Inflammatory bowel disease – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Inflammatory bowel disease
Definition of IBD:
Inflammatory bowel disease (IBD) is an idiopathic and chronic intestinal inflammation which pursue a protracted relapsing and remitting course, usually extending over years.
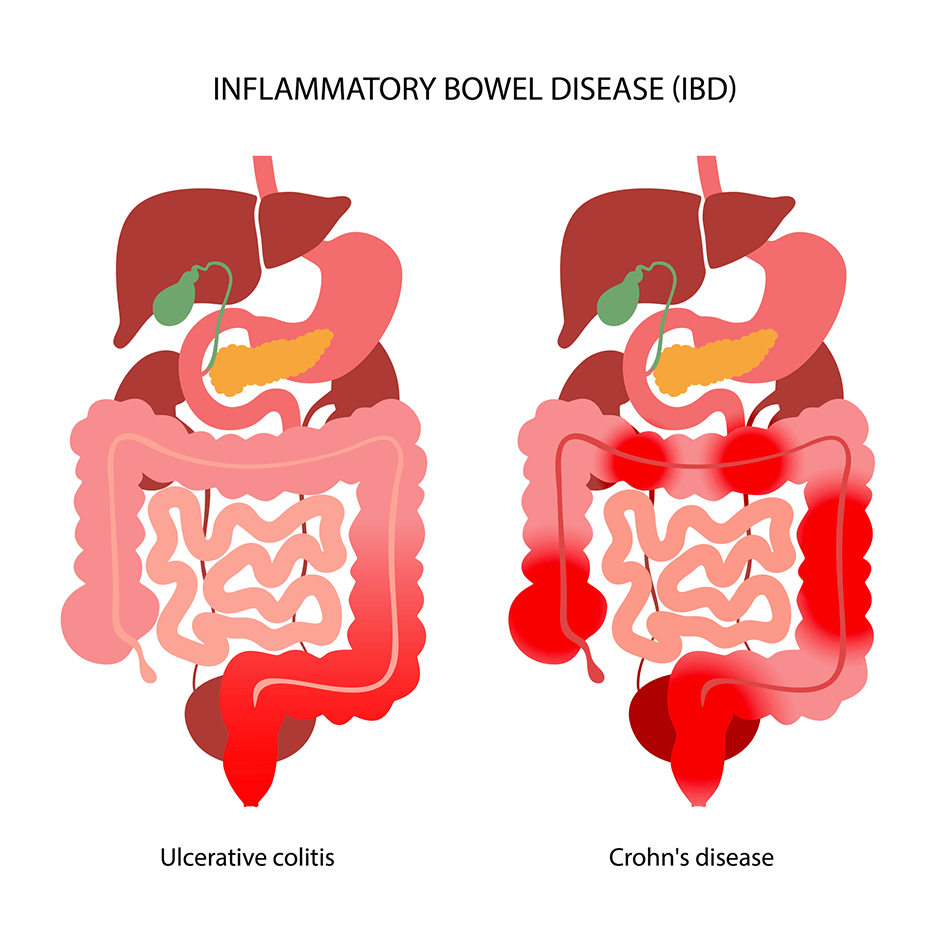
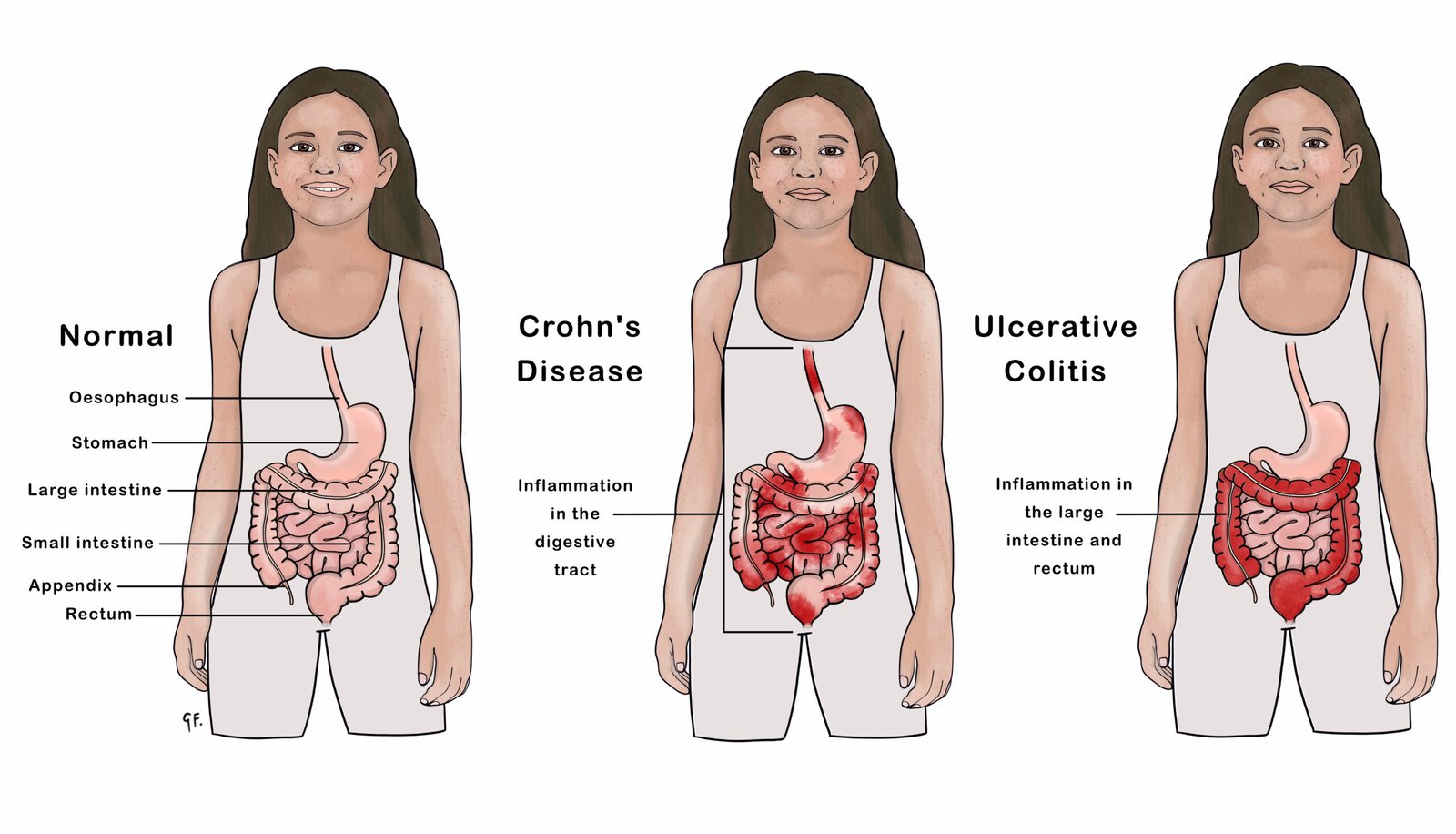
Types of Inflammatory Bowel Disease:
⇒ Ulcerative colitis (Involve usually colon)
⇒ Crohn’s disease. (Involve any part of GIT)
Distribution Of Ulcerative Colitis:
1. Proctitis or Proctosigmoiditis. (40-50%)
2. Left-sided or extensive colitis (30-40%)
3. Pancolitis (20%).
Distribution of Crohn’s disease (Involve any part of GIT):
1. Ileal or ileocolonic 40%
2. Small intestinal 30–40%
3. Crohn’s colitis 20%
4. Perianal disease 10%.
(Ref. Davidson-23/814)
Ulcerative Colitis
Definition of Ulcerative Colitis:
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in digestive tract.
Clinical Type and Presentation/ Sign Symptoms:
Major symptoms-
- Bloody diarrhoea
- First attack-most severe then-
- Relapse & remission.
a. Proctitis:
