Instrumental deliveries – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Instrumental deliveries
Instrumental deliveries:
1. Forceps delivery.
2. Vacuum extraction/ventouse delivery.
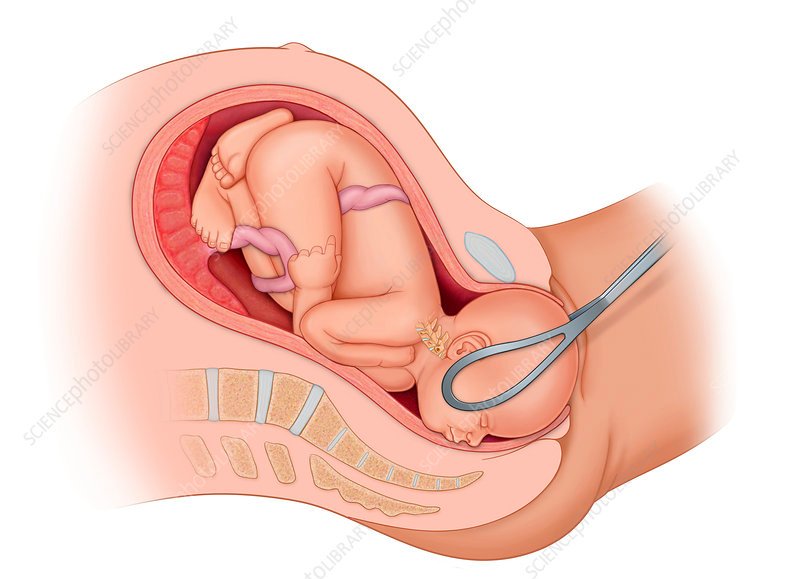
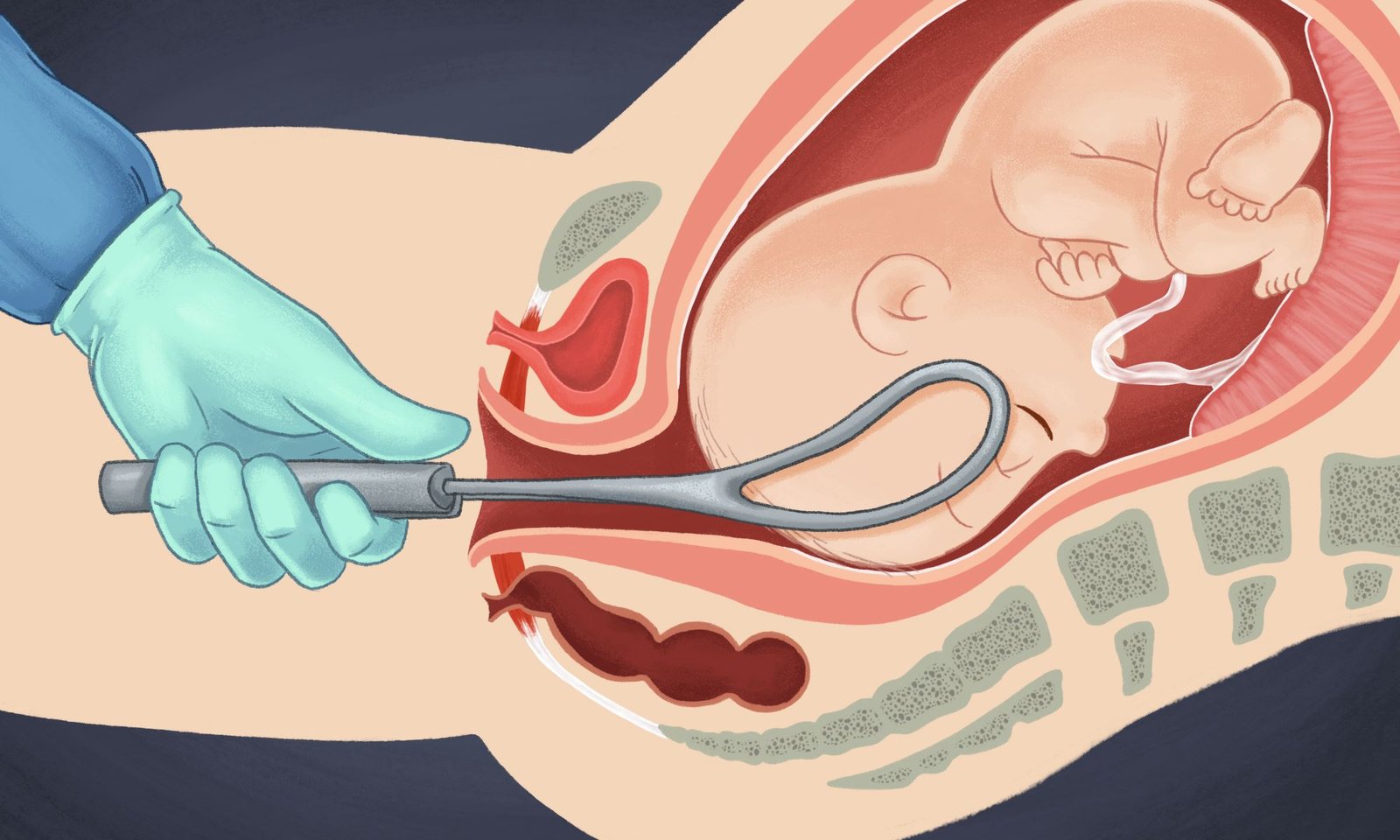
Forceps delivery:
Obstetric forceps is a pair of instruments specially designed to assist extraction of the fetal head & thereby accomplishing delivery of the fetus.
