Introduction to Orthopedic Nursing- An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
The two primary subfields of orthopedic nursing are unplanned and elective surgery. Thus, elective surgery is when a patient’s quality of life is improved by a limb replacement, such as a hip or knee replacement, that has been detected during routine checkups.Some patients suffer an unanticipated injury, like a fractured hip, maybe while out for a walk. Within 48 hours of arriving at A&E, they will probably be clerked, admitted to an orthopedic ward, and undergo surgery.
Introduction to Orthopedic Nursing
Orthopedics has come a long way since of Nicholas Andry, a French physician, who credited for coining the term, orthopaedic from two words in 1741 :
- Ortho meaning straight.
- Paedia meaning children.
Orthopaedics is the branch of medicine concerned with diseases, injuries, and conditions of the musculoskeletal system – relating to the body’s muscles and skeleton, and including the joints, ligaments, tendons, and nerves.
Or
Orthopedics is the branch of medical science concerned with disorders or deformities of the spine and joints.
[Reference: John Ebnezar’s, “Textbook of Orthopedics”, ed-4th, P-6]
The historical background of orthopedic nursing:
Orthopaedics is derived from two Greek words, orthos meaning straight and paidos meaning child. It was introduced in 1741 by Nicholas Andre in a volume work entitled Orthopaedia or The Art of Correcting and preventing deformities in Children. the 1″ Orthopaedics Institute was founded in Switzerland in 1780.
For many years, orthopedic practionnaires were known as “strape and buckle” doctors because of the
appliance the used to straighten body and limbs. Hugh Owen Thomas (1834-1891) become known for ability to set broken bones and reduce dislocate joints. Now a days it is known as Thomas splints.
Relatively little is known about the pioneers of orthopaedic nursing but one, but one name, Agnes Hunt(1862-1948) known as the “Florence Nightingle of the orthopaedic nursing”. She suffered an orthopaedic deformity in childhood but went on to open the “Baschurch Home” in oswestry, England, in1900. From modest beginnings, the home grew into a large orthopaedic hospital with a school for training orthopaedic nurses.
[Reference: Adult Orthopaedic Nursing, Lippincott, P-2]
Definition of orthopedic nursing:
Orthopedic nursing is a nursing specialty focused on the prevention and treatment of musculoskeletal disorders. Orthopaedic issues range from acute problems such as fractures or hospitalization for joint replacement to chronic systemic disorders such as loss of bone density or lupus erythematosus.
Or
Nursing applied to the orthopedic patient is called orthopedic nursing. Orthopedic nursing also deals with trauma, injury, deformity, fracture, and disable patient.
Or
Purpose of orthopedic nursing:
1. To correct deformity.
2. To control and relieve pain.
3. To increase muscle strength and joint function.
4. Correction of the appearance.
5. Save the patient life.
6. To reduce useless limb.
7. To reduce infection like-septicemia, gas gangrene, fat imbolism, tetanus etc.
8. Reduction of injury and illness related to musculoskeletal system.
9. To reduce invalidation.
[Reference: John Ebnezar’s, “Textbook of Orthopedics”, ed-4th,P-6]

Define orthopedic nurse:
The orthopaedic nurse is a member of a team, whose efforts are directed towards the restoration or improvement of the function of the body in disease, injury or deformity at any part of the locomotor system. The team is lead by the orthopaedic surgeon, whose orders govern every stage of the treatment.
Or
A nurse whose primary area of interest, competence, and professional practice is the branch of nursing concerned with the prevention and correction of disorders of the locomotor system, including the skeleton, muscles, joints, and related tissues.
[Trauma Manual, The Trauma and Acute Care Surgery, Ed-3rd; P-3]
Role of a nurse in an orthotrauma patient:
1. She needs to assist the doctors in carrying out the treatment effectively.
2. She needs to take care of the patient in all his functional activities.
3. She needs to function as a effective link between the doctors and patient and their relatives in clearing up any communication hurdle.
4. She gets an opportunity to treat patient as a whole, while a doctors ends up usually treating a case.
[Reference-BT Basvanthappa, P-5]
Or
1. Direct care provider:
Orthopedic nurse is a qualified nurse by vitue of experience or specialized training responsible to provide direct patient care to the traumatic and orthopedic patients admitted to the orthopedic ward. She uses sound scientific knowledge in using nursing process while delivering nursing care to the patient .A orthopedic nurse is also responsible to maintain the record and reports, which are used in the unit. provides round the clock care and continuity while other health professissonal visit the patient.
2. Promote comfort:
A ortho nurse provide comfort to the patient by immobilize the joint and prevent further complication. She also provide eye care, mouth care, wound care to promote comfort to the patient.
3. Promote mobility:
A Orthopedic nurse promote mobility to the patient by;
- Give knowledge about exercise.
- Arrange exercise training programe.
- Encourage the patients ROM Exercise
- Avoid weight bearing activity on the affected part
4. Promote self care activities:
A Orthopedic nurse is responsible for care and prevent complications to the patient. She also educate the patient about self care such as:
- Changing position.
- Maintanance of personal hygiene.
- Wound dressing.
- Importance of immobilization of joint.
- Importance of Calcium diet.
5. Advocate:
It means active support of an important cause. The role of the advocate is to assert the patient s choices or desires. There are three models of advocacy, which can be applied in nursing practice. These are right protection model, value based model and respect for person model.
Importance of Calcium diet.
6. Researcher:
As orthopedic nursing care emerges more and more as a clinical specialty that cut across age group, encompasses many disease conditions and interfaces with other variety of health care disciplines it is necessary to to explore the knowledge developement by carrying out research. The greater extent of nursing practice being based on research, the higher will be the quality of practice and patient outcomes Nurses need to value and use nursing research if nursing nursing has to have strong research based practice rather bthan a weak ritual based practice.
7. Nurse as manager:
The importance of leadership in the role of the nurse manager is essential to effective health care delivery. The essential leadership skills required of a nurse in the are creation of a vision, the building of trust and maintenance of motivation, facilitating of change and creation of work environment which is conductive to patients welfare and staff learning.
8. Increase self-esteem, self-efficacy and self concept.
9. Prevent complication:
As orthopedic nurse prevent complication to the patient by providing wound care, regular monitoring of the wound, provide asceptic technique durind care and rational use of antibiotic to the patient.
10. Restore function of musculoskeletal system:
The prevention of illness and injury in the care of individual of all ages with degenerative, traumatic, inflammatory, neuromuscular, congenital, metabolic, and oncology disorders of the musculoskeletal system.
11. Newer agent:
developing and implementing a plan of care including set goals that are unique to the individual are ongoing basis.
12. Client educator:
An orthopedic nurse educates the client during the time of admission and discharge.She educates the patient on how will they continue their care and prevent complications. She also provides current orthopedic knowledge through formal and non-formal education.
13. As a care coordinator:
An Orthopedic nurse is one member of the team involved in the care of traumatic and injured patients. The nurse provides round-the-clock care and continuity while other health professionals visit the patient. By virtue of this she becomes the co-coordinator of patient care activities.
Common orthopedic problem in Bangladesh:
(A) Traumatic orthopedic problem:
1 ) Trauma to the bone. E.g.: Fracture.
2) Trauma to the soft structure. E.g.: Dislocation, Sublaxation.
3) Trauma to the tendon, and ligaments. E.g.: Strains, sprains.
4) Occupational injuries:
a) Back problem.
b) Carpal tunnel syndrome or tendinitis.
c) Degenerative joint disease.
d) Hearing impairment
e) Stress fracture.
