Infection Control -Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Infection Control
Definition of Infection:
Infection may be defined as the invasion and multiplication of microorganisms such as bacteria, viruses, and parasites that are not normally present within the body. An infection may cause no symptoms and be subclinical, or it may cause symptoms and be clinically apparent.
Or,
Entry of a harmful microbe into the body and its multiplication in the tissues / bloodstream is called infection.
According to WHO infection control may be defined as “infection prevention and control measures aim to ensure the protection of those who might be vulnerable to acquiring an infection both in the general community and while receiving care due to health problems, in a range of settings. The basic principle of infection prevention and control is hygiene.”
Or,
Infection Control in a health care facility is the prevention of the spread of microorganisms from:
- Patient to patient
- Patient to Staff member
- Staff member to patient
General Measures of Infection Control:
A. Isolation
Assess the need for isolation. Screen all intensive care unit (ICU) patients for the following:
- Neutropenia and immunological disorder
- Diarrhea
- Skin rashes
- Known communicable disease
- Known carriers of an epidemic strain of bacterium.
B. Observe hand hygiene
World Health Organization’s five moments for hand hygiene
- Before touching a patient to protect the patient from harmful germs carried on your hands
- Before aseptic procedures to protect the patient against harmful germs, including the patient’s own germs
- After body fluid exposure/risk-to protect yourself and the health care environment from the harmful patient’s germs
- After touching the patient-to protect yourself and the health care environment from the harmful patient’s germs
- After touching the patient’s surrounding to protect yourself and the health care environment from the harmful patient’s germs.
C. Follow standard precautions
Standard precautions include prudent preventive measures to be used at all times, regardless of a patient’s infection status.
a) Gloves: Sterile gloves should be worn after hand hygiene procedure while touching mucous membrane and non-intact skin and performing sterile procedures (2A) e.g. arterial, central line and Foley catheter insertion
b) Gown: Wear a gown to prevent soiling of clothing and skin during procedures that are likely to generate splashes of blood, body fluids, secretions or excretions (IB)
c) Mask: eye protection/face shield
- Wear a mask and adequate eye protection (eyeglasses are not enough), or a face shield to protect mucous membranes of the eyes, nose and mouth during procedures and patient care activities
- Patients, relatives and health care workers (HCWs) presenting with respiratory symptoms should also use masks (e.g. cough).
d) Shoe and head coverings
- Required for visitors.
e) Patient-care equipment
- Used patient-care equipment soiled with blood, body fluids, secretions, or excretions should be handled carefully to prevent skin and mucous membrane exposures
- Ensure that single use items and sharps are discarded properly.
D. Follow transmission-based precautions
a) Airborne precautions
- Isolate with negative-pressure ventilation
- Respiratory protection must be employed when entering the isolation room ob
b) Contact precautions
- Isolation is required
- Non-critical patient-care equipment should preferably be of single use. If unavoidable, then clean and disinfect them adequately before using to another patient
- Limit transport of the patient
- Droplet precautions
- Isolation is required
- Respiratory protection must be employed when entering the isolation room or within 6-10 ft of the patient. Limit transport of the patient
- Use specific strategies focused on prevention of specific nosocomial infections
E. Strategies to reduce VAP (ventilator-associated pneumonia)
- Avoid intubation whenever possible
- Consider noninvasive ventilation whenever possible
- Prefer oral intubations to nasal unless contraindicated
