin pregnancy continuing beyond 38 weeks.
❖ Previous health conditions that puts risk on the woman and/or her child such as diabetes, high blood pressure
Induction of labor in those who are either at or after term improves outcomes for the baby and decreases the number of C-sections performed.
Methods of induction of labor:
Methods of inducing labor include both pharmacological medication and mechanical or physical approaches.
Mechanical and physical approaches can include artificial rupture of membranes or membrane sweeping. The use of intrauterine catheters are also indicated. These work by compressing the cervix mechanically to generate release on prostaglandins in local tissues. There is no direct effect on the uterus.
Pharmacological methods are mainly using either dinoprostone (prostaglandin E2) or misoprostol (a prostaglandin El analogue)
A. Medication
- Intravaginal, endocervical or extra-amniotic administration of prostaglandin, such as dinoprostone or misoprostol. Prostaglandin E2 is the most studied compound and with most evidence behind it. A range of different dosage forms are available with a variety of routes possible. The use of misoprostol has been extensively studied but normally in small, poorly defined studies. Only a very few countries have approved misoprostol for use in induction of labor.
- Intravenous administration of synthetic oxytocin preparations. A high dose does not seem to have greater benefits than a standard dose.
- Use of mifepristone has been described but is rarely used in practice.
- Relaxin has been investigated, but is not currently commonly used.
- Mnemonic”ARNOP”: Antiprogesterone, relaxin, nitric oxide donors, oxytocin, prostaglandins
B. Non-pharmaceutical
- “Membrane sweep”, also known as membrane stripping, or “stretch and sweep” in Australia and the UK during an internal examination, the practitioner moves their finger around the cervix to stimulate and/or separate the membranes around the babyfrom the cervix. This causes a release of prostaglandins which can help to kick-start labor.
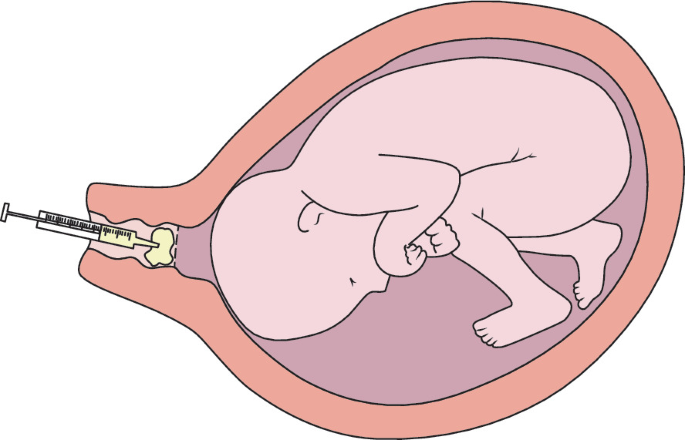
- Artificial rupture of the membranes (AROM or ARM) (“breaking the waters”)
- Extra-amniotic saline infusion (EASI), in which a Foley catheter is inserted into the cervix and the distal portion expanded to dilate it and to release prostaglandins.
- Cook Medical Double Balloon known as the Cervical Ripening Balloon with Stylet for assisted placement is FDA approved. The Double balloon provides one balloon to be inflated with saline on one side of the uterine side of the cervix and the second balloon to be inflated with saline on the vaginal side of the cervix.