5) Common trauma disorder:
a) Upper Extremity Disorder
i. Tenditis
ii. Lateral epicondylitis or tennus elbow
iii. Medial epicondylitis or golfer’s elbow
iv. Rotator cuff tendinitis
b) Back and Neck Disorders
i. Low back pain
ii. Tension neck syndrome
iii. Thoracic outlet syndrome
iv. Lumber intervertebral disc syndrome
c) Lower Extremity Disorde
i. Achillers tendonitis
ii. Knee bursitis
(B) Non-traumatic orthopedic problem:
1. Inflammatory joint disease:
- Rheumatoid arthritis.
- Ankylosing spondylitis.
- Reiters arthritis.
- Psoriate arthritis.
- Juvenile arthritis
2. Infection:
- Osteomyolitis.
- Septic arthritis.
- Tropical ulcer
- Tubercular arthritis
3. Connective tissue disease:
- SLE
- Polyarthritic nodosa.
- Poly myositis
4. Crystal deposition:
- Gout
- Chondrocalcinosis
5. Disorder of bone:
- Osteoarthritis
- Osteomalacia
- Osteoporosis
6. Other orthopedic problem:
- Pain
- Deformity
- Discomfort
- Dysfunction
- Self care deficit due to immobilization.
- Complication due to immobilization.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4th edition, P-50]

Qualities of a orthopedic nurse:
1. A knowledge about the skeleton anatomy.
2. General nursing knowledge about bed making, dressing, etc.
3. A knowledge about first aid.
4. A knowledge about general orthopedic treatment like splint, sling, plaster, traction, etc.
5. A knowledge about treatment method individual fractures.
6. Most importantly a truck load of human qualities.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4th edition, Forward BT Basavanthappa, p-7]
Six important factors influence orthopedic nursing care: They are:
1. Standards of practice.
2. Philosophy of rehabilitation.
3. Ageing
4. Nutrition
5. Health teaching
6. Interrelation between the musculoskeletal system and the rest of the body
[Lippincot Adult orthopedic Nursing, page 2]
Trauma:
Trauma is the study of medical problems associated with medical injury. The injury is the adverse of a physical force upon a person. There are a variety of forces that can lead to injury, including thermal, ionizing radiation and chemical.
Or
[Ref-Bailey & Love’s, “Short Practice of Surgery”, 25th edition, Page-271)]
Trauma is a Greek word meaning ‘wound or injury’. Trauma refers to a serious or critically bodily injury, wound or shock.
Trauma nursing:
Trauma nursing is a subspecially in emergency nursing, which encompasses all aspects of nursing care for the injured or those at risk for injury.
Definition of traumatology:
The term traumatology derived from Greek word ‘Trauma” meaning wound or injury. So it is a study of wounds and injury, caused by accidental or violence to a person and need emergency treatment.
Or
Traumatology is the branch of surgery which deals with trauma patients and theirs injury.
Or
Trauma is mechanical damage to the body caused by an external force. The trauma patient has been defined as “an injured person who requires timely diagnosis and treatment of actual or potential injuries by a multidisciplinary team of health care professionals, supported by the appropriate resources, to diminish or eliminate the risk of death or permanent disability.” This chapter describes the current impact of injury on society, the structure of modern trauma systems, and finally the way injuries are measured and quantified
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Definition of trauma patient:
The trauma patient has been defined as “an injured person who requires timely diagnosis and treatment of actual or potential injuries by a multidisciplinary team of health care professionals, supported by the appropriate resources, to diminish or eliminate the risk of death or permanent disability”.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Trauma Patient Classification System :
Class A:
Unstable patient: requires immediate surgical intervention; no further injury evaluation (e.g., x- ray or laboratory studies) required.
Immediate access to the operating room is necessary.
Initiate massive transfusion protocol for blood and blood products (e.g., fresh frozen plasma, platelets).
Class B:
Unstable patient: high probability of surgical intervention within 15-30 min. Some injury evaluation in progress.
Massive transfusion likely.
Class C:
Stable patient: probability of surgical intervention within 2 h. Complete injury evaluation (e.g., CT scan) in progress.
Crossmatched blood or type and screen sufficient.
Class D:
Stable patient: minimal probability of surgical intervention (minor injuries).
Definition of trauma team:
The trauma team is an organized group of professionals who perform initial assessment and resuscitation of critically injured patients. Team composition, level of response, and responsibilities of each member are institution-specific.
The epidemiology of trauma :
A.
Overall, trauma is the third leading cause of death in the United States and is the leading source of mortality for patients between 1 and 44 years of age. In 2003, 164,002 people died secondary to injury, representing 56 deaths per 100,000 population. Of these, 109,277 were unintentional in nature while
49,639 were caused by violence. A fatal injury occurs approximately every 5 minutes.
B.
Mortality after trauma can be characterized by a well-studied distribution that identifies three time periods during which the majority of deaths occur. Approximately 50% of deaths occur immediately and are usually secondary to > severe neurologic injuries or exsanguination from major blood vessel injuries (Fig. 1-1). These deaths can be avoided only through injury prevention.
The second peak of approximately 30% of all deaths occurs during the initial hours postin-jury and preventing these deaths is the goal of modern trauma care, such as is taught through the Advanced Trauma Life Support (ATLS) course. Finally, 20% of deaths occur late (within 1-2 weeks) and are secondary to sepsis and multiple organ failure. It is believed that improved early management of injury and associated shock may prevent these late complications.
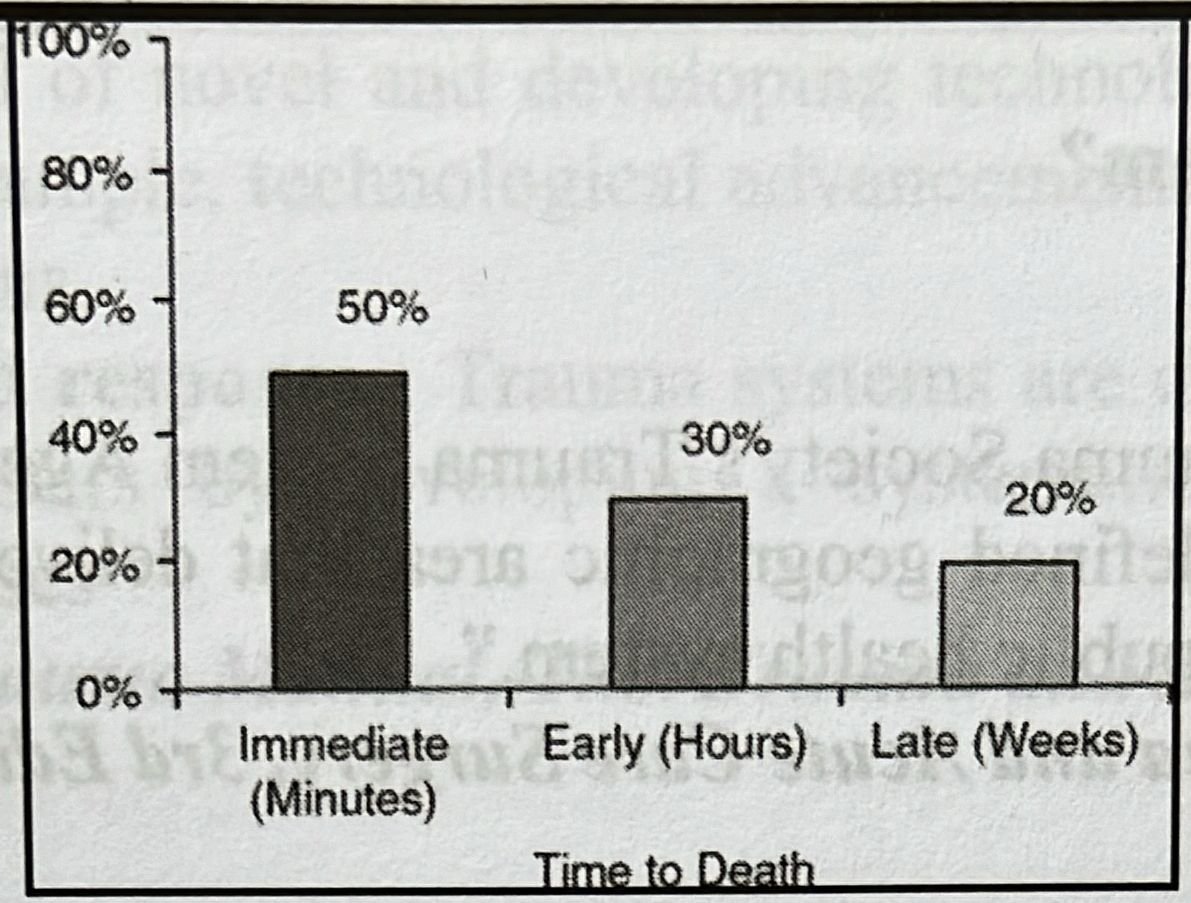
Figure 1-1. Distribution of death after injury. (Adapted from Trunkey DD. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, more expedient surgery and further research. Sci Am 1983; 249:28.)