- Keep head elevated at 30-45° in the semi-recumbent body position
- Daily oral care with chlorhexidine solution of strength 0.12%
F. Strategies to reduce CRBSI (Catheter-related bloodstream infection)
- Prefer the upper extremity for catheter insertion. Avoid femoral route for central venous cannulation (CVC)
- Use maximal sterile barrier precautions (cap, mask, sterile gown and sterile gloves) and a sterile full-body drape while inserting CVCs, peripherally inserted central catheters, or guidewire exchange (IA)
G. Strategies to reduce UTI
- Insert catheters only for appropriate indications
- Follow aseptic insertion of the urinary catheter)
- Maintain a closed drainage system
- Remove the catheter when it is no longer needed
H. Consider environmental factors
- Cleaning and disinfection
- Organizational and administrative measures of
- Work with hospital administration for better patient to nurse ratio in the ICU
- Policies for controlling traffic flow to and from the unit to reduce sources of contamination
- from visitors, staff and equipment
- Waste and sharp disposal policy
- Education and training for ICU staff about prevention of nosocomial infections
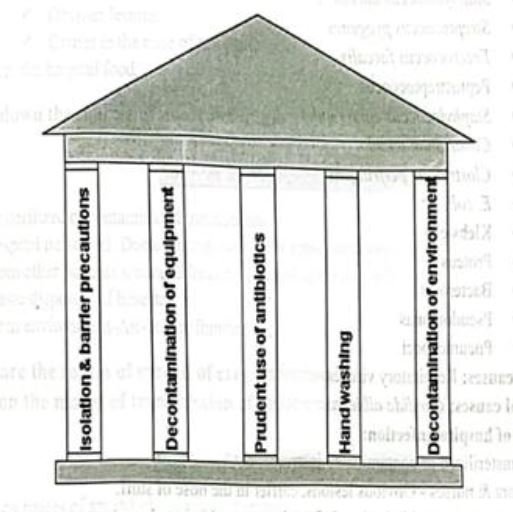
- Isolation and barrier precautions
- Decontamination of equipment
- Prudent use of antibiotics
- Hand washing
- Decontamination of environment
Hospital Acquired Infection / Cross Infection/Nosocomial
Infection
Hospital Acquired Infection/Cross Infection/Nosocomial Infection:
Infections developing in patients in hospitals or other healthcare facilities after 48 hours of admission
which are not present or incubating at the time of admission.
They occur in 5-15% of patients admitted to hospital
Or,
A hospital-acquired infection (HAI), also known as a nosocomial infection, is an infection that is acquired in a hospital or other health care facility. To emphasize both hospital and nonhospital settings, it is sometimes instead called a health care-associated infection (HAI or HCAI).

Causes of Nosocomial Infection:
Organisms responsible for hospital infection:
A. Bacterial causes:
- Staphylococcus aureus
- Streptococcus pyogenes
- Enterococcus faecalis
- Peptostreptococcus
- Staphylococcus epidermidis
- Clostridium tetani.
- Clostridium perfringens
- E. coli
- Klebsiella
- Proteus
- Bacteroids
- Pseudomonas
- Pneumococci
B. Viral causes; Respiratory viruses.
C. Fungal causes; Candida albicans.
Common sources of hospital infection:
- From the unsterilized or contaminated instruments.
- From doctors & nurses-Obvious lesions, carrier in the nose of stuff.
- From the patient’s wound infection, infected urine, and infected stool.
- From environment-Air-born, Fomites.
Common Types of Nosocomial Infection:
1. Hospital-acquired pneumonia
- Ventilator-associated pneumonia
2. Urinary tract infection
3. Gastroenteritis
4. Puerperal feverah

Types of Nosocomial Infection:
Endogenous infection: Arise from patient himself while he is in the hospital –
- Wound infection.
- Infected urine.
- Infected stool.
- Following perforated peptic ulcer.
Exogenous infection:
Derived from hospital environment:
- Airborne.
- Fomites.
From the unsterilized or contaminated instruments.
From doctors & nurses:
- Obvious lesions.
- Carrier in the nose of the stuff.
From the hospital food.
Sources of Nosocomial Infection:
- Unsterilized or contaminated instruments.
- Hospital personnel: Doctor, nurse, ward boy (obvious lesions, carrier in the nose of the stuff).
- From other patients wound infection, infected urine and infected stool.
- Waste disposers of hospital.
- From environment-Air-borne, fomites.
Routes of Spread of Cross Infection:
The common routes of spread of cross infection are-
1. Direct contact: i.e. the organism may be transferred directly from the hands of a nurse or doctor to a susceptible patient.
2. Droplet infection: e.g. droplets released from nose and throat through coughing or sneezing.
3. Air-borne particles.
4. Release of hospital dust into the air.
5. Through various hospital procedures,-
- Catheterization.