- Rectal bleeding with mucus.
- Tenesmus.
- Either small volume frequent stool/or
- Constipated and pass pellety stool.
- No constitutional symptom.
b. Proctosigmoiditis:
- Bloody diarrheoa with mucus.
- Some has constitutional symptom. Fever, lethargy & abdominal discomfort.
c. Extensive colitis:
- Bloody diarrhoea with mucus.
- Anorexia
- Malaise
- Weight loss
- Abdominal pain
- Fever.
- Tachycardia/palpitation.
Laboratory Investigation:
a. Blood TC,DC, ESR,CRP, Hb%, albumin
- Anaemia resulting from bleeding or malabsorption of iron, folic acid or vitamin B12.
- ESR & CRP- Raised.
- Serum albumin-fall
b. Stool routine/microscopy & culture
c. Blood cultures
d. Colonoscopy/ Sigmoidoscopy:
- Loss of vascular pattern.
- Granularity.
- Friability
- Ulceration.
e. Radiograph:
i. Ba enema:
- Shortened tubular colon.
- Loss of haustration
- Psudopolyp.
ii. Plain X ray abdomen:
- Dilatation of the colon.
- Mucosal oedema (thumb printing)
f. MRI
Treatment of Ulcerative Colitis:
Aims of Treatment:
i. Treat acute attacks.
ii. Prevent relapse.
iii. Detect carcinoma at an early stage
iv. Select pt. for surgery.