C.
In 2003, more than 29 million medically attended, nonfatal injuries occurred in the United States. Data from 2002 reveal an estimated 37.8 million injury-related emergency department and 99.2 million office- based visits. There were approximately 1.8 million hospital discharges for injured patients. Injury represents the greatest cause of years of potential life lost (YPLL) before age 65 totaling over 3.4 million years or 29.3% of all YPLL. The total cost for injuries occurring in 2003 including medical expenses, lost wages, property damage, cost to employers, fire losses, and all other costs was estimated to be $607.7 billion.
D.
Specific injury patterns and mechanism
- Age: While people 44 years old and younger account for the majority of fatal and non-fatal injuries, the impact of trauma on the elderly is far more severe. The death rate for injuries among patients 0 to 44 years old is approximately 45 per 100,000 population, whereas this rate is 113 per 100,000 foropen people over 65 years old and 169 per 100,000 for people over 75 years old.
- Gender: Sixty-nine percent of all injury-related deaths occur in males, twice the number of female deaths. The distribution of nonfatal injuries is more equivalent with males representing 55%.
- Mechanism:
- Motor vehicle crashes (MVCs) are the leading cause of injury-related death, accounting for 44,800deaths in 2003 or 15.4 deaths per 100,000 population. Over 3.5 million people sustained nonfatalinjuries secondary to MVC in 2003. Despite this, the death rate per vehicle miles traveled (VMT) has declined steadily throughout the century from 18 deaths per 100 million VMT in 1925 to approximately 5 per 100 million VMT in 1960 to as low as 1.56 per 100 million VMT in 2003. In the 2005 National Trauma Data Bank (NTDB), MVCs accounted for 43.1% of cases and 46% of the mortalities. MVC-related deaths occurred in 4.9% of NTDB cases.
- Firearm-related injury resulted in 28,827 deaths in 2003 and was the second leading cause ofinjury-related mortality for all ages in that year. Fifty-nine percent were the result of suicide, while 41% were homicide related. Nonfatal gunshot wounds were identified in 65,834 patients in 2003. Predominately, fatal shootings involve young males, with the number of deaths in the 15-to-34- year-old age range being over seven times that of females. Handguns were involved in 80% of all homicides with a firearm in 2003. Six percent of the injuries in the NTDB were associated with firearms; 16% of cases resulted in death. Firearm-related injuries peaked at 19 years of age.
- Falls are the leading cause of nonfatal injury resulting in approximately 8.1 million injuries and 17,229 deaths throughout all age groups. Falls are most common among the young and the elderly with both groups demonstrating injury rates of greater than 4,000 injuries per 100,000 population in 2003, twice that of people in the intermediate age groups. Despite this similarity, falls are the matal leading cause of death in patients 65 years or older while death in children is uncommon. The death rate due to falls in elderly patients is more than 170 times that of children less than 10 years old. Falls in the NTDB accounted for 26% of all cases, with an associated mortality of 3.5%. The peak incidence occurred at age 82.
- Other common mechanisms contributing to trauma mortality include poisoning, suffocation, drowning, cutting/piercing, and burns. Common non-fatal injuries include struck by/against injury, overexertion, and bites/stings.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Trauma system:
As defined by the American Trauma Society’s Trauma System Agenda for the Future, “A trauma system is an organized, coordinated effort in a defined geographic area that delivers the full range of care to all injured patients and is integrated with the local public health system.”
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Fundamental components of trauma system :
1. Injury prevention has become an essential focus for all trauma systems in order to proactively reduce the impact of injury. Many systems have developed formal injury prevention programs and dedicated centers to better address this need.
2. Pre-hospital care includes community access and communication systems as well as EMS systems and triage protocols. Universal access to emergency care (i.e., 911) is essential to allow efficient activation of the system. A robust communication system provides for coordination of pre-hospital resources as well as proper transfer of information to receiving facilities. Standardized curricula for training EMS personnel provide a more consistent knowledge base and skills set. Developed trauma systems have ensured more efficient emergency response through improved geographical placement of EMS providers versus only facility-based responders.
3. Acute care facilities provide a range of injury management from initial stabilization and transfer to all- inclusive definitive care. Based on available resources, facilities are characterized by injury management capabilities and many are designated as trauma centers using a scale of 1 to 4, with Level 1 centers providing the most comprehensive level of care. Successful trauma systems benefit from the contributions of all available facilities to become more inclusive and to provide consistent care to all people within the system.
4. Post-hospital care is an important part of reducing disability and improving an injured patient’s long- term outcome. Efficient transfer from the acute care setting to rehabilitation is a necessary attribute of a well-developed trauma system.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 31]
Trauma system infrastructure elements:
1. Leadership: A lead agency should be established to coordinate trauma system development and provide necessary administration.
2. Professional resources: Successful trauma systems rely on competent and energetic health careproviders to ensure optimal injury care. Recruiting methods to identify and employ the highest qualityhealth care professionals is a necessity. habi
3. Education/Advocacy: Trauma systems must improve public awareness about trauma as a disease state of injury prevention to reduce the societal impact of trauma. nostalot and the ability
4. Information management: Trauma data registries at the local and national levels provide an invaluable resource for performance improvement, research, and trauma system management. Ideally, trauma data should be consistently captured and incorporated into regional and national databases to provide the mostaccurate depiction of the status of injury care.
5. Finances: Adequate financial support is essential for both trauma system development and the continued provision of trauma care. Increased public and political awareness of the magnitude of theproblem is required to improve governmental funding.
6. Research: To continue improving the care of the injured, research endeavors must be encouraged and efforts to increase financial support for trauma research is crucial.
7. Technology: The potential of novel and developing technologies must be adopted and applied to the field of trauma care. For example, technological advancements have decreased EMS response times and improved crash investigations.
8. Disaster preparedness and response: Trauma systems are charged with the task of being prepared to respond to potential disasters by developing a systematic and organized approach that can be Tata implemented if the need arises
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Trauma system:
Injury scoring systems have been developed to accurately and consistently quantify the magnitude of injury from an anatomic, physiologic, or a combined standpoint. Scoring systems are used in triage decision making, quality improvement and benchmarking initiatives, prevention program analyses, and research endeavors.