- Intravenous procedures.
- Infected cat gut
- Dressings.
- Sputum cups.
- Bed pans.
- Urinals
Common Risk Factors of Nosocomial Infection:
Risk factors three main criteria broadly enclose the factors predisposing a patient to infection in a hospital setting:
Increased susceptibility:
Evidently, patients admitted in hospitals have poor state of health, which means lower defense quality against bacteria. This group includes-
- Elderly.
- Premature babies.
- Immunodeficient (because of drug abuse, illness or irradiation therapy).
- Additionally patients with Chronic Obstructive Pulmonary Diseases have specifically increased chances of respiratory tract infection.
Invasive devices:
- For instance intubation tubes.
- Catheters.
- Surgical drains.
- Tracheotomy tubes.
Patients already colonized on admission are instantly put at greater risk when they undergo an invasive procedure.
Medications or treatment (e.g. repeated blood transfusions) themselves make the patient vulnerable to infections, e.g. antacid treatment or antimicrobial therapy (which eliminates competitive flora and allows flourishing of resistant organisms).

Prevention of Nosocomial Infection/Hospital Acquired Infection:
1. Sterilization: Proper sterilization method should be maintained in the hospital settings for the prevention of nosocomial infection.
2. Isolation: Isolation precautions are designed to prevent transmission of microorganisms by common routes in hospitals. Because agent and host are more difficult to control.
3. Hand washing and gloving: Hand washing frequently is called the single most important measure to reduce the risks of transmitting skin microorganisms from one person to another. Gloving is very essential to reduce the risk of transmitting microorganisms from one person to another.
4. Where possible use of single use disposable items.
5. Ensuring an effective administrative set up.
6. Rational use of antibiotics
7. Proper hospital waste disposal
8. Active oversight within the hospital.
9. Wearing an apron during patient care to reduce the risk of infection. The apron should either be disposable or be used only when caring for a specific patient.
10. Adoption of effective aseptic techniques.
11. Detection of the carriers & proper treatment.
Prevention and control of hospital acquired/nosocomial Infection:
Isolation: Infectious patients must be isolated.
¤ Hospital staff: Those who are suffering from skin diseases, sore throat, common cold, ear infection, diarrhoea or dysentery or other infectious aliments should be kept away from work until completely cured.
¤ Hand washing: A suitable disinfectant must be employed for hand washing when dealing with patients.
¤ Dust control: Suppression of dust by wet dusting and vacuum cleaning are important control measures.
¤ Disinfection: The articles used by the patients as well as patient’s urine, faeces and sputum should be properly disinfected.
¤ Control of droplet infection: Use of face masks, proper bed spacing, prevention of overcrowding and ensuring adequate lighting and ventilation are important control measures.
¤ Nursing techniques: Barrier nursing and task nursing to minimize cross infection.
¤ Administrative measures: To formulate policies regarding admission of infectious cases, isolation facilities, disinfection procedures, and in fact all matters relating to control of hospital acquired infection.
(Ref by-Park/24th/376)
Roles and Responsibilities of a Nurse to Prevent Nosocomial Infection
The followings are specific preventive measures all nurses should carry out:
¤ Awareness of the possible risk of infection among hospitalized patient.
¤ Catheter associated urinary tract infections are the cause of hospital associated infections. If possible avoid the use of indwelling catheters, use an alternate form of drainage such as condom drainage, suprabubic catheterization or intermittent catheterization. If an indwelling catheter must be used it should be removed promptly when no longer needed.
¤ Great care must be exercised in using and sterilizing respiratory therapy equipment. Every precaution should be taken to reduce the possibility of aspiration.
¤ Prolonged IVV, therapy should be avoided. Scrupulous attentions should be paid to inserting the needle properly, protecting the needle site and observing and caring for VV set up.
¤ Use all surveillance and preventive methods known to provide the safest possible environment for patients, personnel and visitors.
¤ Fundamental to the control of infection are current hand washing procedures and strict aseptic technique applied to all diagnostic and therapeutic procedures involving the use of catheters, cardiac pacing, VV therapy, endotracheal and tracheostomy tube drainage and wound care.