Medical Management:
a. Active proctitis:
- First line: Oral aminosalisylate (Salfasalazine or mesalazine) +Local aminosalisylate ( mesalazine enema).
- Fail to respond: Oral Prednisolone 40 mg/day orally for 2 weeks & reduced slowly over 8 weeks.
b. Left sided or extensive colitis:
Oral aminosalisylate (Salfasalazine or mesalazine) +Local aminosalisylate (mesalazine enema)
+
Oral Prednisolone 40 mg/daily.
c. Severe ulcerative colitis:
- Intravenous fluids
- Transfusion if Hb < 100 g/L
- I.V methylprednisolone (60 mg daily) or hydrocortisone (400 mg daily)
- Antibiotics for proven infection
- Nutritional support
- Subcutaneous heparin for prophylaxis of venous thromboembolism
- Avoidance of opiates and antidiarrhoeal agents
- Consider infliximab (5 mg/kg) in stable patients not responding to 3-5 days of corticosteroids
Urgent colectomy:
- Patients who develop colonic dilatation (> 6 cm)
- Clinical and laboratory measurements deteriorate
- Do not respond after 7-10 days’ maximal medical treatment
d. Maintenance of remission: (Life-long maintenance therapy)
- Relapse more than once a year.
- Oral aminosalicylates-either mesalazine or Sulfasalazine -are first-line agents.
- Patients who frequently relapse despite aminosalicylate drugs are treated with Azathiopurines
Surgical Mx:
- a) Panproctocolectomy with ileostomy or
- b) Proctocolectomy with ileal-anal pouch anastomosis
(Ref-Davidson/234/820-823)
Nice to know:
Indications for Surgery in Ulcerative Colitis:
i. Impaired quality of life
- Loss of occupation or education.
- Disruption of family life
ii. Failure of medical therapy
- Dependence upon oral corticosteroids
- Complications of drug therapy
iii. Fulminant colitis
iv. Disease complications unresponsive to medical therapy
- Arthritis
- Pyoderma gangrenosum
v. Colon cancer or severe dysplasia
(Ref-Davidson/234/823)
Nursing Management of Ulcerative Colitis:
1. Monitor Vital signs, patient’s bowel movements (what does it look like and its frequency), keep patient hydrated, monitor daily weights (for weight loss), focus on GI assessment (bowel sounds: hyperactive, hypoactive, or absent, tenderness)
2. Signs and symptoms of toxic mega-colon: abdominal distention, fever, diarrhea, abdominal pain, dehydration, tachycardia, hypoactive or absent bowel sounds
3. Signs and Symptoms of peritonitis: distention or abnormal bloating, increased heart rate, tachypnea, pain (note toxic megacolon can lead to peritonitis)
4. May need NPO with IV hydration. Provide advance diet as per Doctor order as symptoms subside will typically start with clear, fulls, and then solids
5. Diet Education:
➤ Watch foods that can cause a “flare-up” or should be avoided during a “flare-up”:
- High-fiber foods (they require a lot of digestion and the gut needs to rest)
- Food hard to digest like: nuts, raw vegetables or fruits (cooked are better)
- Allergen type foods: dairy or certain foods that the person may be intolerant too
- like wheat, fish Avoid spicy, high-fat foods, gluten, gas causing foods like onions, beans etc.
➤ Foods to eat during “flare-up” or to prevent one:
- Low fiber (easier on the gut to digest), high-protein and stay bydrated
6. Importance about regular screening of colon cancer
7. If patient had surgery, educate about ostomy placement: know the nursing pre and post care, how to provide ostomy care (diet, how to change pouching system, stoma care etc.)