Injury scoring systems used for triage decision making must be easy to calculate from rapidly available information. Scoring is commonly used in the research setting and in this case should be able to identify patients with comparable injuries.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Principles of injury scoring:
1. Purpose: Injury scoring systems have been developed to accurately and consistently quantify the magnitude Stream of injury from an anatomic, physiologic, or a combined standpoint. Scoring systems are used in triage decision making, quality improvement and benchmarking initiatives, prevention program analyses, and research endeavors.
2. Database use: Scoring systems are commonly included in trauma databases to provide a quantifiable means of patient comparison. Based on the purpose of the database, certain scoring systems may be more baan appropriate and relevant than others. For example, administrative databases would more appropriately contain International Classification of Diseases (ICD-9) based scoring systems (e.g., ICD-based Injury Severity Score [ICISS]) while trauma registry databases may contain Abbreviated Injury Score (AIS) based total scoring systems. Identification of the specific needs of the database often reveals the type of scoring system that would be most applicable.
3. Correct use of scoring: While there are many available scoring systems, the use of some of these systems may be limited. Systems used for triage decision making must be easy to calculate from rapidly available information. Scoring is commonly used in the research setting and in this case should be able to identify patients with comparable injuries. Evaluation of responses to therapy may benefit from applying a physiologic scoring system. The combined scores are valuable when assessing outcome after injury.
4. Limitations: Since every injured patient is unique, there is no single scoring system that can provide a perfect description. Care must be taken when interpreting the results of injury severity scoring to recognize that there will always be aspects of the patient’s condition that were not captured.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 2]
Assessment level of severity of injury of a patient:
1. Anatomic scores:
- Abbreviated Injury Score (AIS). First proposed in 1969 and updated last in 1990, the AIS assigns a severity level to the worst injury in each of six separate body regions: head/neck, face, thorax,abdomen/pelvic contents, bony pelvis/extremities, and external structures. Level of severity ranges from 1 (minimally injured) to 6 (fatal). The AIS does not account for multiple injuries in the same patient.
- Injury Severity Score (ISS). ISS was first introduced in 1974 to more accurately characterize severity when multiple injuries were present. ISS is calculated by squaring the AIS scores from the three most severely injured body regions and adding the results. If any AIS is 6, the ISS is automatically 75 and considered to be a fatal injury. ISS is commonly used for injury quantification, although it is limited in that its accuracy requires that all injuries be identified before calculation and it is unable to account for multiple injuries within the same body region.
- The 2005 NTDB categorized injuries based on ISS as minor (ISS 1-9), moderate (ISS 10- 15), severe (ISS 16-24), and very severe (ISS >24). Minor injuries constituted about two thirds (68%) of the injuries with the remainder being nearly equal among the other groups. The average hospital length of stay increased by approximately 3 days for each severity grouping while intensive care unit (ICU) days also increased (moderate = 1.7 days, severe = 3.9 days, very severe =7.7 days).
- New Injury Severity Score (NISS). In an attempt to improve on the shortcomings of ISS, NISS was developed in 1997. NISS is calculated similarly to ISS, but the three most severe injuries, regardless of body region, are used in the equation. As a result, NISS is more straightforward to calculate and has been shown to be more predictive of survival than ISS.
- American Association for the Surgery of Trauma (AAST) Organ Injury Scale (OIS). In 1987 the AAST organized the OIS committee to create an injury scoring system that accurately quantifies the severity of individual organ injuries for clinical investigation and outcomes research purposes. Scales were created from critical review of available literature as well as expert trauma surgeon consensus. Injuries to organs are graded from 1 to 5 to reflect severity and anticipated impact on outcome. Injury scales for abdominal organs spleen, liver, kidney, pancreas, duodenum, small bowel, colon, and
rectum have been provided (Appendix A). - Survival Risk Ratios (SRR)/ICD-based Injury Severity Score (ICISS). Recently, ICD-9 diagnostic codes have been employed to quantify injury severity. Using large trauma databases, SRRs are calculated by determining the mortality observed for each injury-related ICD-9 code. All SRRs for a given patient are then combined to yield ICISS. Because reimbursement depends on ICD-9 codes, the information needed to calculate ICISS is readily available in any hospital data repository. Despite its simplicity, ICISS has been found to be a better predictor of mortality than either ISS or the Trauma and Injury Severity Score (TRISS).
- Anatomic Profile (AP). The AP incorporates injuries from three body regions: head/spine, anterior neck and chest, and all other injuries. Scores for these regions are modified and used in an equation derived from logistic regression. The AP has recently been shown to demonstrate good injury model predictiveness compared to other scoring systems.
TABLE 1-1 Glasgow Coma Scale
Eye opening
Spontaneous 4
To voice3
To pain2
None 1
Verbal response
Oriented 5
Confused 4
Inappropriate 3
Incomprehensible 2
None 1
Motor response
Obeys commands6
Localizes pain5
Withdraws to pain4
Flexion 3
Extension 2
None 1
Total Glasgow Coma 3-15
Score
- Penetrating Abdominal Trauma Index (PATI). PATI is a scoring system designed to quantify the effects of penetrating abdominal injury. Each organ has a pre-determined risk factor score (1 to 5) and injured organs are assigned a severity score (1 to 5) based on published criteria. The severity score is multiplied by the risk factor score and the sum of all of these results is the PATI.
Physiologic scores
- Glasgow Coma Score (GCS). The GCS is the most widely used scoring system for the characterization of neurologic injury. A patient’s status in terms of eye opening, verbal response, and motor activity is determined and summed to calculate the GCS (Table 1-1). A patient’s GCS can be rapidly calculated in the field or in the emergency department and is commonly used for patient care decision-making and triage.
- A GCS of 8 or less is usually indicative of severe brain injury and suggestive of required intervention (e.g., intubation).
- The motor component of the GCS has been found to correlate well with the entire GCS and be the most predictive of outcome.
- Trauma Score (TS). The TS was developed in 1981 to incorporate physiologic parameters in severity scoring. Quantification of respiratory effort, systolic blood pressure, capillary refill, and GCS are included in the determination of the TS. Use of the TS has been limited by the subjective nature of respiratory effort and capillary refill assessments.
- Revised Trauma Score (RTS). The RTS addressed the deficiencies of the TS by removing the ambiguous respiratory and perfusion components. As Table 1-2 demonstrates, coded values are assigned to quantify the GCS, systolic blood pressure, and respiratory rate parameters. The result is a score of 0 to 12 with 12 demonstrating normal physiology. Therefore, the RTS is simple to calculate and is used in making triage decisions and predicting hospital outcomes.
- Systemic Inflammatory Response Syndrome Score (SIRS Score). The SIRS score incorporates patient temperature, heart rate, respiratory rate, and white blood cell count to physiologically characterize injured patients
TABLE 1-2 Revised Trauma Score
| A Glasgow Coma Score | B Systolic blood pressure (mmHg) | C Respiratory rate (breaths/min) | Coded value (CV) |
| 13-15 | >89 | 10-29 | 4 |
| 9-12 | 76-89 | >29 | 3 |
| 6-8 | 50-75 | 6-9 | 2 |
| 4-5 | 1-49 | 1-5 | 1 |
| 0 | 0 | 0 | 0 |
(Table 1-3). The SIRS score can be calculated easily and has been demonstrated to be predictive of outcome on admission and further into a patient’s hospital course.