Classification of forceps delivery:
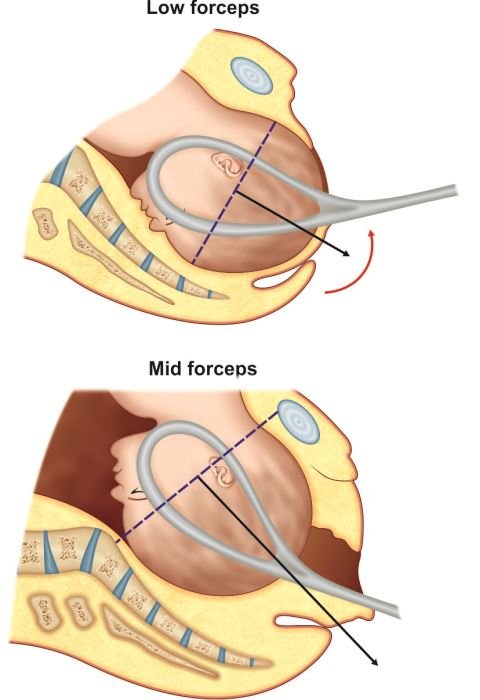
1. Low forceps (90%):
The head is near the pelvic floor or even visible at the introitus. It is commonly used now-a-days with advantages.
2. Mid forceps (10%):
It is used when head (station) is at or near the level of ischial spine. Internalrotation of the head is often incomplete. Manual rotation may be is needed before traction.
3. Outlet forceps:
It is a variety of low forceps where the head is on the perineum. Thus, all outletforceps are low forceps but not all low forceps are outlet forceps operations.
[Ref-D. C. Dutta’s Obs/8h/6511]
Varieties of obstetric forceps:
- Long curved forceps with or without axis traction device.
- Short curved forceps.
- Kielland’s forceps.
Criteria/conditions to be fulfilled before forceps operation:
a) Fetal & utero-placental criteria:
1. The fetal head mmust be engaged.
2. The cervix must be fully dilated.
3. The membranes must be ruptured.
4. The position & station of the fetal head must be known with certainty.
Maternal criteria:
1. Adequate analgesia
2. No major CPD
3. Urinary bladder must be empty
Others:
1. Experienced operator.
2. Verbal or written consent.
[Ref: D. C. Dutta’s Obs/9/531]
Indications of forceps delivery:
Maternal:
- Inadequate expulsive efforts.
- Maternal distress (exhaustion).
- Where expulsive efforts are to be avoided:
- Cardiac diseases.
- Eclampsia.
- Pre-eclampsia.
- Cerebro-vascular diseases.Fetal:
- Non-reassuring FHR (i.e. fetal distress) in –
✓ Low birth weight baby.
✓ Post maturity
Others:
- Prolonged 2nd stage of labour.
- To shorten the 2nd stage of labour in cases of-
✓ Cardiac diseases.
✓ Eclampsia.
✓ Pre-eclampsia.
✓Post caesarean pregnancy
[Ref-D. C. Dutta’s Obs/9/533]
Contraindications of forceps delivery:
- Brow presentation.
- Cervix not fully dilated.
- Contracted pelvis.
- Floating head (high station of head).
Important conditions to be fulfilled before forceps delivery:
1. Evidence of CPD must be excluded.
2. The cervix must be fully dilated.
3. The membranes must be ruptured.
4. The position & station of the fetal head must be known with certainty & the fetal head must be engaged.
Or (Another answer)
Prerequisites for forceps delivery:
- Cervix must be fully dilated, attempts to apply forceps blades with an undilated cervix will lead to much trauma and bleeding without successful delivery.
- Bladder must be empty. If necessary it should be emptied with a catheter. This prevents trauma and subsequent lack of bladder sensation.
- Membranes should be ruptured.
- Head must be engaged.
- No signs of cephalopelvic disproportion.
- Episiotomy should usually be performed to allow space for the posterior pull.
- Analgesia some form should be used: lignocaine pudendal block with infiltration to the vulva is sometimes enough. More anaesthesia (epidural or spinal) may be needed.
Failed forceps delivery:
When a deliberate attempt in vaginal delivery with forceps has failed to expedite the process, it is called failed forceps.
Treatment:
General:
- I/V fluid: Ringer’s lactate, Hartman’s solution, normal saline, 5%DA & DNS.
- Parenteral antibiotic.
- Blood transfusion (if necessary).
- Exclusion of ruptured uterus.
Specific treatment:
- Caesarean section is the treatment of choice.
- Ruptured uterus laparotomy.
- Dead fetus craniotomy.
[Ref-D. C. Dutta’s Obs/9/538]
Complications of forceps delivery:
1. Maternal
Immediate
Injuries:
- Cervical tear.
- Complete perineal tear.
- Vaginal laceration.
- Extension of injury to involve vaginal vault.
- Nerve injury: Femoral, Lumbo-sacral trunk.
- Complications of episiotomy if given.
Haematoma:
- Vulval haematoma.
- Vaginal haematoma.
Post-partum haemorrhage:
- Atonic or
- Traumatic or
- Both
Anaesthetic complications (following local or general anaesthesia)
Puerperal complications:
- Puerperal pyrexia.
- Puerperal sepsis.
- UTI
A. Remote:
- Painful perineal scars.
- Dyspareunia.
- Low back pain.
- Genital prolapse.
- Stress urinary incontinence.
- Sphincter dysfunction.
- Complications of episiotomy (if episiotomy is given).
2. Fetal complications:
Immediate:
- Cephalhaematoma.
- Facial palsy.
- Intra cranial haemorrhage.
- Asphyxia.
- Facial bruising.
- Skull fracture.
- Spinal injury (cervical).
Remote:
- Cerebral or spastic palsy due to residual cerebral injury (rare).
- Mental retardation.