8. Administering Medications per Doctor Order:
➤ Anti-inflammatory: decrease the inflammation in the bowel
- 5-Aminosalicylates (5-ASA): “Sulfasalazine”
- Steroids: “corticosteroids”
➤ Immuno-suppressors/modulators: used when other medications haven’t work or patient needs to be off of steroids due to their side effects
➤ Antibiotics: treat or prevent infections during flare-ups “Ciprofloxacin”
9. Surgery:
➤ Proctocolectomy: complete removal of the colon and rectum…
➤ Ileoanal anastomosis (J-pouch)
Comparison between Ulcerative Colitis & Crohn’s Diseases:
| Traits | Ulcerative colitis | Crohn’s disease |
| Age group | Any | Any |
| Gender | M-F | Female |
| Ethnic group | Any | Any, more common in Ashkenazi Jews |
| Genetic factors | HLA-DR103 associated with severe disease | CARD 15/NOD-2 mutations predispose |
| Risk factors | More common in non-/ex-smokers | More common in smokers |
| Anatomical distribution | Colon only, begins at anorectal margin with variable proximal extension | Any part of gastrointestinal tract; perianal disease common, patchy distribution-‘skip lesions’ |
| Extra-intestinal manifestations | Common | Common |
| Presentation | Bloody diarrhoea | Variable, pain, diarrhoea, weight loss all common |
| Histology | Inflammation limited to mucosa; crypt distortion, cryptitis, crypt abscesses, loss of goblet cells | Submucosal or transmural inflammation common; deep fissuring ulcers, fistulae; patchy changes; granulomas |
| Management | 5-ASA; corticosteroids, azathioprine; colectomy is curative | Corticosteroids; azathioprine; methotrexate; infliximab, nutritional therapy; surgery for complications is not curative |
Crohn’s Disease
Definition of Crohn’s Disease:
Crohn’s disease is a chronic inflammatory disease of the digestive tract. Symptoms include abdominal pain and diarrhea, sometimes bloody, and weight loss.
Or,
Crohn’s disease is an inflammatory bowel disease (IBD). It causes inflammation in digestive tract, which can lead to abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition.
Management of Crohn’s Disease:
Clinical features:
Symptoms
- Abdominal pain.
- Diarrhoea.
- Weight loss.
- Sub-acute or acute intestinal obstruction – Vomiting, constipation.
Signs:
- Evidence of weight loss.
- Anaemia, & apthous ulceration
- Glossitis and angular stomatitis.
- Abdominal tenderness, most marked over the inflamed area.
- An abdominal mass due to matted loops of thickened bowel or an intra-abdominal abscess may occur.
- Perianal skin tags, fissures or fistulae
Investigations
1. Full blood count with ESR:
- Anaemia resulting from bleeding or malabsorption of iron, folic acid or vitamin B12
- ESR & CRP-raised
2. Serum albumin concentration:
- Low (because of protein-losing enteropathy reflecting active and extensive disease)
3. Bacteriology:
- Stool cultures
- Blood cultures
4. Colonoscopy with biopsies:
- Patchy inflammation with discrete, deep ulcers, perianal disease (fissures, fistulae and skin tags) or rectal sparing occurs.
5. Barium follow through-Narrowed & ulcerated & multiple stricture-are common
6. Straight abdominal X-ray:
- Evidence of intestinal obstruction or displacement of bowel loops by a mass
7. MRI: Delineating pelvic or perineal involvement.
Treatment
Aims of Treatment:
i. Treat acute attacks.
ii. Prevent relapse.
iii. Detect carcinoma at an early stage
iv. Select pt. for surgery.
Medical Management:
- Induction of remission in active disease &
- Maintenance of remission.
a. General measures:
➤ Diet-high protein, low fat & milk free
➤ Supplement of iron, B12, folic acid & zinc
➤ Symptomatic treatment for diarrhoea & blind loop syndrome
➤ Blood transfusion if Hb < 10 gm/dl.
➤ Nutritional support.
➤ Antibiotics for proven infection.
b. Medical therapy/Drugs:
➤ Active ileocolitis & colitis:
- Oral aminosalisylate (Salfasalazine or mesalazine) or Oral Prednisolone
- In severe disease intravenous steroids.
➤ Isolated ileal disease:
- Corticosteroids (Budesonide)
➤ Active Crohn’s disease at any site within the gastrointestinal tract-
- Intravenous infusion 4-8-weekly on three occasions
➤ Patients with diffuse and extensive ileocolonic involvement:
- A combination of drug therapies, nutritional support, surgical intervention and endoscopic balloon dilatation of stricture
c. Fistulas and perianal disease:
➤ Simple perianal disease metronidazole and/or ciprofloxacin
➤ Thiopurines are used in chronic disease
➤Infliximab and adalimumab heal enterocutaneous fistulas and perianal disease
➤ Surgical intervention
d. Maintenance of remission: (Life-long maintenance therapy)
➤ Patients who relapse more than once a year should be treated with thiopurines (Azathioprine).
➤ Patients who are intolerant of or resistant to thiopurines should be treated with once-weekly methotrexate combined with folic acid.
➤ Patients with aggressive disease are managed using a combination of immunosuppressives and anti-TNF therapy
d. Surgical treatment:
Surgery is not curative
If obstruction, fistula or abscess formation.
➤ Extensive colitis require total colectomy.
➤ Segmental resection and/or multiple stricturoplasties are done in localized segments of Crohn’s colitis.
➤ Seton drainage, fistulectomy and use of advancement flaps are appropriate for complex fistula in combination with medical therapies.
(Ref-Davidson/23/816-823)