Combined scores
- Trauma and Injury Severity Score (TRISS). Introduced in 1983, TRISS combines anatomic and physiologic parameters to arrive at a calculated probability of survival. TRISS incorporates the ISS, RTS, patient age, and injury mechanism into an equation that uses established coefficients determined using large trauma databases. TRISS is valuable in outcomes analyses and research but has no value in the patient care setting.
- A Severity Characterization of Trauma (ASCOT). ASCOT uses a methodology similar to TRISS but has been adapted to better characterize situations where the predictive ability of TRISS is deficient (e.g., penetrating torso injury). ASCOT uses the RTS, patient age, and an anatomic description similar to the AP. ASCOT also employs a logistic regression model to determine survival probabilities. The results of ASCOT assessments have been minimally more predictive than TRISS methodology.
- Harborview Assessment for Risk of Mortality (HARM). First published in 2000, HARM combines 80 variables such as ICD-9 codes, age, injury mechanism, comorbidities, and injury associations to predict survival probabilities.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 2]
Definition of blunt trauma:
A usually serious injury caused by a blunt object or collision with a blunt surface (as in a vehicle accident or fall from a building) the patient died of blunt trauma to the head called also blunt force trauma
Or
A usually serious injury caused by a blunt object or surface died of blunt trauma to the head.
Possible Associated Injuries related to blunt trauma:
| Documented injury | Possible associated injuries |
| 1. Neck injury (cervical fracture) | 1. Carotid artery injury |
| 2. Sternal or first/second rib fracture | 2. Thoracic aortic injury, myocardial contusion, atrial rupture |
| 3. Scapula fracture | 3. Pulmonary contusion, thoracic aortic injury |
| 4. Chest wall injury (rib fractures 6-12) | 4. Left side splenic injury, right side hepatic injury |
| 5. Lumbar fracture (L2-L3) | 5. Pancreatic contusion/transaction, intestinal rupture |
| 6. Abdominal wall abrasion/ contusion (“seatbelt”sign) | 6. Intestinal rupture, mesenteric rent |
| 7. Severe pelvic fracture | 7. Bladder rupture, urethral transection, rectal/vaginal injury |
| 8. Shoulder dislocation (anterior) | 8. Axillary nerve injury |
| 9. Knee dislocation (posterior), supracondylar femur fracture | 9. Popliteal artery injury (intimal tear/thrombosis) |
| 10. Bilateral calcaneal fractures | 10. Lower extremity and vertebral fractures, renal/thoracic aortic injuries |
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 11]
Possible Associated Injuries related to penetrating trauma:
Penetrating Trauma: Documented and Possible Associated Injuries
| Documented injury | Possible associated injuries |
| Cervical (platysma penetration) injuries | Jugular esophageal injury vein/carotid |
| Transmediastinal injury | Cardiac/tracheobronchial and pulmonary/vascular/ diaphragmatic/gastrointestinal injury |
| Thoracoabdominal injury | Pulmonary/diaphragmatic/cardiac/gastrointestinal injury |
| Transabdominal injury | Gastrointestinal/hepatic/vascular injury |
| Transpelvic injury | Bladder/intestinal/uterine/vascular injury |
| Flank injury | Genitourinary/intestinal injury |
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 12]
Types of blunt trauma :
1. Motor vehicle crashes.
2. Motorcycle crashes.
3. Pedestrian-automobile impacts.
4. Falls.
5. Assaults.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
Motor Vehicle Crashes (MVCS):
A. Injuries are produced by the rapid decrease in velocity over a short distance (deceleration). Severity of injury depends on energy transferred during deceleration as a result of a crash.
- MVCs account for over half of the deaths from unintentional causes.
- MVCs cause at least half of closed head and spinal cord injuries.
- The risk of a major injury increases 300% to 500% if the victim is ejected (including a 1 in 13 risk of spinal column injury).
- MVCs involve three types of collisions:
- Primary collision-motor vehicle impacts another object
- Secondary collision-victim strikes internal components of the car
- Deceleration-induced deformation results in differential movement of fixed and nonfixed anatomic parts (e.g., shearing injury to the brain or transection of the thoracic aorta)
B. Determinants of injury:
- Magnitude of force (force = mass × acceleration)
- Location of victim (front seat versus back seat; driver versus passenger) yell
- Restraint devices (Table 2-3)
- Injury risk is greatest in the unrestrained victims.
- Lap belts alone decrease mortality by 50% (there is, however, an increased rate of abdominal injury).
- The lap belt is designed to fit across the pelvis (the anterior superior iliac spines). If inappropriately worn over the abdomen, compression fractures of the lumbar spine (Chance fractures) can occur. Lap belt injuries are associated with small bowel and coloninjuries. Such injuries also include mesenteric tears and thrombosis of the abdominal aorta.
- Three-point constraints plus airbags provide the optimal protection, especially in front-end collisions.
- Secondary collisions of occupant with the vehicle are reduced with the utilization of three- point restraints. Ejection is prevented and mortality is substantially decreased.
- With three-point constraints, extremity injuries are not prevented. Also, there is no effect on major injury patterns with side impact collisions.
- Shoulder belt should not be worn without the lap component; the driver and passengers can slip under this restraint.
- Shoulder belt injuries are associated with multiple vascular injuries, including intimal damage or thrombosis of innominate, subclavian, carotid, or vertebral arteries.
Restraint Devices
A. Lap belt
B. Shoulder belt
C. Shoulder and lap belts
D. Airbags (frontal and side impact)
Airbags allow a less traumatic deceleration when compared to three-point restraints. The proportion and severity of lower extremity injuries are increased relative to torso and head injuries. However, airbags can cause injuries to occupants who are facing backward or leaning against the steering wheel or into another passenger’s compartment.
- cranial injuries (16%)
- facial fractures (37%)
- cervical spine injuries (10-15%)
- major thoracic injuries (46%)
- abdominal injuries (5-10%)
- femur fractures (65%)
- distal lower extremity fractures (33%)
- forearm fractures (46%)
- A lateral crash can result in direct impact between the vehicle and the occupant because of the limited space between the driver and the colliding vehicle.
- Because there is very little substantive material to blunt such an impact, lateral impact collisions are associated with twice the mortality of frontal impacts.
- Thoracic and abdominal injuries are most prevalent.
- The occupant is projected into the next compartment.
Rear-end impact collisions
- Rear-end impact collisions do not usually cause severe injuries, with only 8% of crashes resulting in serious injury.
- An extension flexion injury (“whiplash”) is common.
Rollover collisions
- Because of the random nature of these collisions, force vectors vary.
- Kinetic energy of the car is usually dissipated over a long distance. Roof collapse can produce severe head injury.
- Axial load forces can result in compression fractures of the spine.
- Ejection of the occupant can occur.
Unrestrained (backseat passenger)
The rear seat passengers have the same risk of injury as those in the front seat except the direct injuries sustained from the steering wheel and dashboard impact.
Rear seat passengers are less likely to be restrained.
Unrestrained rear seat passengers can be a projectile, potentially causing injury to both themselves and occupants in the front seat
** Short note: III. Motorcycle Crashes
- Unlike motor vehicle crashes, the driver or passenger usually absorbs all the impact and the associated kinetic energy.
- The majority (75%) of motorcycle deaths are a result of cranial injuries.
- Spine, pelvis, and extremity injuries are also common.
- Less obvious fractures can occur.
- There is a high risk of limb loss with open or severe injuries to the tibia and fibula
** Short note: Pedestrian-Automobile Impacts
Although pedestrian-automobile impacts account for only 2% of traffic injuries, they account for 13% of traffic-related deaths. Children, the elderly, and the intoxicated, are more at risk for this mechanism of injury. The pattern of injury is depicted in Fig. 2-1. Torso trauma (chest, abdomen, and pelvis) represents 6% of the injuries; however, musculoskeletal and intraabdominal are more common (35% and 27%, respectively).
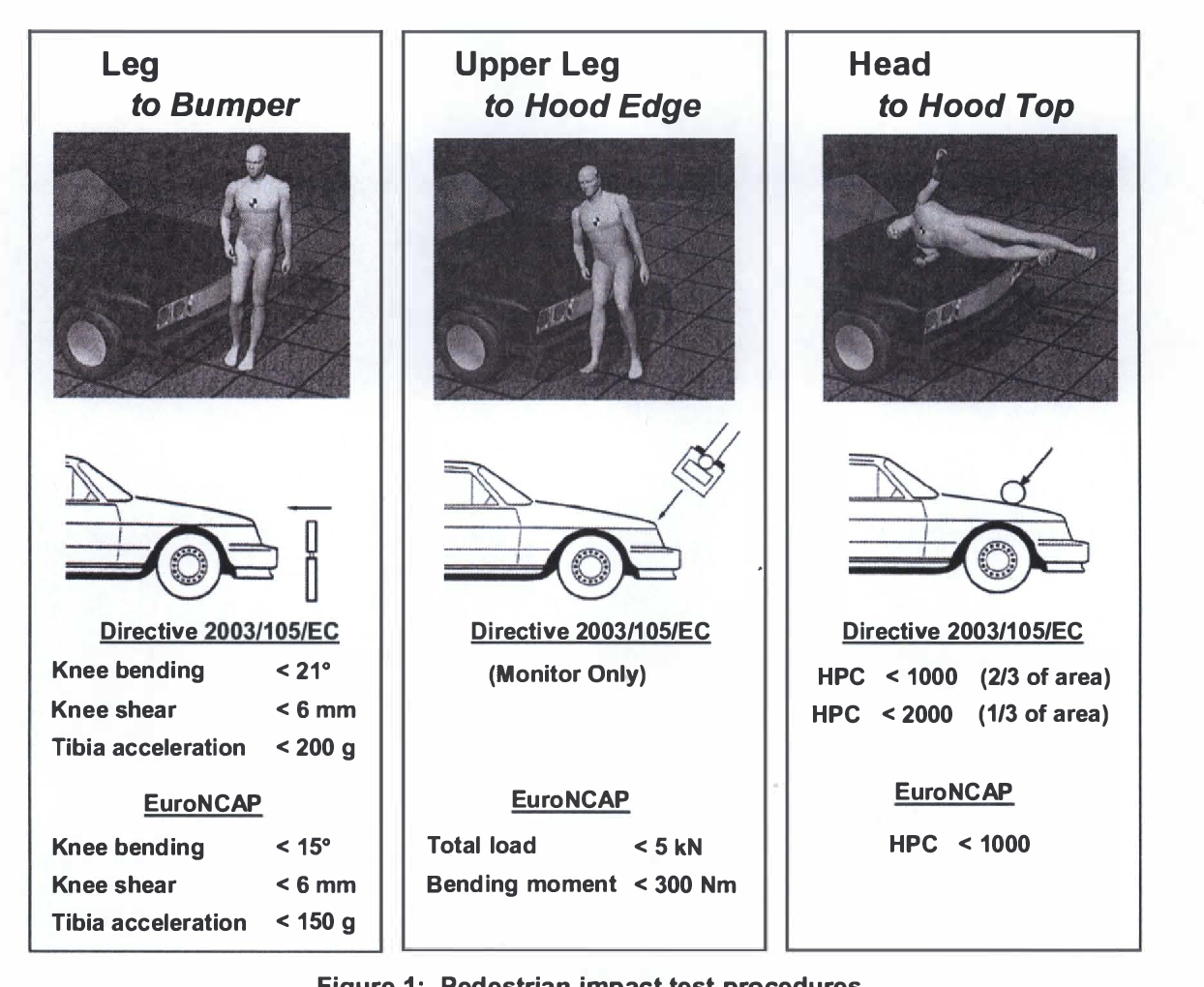
Figure 2-1. Pedestrian-automobile impact. (Baylor College of Medicine 1986. Modified from Feliciano DV, Moore EE, Mattox KL, eds. Trauma. 3rd ed. Norwalk, Conn: Appleton and Lange, Englewood Cliffs, NJ; 1996:97, with permission.)
- This type of impact often results in Waddle’s triad of injury: (1) tibiofibular or femur fracture, (2) truncal injury, and (3) craniofacial injury. Therefore, a patient with two components of Waddle’s triad of injury should be assumed to have the third component as well.
- In general, small children tend to be “run over” and adults “run under” or thrown over the car with impact onto the street.
- A lateral compression pelvic fracture can occur as a result of contact between the hip and the fender of the motor vehicle.
** Short note: Falls
- Injuries sustained in falls depend on distance of fall, surface struck, and the position on impact.
- Energy at impact is the product of the victim’s weight times distance of fall times gravitational forces.
- Kinetic energy is dissipated, on impact, throughout the skeleton and soft tissues. • Duration of impact (i.e., how quickly the victim stops) is critical in determining injury severity.
- Impact force over a shorter time increases the magnitude of injury.
- Harder surfaces increase severity of injury because of immediate deceleration and transfer of all energy to the body (e.g., concrete vs. grass, sand, or snow).
Fall injuries are frequent in the elderly. Comorbidities are major determinants of outcome and can also contribute to causing the fall. - Femoral neck fractures and head and cervical spine injuries can result from the elderly falling while walking.
- Falls occurring from a height can involve a tumbling mechanism or a “free fall.” Free falls imply a fall from a height directly to the ground.
- Falls of 25 to 30 feet (three stories) have a mortality of 50%. Survival is rare in free falls from above five stories.
- Injury patterns differ depending on how the victim lands. If the victim lands on his or her feet, from a height above 10 to 15 feet, the pattern of injuries
- could include calcaneal, lower extremity, pelvis, and spine fractures. Thoracic aorta and renal injuries can also occur.
- Falls with a horizontal orientation result in greater energy dissipation and fewer injuries. This is a less predictable injury pattern and includes craniofacial trauma, hand and wrist fractures, along with abdominal and thoracic visceral injuries. (fisticuffs, kicking, stomping, striking with an object)
- Young males are the most commonly injured by this mechanism, with injury patterns being variable (depending on the weapon, position of the person being assaulted, and the magnitude and intensity of the attack).
- Head and facial injuries are more common (72%).
- Defensive posturing of the victim usually results in lower extremity injuries (<10%).
- Severe torso injuries (including pancreatic and hollow viscus injuries) can occur from a stomping or kicking injury.
- An intoxicated assault victim with a depressed level of consciousness has an intracranial injury until proven otherwise.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 4]

Physiologic Responses to the trauma patient:
A. Altered mental status Belligerence, anxiety, immobilization, withdrawal, and antagonism are commonly seen after major trauma. It is important to be aware that this can signify severe hypovolemia, hypoxemia, or both.
B. Altered vital signs Fever may be seen after fluid resuscitation, which can be caused by the sustained inflammatory response. It is critical to be vigilant for infectious causes.
C. Blood pressure may not become significantly decreased until the patient has lost 30% to 40% of circulating blood volume. Therefore, blood pressure correlates poorly with either blood volume or flow.
D. Tachycardia can persist even after fluid resuscitation and pain is adequately controlled.
E. Increased minute ventilation secondary to both tachypnea and increased tidal volume is common.
F. Generalized edema is common secondary to increased total body salt and water within the interstitium. This is a result of increased sympathetic vasoconstriction, altered capillary permeability, and hypoproteinemia. Also, local inflammation at the wound site leads to edema formation secondary to the release of locally acting chemokines.
G. Increased cardiac output Heart rate and contractility increase with injury. However, with hypovolemia, preload may be decreased to a degree that significantly lowers cardiac output.
H. Hypermetabolism Energy demands, oxygen consumption, and carbon dioxide production are all elevated following trauma.
I. Altered protein, glucose, and fat metabolism Energy requirements are increased following injury, with the magnitude of the additional energy need dependent on the severity of injury, magnitude of tissue destruction, and lean body mass of the patient.
- Protein loss is approximately 300 to 500 grams per day (g/day) of lean body mass, with visceral proteins spared at the expense of skeletal muscle proteins.
- Proteins are broken down to constituent amino acids that are catabolized to ammonia (forms urea) and precursors of the tricarboxylic cycle (TCA).
- Carbohydrates provide 4 kilocalories per gram (kcal/g) when oxidized. Muscle glycogen (storageform of glucose) is used only by skeletal muscle (i.e., not released systemically), whereas hepatic glycogen provides glucose for glucose-dependent tissues (brain, leukocytes).
- Gluconeogenesis can occur from amino acids, glycerol, lactate, or pyruvate via TCA or Krebs’ cycle.
- Lipids, which are used by tissues that are not glucose dependent, are the largest source of energy (9.4 kcal/g) in the body. Lipids are catabolized to form ketone bodies in the liver along with CO₂ and energy from glycerol and fatty acids.
J. Leukocytosis Elevation in the white blood cell count can be seen after injury.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 7]
Trauma Management:
A. Airway management:
- Patient assessment. The airway is assessed by simultaneous evaluation of several simple clinical features. These include level of consciousness, physical findings, and vital signs.
- Level of consciousness. The patient’s general condition of wakefulness is the best predictor of the ability to protect the airway from aspiration or occlusion. Specific simple features are commonly sought using the AVPU scale: Is the patient awake, eyes open, and conversing? Is the patient reacting to verbal stimuli? Is the patient arousable only to painful or noxious stimuli? Is the patient unresponsive? Abnormalities of mental status can be caused by hypoventilation, hypoxemia, hypoperfusion, drug or alcohol intoxication, or head injury. If the patient’s ability to maintain adequate oxygenation, ventilation, or airway patency is impaired, airway interventions are required.
- Physical findings. Search for findings indicative of poor oxygen delivery to tissues: pale, cool, moist skin; delayed capillary refill (>2 seconds); noisy or labored respirations (too fast or too slow). Other physical findings more specific to a pure respiratory abnormality include asymmetric or shallow chest excursion, crepitus, thoracic ecchymosis, nasal flaring, accessory muscle use, abdominal breathing, or subcostal retraction. from
- Vital signs. Abnormal vital signs (including pulse oximetry) must be addressed and appropriate therapy instituted. Normal vital signs do not guarantee adequate ventilation or airway protection.
- Airway resuscitation encompasses positioning and clearing the airway, delivering supplemental oxygen, using adjuncts or assist devices, and implementing tracheal intubation techniques.
- Positioning the airway. Manual techniques for opening the airway include the head tilt/chin lift, jaw thrust, and jaw lift. Each acts to manually displace oropharyngeal soft tissues and the tongue away from the posterior portion of the throat, allowing upper airway patency. In the trauma patient, presence of a cervical spine injury must almost always be suspected; therefore, the head tilt/chin lift is contraindicated in most trauma patients,aside from those with isolated extremity injuries.
The jaw thrust is accomplished by placing two hands at the angles of the mandible and lifting the jaw forward. The jaw lift is performed by placing a thumb inside the mouth on the mandibular incisors and fingers under the tip of the chin. The jaw and its attached soft tissues are then lifted forward. Semiconscious or combative patients may bite rescuers, precluding use of the jaw lift. Otherwise, when performed with cervical spine immobilization, jaw thrust and lift offer low risk and good yield for patients requiring assistance in band maintaining airway patency. These maneuvers are also adjuncts for more advanced interventions, including assisted ventilation and tracheal intubation.
- Supplemental oxygen. To maximize alveolar oxygen concentration, supplemental oxygen should be administered to all trauma patients. This can be accomplished by numerous devices. The high- flow devices, including the partial and nonrebreather masks, are best for delivering oxygen to the conscious, alert trauma patient. The fraction of inspired oxygen (FiO2) delivery by nasal cannula is variable and limited by blood or secretions in the nares. For this reason, nasal cannula oxygen had supplementation should not be used in place of high-flow mask devices.
- Airway adjuncts are devices or maneuvers that aid in maintaining airway patency.
- Suctioning. The clearing of secretions, mucus, blood, debris, or vomi-tus is essential to establishing airway patency. Dentures, loose teeth, bone fragments, and other foreign material must be removed. Suctioning is performed with a plastic, rigid, large-opening device (e.g., a Yankauer or tonsil tip catheter) to allow rapid removal of materials without clogging of the device. Handheld pump-action devices or large-caliber suction tubing without a tip can also be used to clear the airway of debris. Care must be taken to avoid inducing or exacerbating oropharyngeal bleeding when using any suction device. Small- bore devices are not recommended for use in trauma patients.
- Nasopharyngeal airway is a device to maintain airway patency in the semiconscious or unconscious patient. Nasal airways must be used in conjunction with manual positioning of the airway (jaw thrust or lift). The size of the patient’s little finger can help guide choice of a nasal airway, and the most patent nostril should be used for insertion. The device is an uncuffed, pliable rubber tube with a beveled tip and a funnel-shaped top (hence the common nickname “nasal trumpet”). The device is inserted into the nose, and extends from the nostril to the nasopharynx, coming to rest behind the base of the tongue. Advantages of the nasopharyngeal airway are ease of insertion; aid in maintaining airway patency behind the tongue; ability for repeated suctioning without intense oropharyngeal stimulation; and usefulness in patients with a gag reflex or clenched teeth whereoropharyngeal airways cannot be used. Disadvantages include inability to isolate the trachea, and obstruction by blood or secretions.
- Oropharyngeal airway is a rigid, plastic, semicircular-shaped device with side ports that facilitate suctioning. It is used only in unconscious patients who lack a gag reflex. Oropharyngeal airways must be used in conjunction with manual positioning of the airway. The device is placed into the mouth following the curvature of the tongue (while holding the tongue with a gauze pad or using a wooden depressor) with the tip resting behind the base of the tongue. Alternatively, the airway can be inserted with the open curve of the “C” facing cephalad or lateral, with the tip then rotated to match the natural tongue curve after placement. With either placement method, pushing the tongue posteriorly will occlude the airway. The size of the oropharyngeal airway is chosen based on the distance from the lip angle to the ear lobe. In addition to maintaining or restoring airway patency, the advantages of an oropharyngeal airway include ease of suctioning and assistance of ventilation. Disadvantages are stimulation of the gag reflex in the semiconscious patient, inability to place the device in patients with clenched teeth, and inability to isolate or protect the trachea.
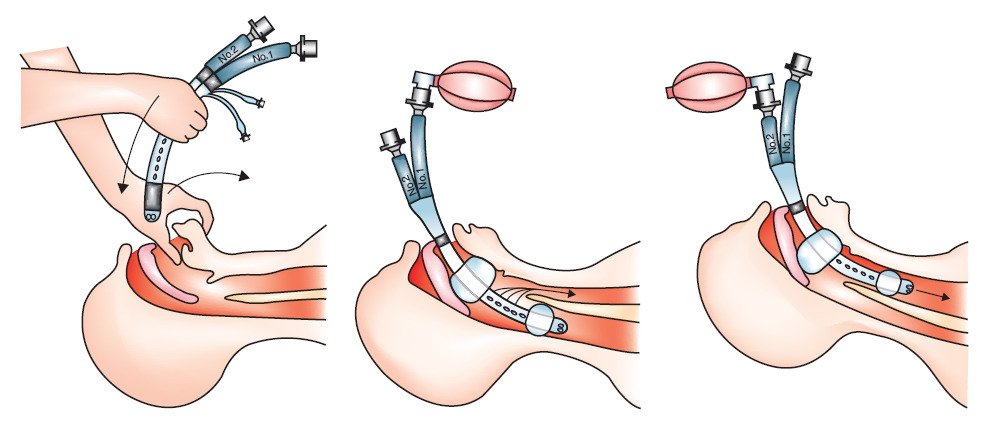
- Esophagotracheal Combitube (ETC) (Fig. 6-1)
- The ETC is placed through the mouth without direct hypopharyn-geal or glottic visualization. Normally, the tip resides in the upper esophagus and hypopharynx. After inflating the balloon to obstruct the flow of gases to the esophagus, the esophageal port is ventilated. Gas exits from holes above the esophageal cuff or balloon and is directed the short distance toward the glottis, resulting in near normal tidal volumes delivered to the lungs, with attendant breath sounds and expired CO2
- Approximately 10% to 15% of insertion attempts result in the glottis being entered rather than the upper esophagus; resultant ventilation of the esophageal port yields lack of chest excursion or breath sounds. This must be recognized; in this situation, the second port should be ventilated. Similar to a standard endotracheal tube, this should provide direct oxygen to the trachea and produce symmetric breath sounds, CO₂ on exhalation, and a quiet epigastrium. Little neck manipulation is needed with the blind insertion. The major disadvantages include lack of tracheal isolation in most cases, and the need to identify the cases in which the glottis is entered (to allow ventilation through the correct port).
- Laryngeal mask airway (LMA) (Fig. 6-2) The LMA is a pliable, sili-cone teardrop-shaped diaphragm with an inflatable, cuffed rim and a proximal ventilation tube. The diaphragm is placed through the oropharynx and rests above the glottis, with its tip in the esophagus. The diaphragm acts to isolate the posteriorly located esophageal structures from the anterior laryngeal opening. The proximal port is ventilated using a bag-valve device. Advantages of the LMA include rapidity and ease of placement, high success rates with rvo not training, andmaintenance of inline cervical positioning during insertion. Its ability to prevent aspiration is controversial, particularly in patients with high airway pressures (e.g., asthma). Disadvantages include initial training requirements, little data on its use outside the operative suite or hospital, the requirement of an unconscious patient, and the necessity of “sizing” the device
- Sellick’s maneuver. Gentle manual pressure is placed on the cricoid cartilage, with the intent of occluding the esophagus that lies directly behind it. When correctly performed, cricoid pressure helps limit the risk of aspiration by impeding gastric insufflation and the movement of vomited material into the hypopharynx and glottis. It also can aid intubation by moving anterior laryngeal structures into view during laryngoscopy (e.g., backward, upward, rightward pressure, or BURP). Care must be exercised as aggressive pressure can transmit forces to the underlying cervical spine. Otherwise, this maneuver offers little risk and great potential benefit. One common mistake is to put pressure on the thyroid cartilage rather than the cricoid cartilage, which does not alter the risk of aspiration and can tilt the glottis out of view during laryngoscopy. Cricoid pressure is maintained until proper endotracheal tube position is confirmed.
- Advanced airway skills in the field
- All advanced airway techniques, from direct oral intubation to surgical airways, require a significant investment in training, equipment, and continuing education (to maintain competency). Each skill can be performed by physicians, paramedics, and nurses after proper training and with specific guidelines. However, it is not at all clear under what circumstances these techniques should be used, particularly in the nonarrest patient. Chapter 11 discusses general trauma airway issues; here, we highlight those specific to the prehospital setting.
- Endotracheal intubation. (Chapter 11 also discusses this topic.) Orotracheal intubation is the method of choice for most apneic patients, with nasotracheal intubation an alternative bobose al itu method in certain spontaneously breathing patients with clenched teeth or inability to open their mouths. In the field, the success rate of nasal intubation is lower than with oral intubation. Recent data strongly suggest that field intubation assisted by sedative and paralytic drugs (“rapid-sequence intubation”) is associated with worse outcomes in patients with serious head trauma than is noninvasive management with bag-valve-mask 1,00 techniques. No cause-effect relationship has been established, and optimal ventilation
strategies for these patients remain unknown. - Digital intubation may be useful when limited access to the patient or inability to directly visualize the airway structures exist. In the field, limited suction capabilities make this an attractive option for advanced providers. Digital intubation requires an unconscious patient and a “bite-block” (or other protective device) to prevent injury to the provider’s fingers. The long finger of the nondominant hand is “walked” to the base of the tongue until a with the long finger and elevating the epiglottis with the index finger, the endotracheal tube is guided blindly between the fingers into the glottic opening. Digital intubation has the advantage of being possible in cases where injury or foreign material limits direct visualization of the glottis. However, the technique requires dexterity, has risk of harming the provider, and causes uncertain motion of the cervical spine. There have been no organized studies of the efficacy or effectiveness of this technique.
- Transillumination (lighted stylet) intubation. Newly developed intubation devices take advantage of fiberoptic technology to aid in tracheal intubation. A bright light introduced into the larynx will transmit through the anterior neck soft tissues to allow the operator to visualize correct stylet positioning and subsequent endotracheal intubation.
- Percutaneous translaryngeal catheter (jet) insufflation may be useful in either failed oral or nasal intubation or in those patients with incomplete upper airway obstruction unrelieved with standard maneuvers. The relevant techniques are discussed in Chapter 11.
- Cricothyroidotomy. Paramedics, flight nurses, and other providers can perform cricothyroidotomy for patients after failed intubation or with anatomic distortion that precludes other methods of gaining airway control. Several case studies regarding field use have been published. The techniques are discussed in Chapter 11.
- Assist devices. Prehospital personnel provide ventilatory assistance using multiple methods.
- Bag-valve devices. The bag-valve is an oblong, self-inflating rubber bag with two one-way valves. The bag has a standard (15 mm) connection that can attach to a face mask or endotracheal tube for ventilation. When used with room air, delivered FiO2 is 21%. High- flow oxygen at 12 to 15 liters per minute (L/min) provided by a supplemental oxygen inlet with a reservoir bag can deliver up to 90% to 95% oxygen. The bag-valve-mask device can be used to assist spontaneous respirations or to ventilate apneic patients.
- Demand valve devices. The demand valve (manually triggered oxygen-powered breathing device) delivers 100% oxygen at high flow rates (40-60 L/min). A push-button valve allows oxygen to flow to the patient. Advantages include ease of use and high concentration of delivered oxygen. Disadvantages include lung barotrauma, inabilityto assess lung compliance, gastric distention, and inability to use in pediatric patients. Because of these disadvantages, demand valve use is discouraged.
- Automatic ventilators are time-cycled, constant-flow, gas-powered devices. These are small and portable, and usually have two controls-one for ventilatory rate and one for tidal volume. A standard (15 mm) adapter allows use with an endotracheal tube. While designed primarily for use in prolonged interfacility transports, some EMS systems use them in the prehospital setting.
- Field confirmation of tracheal tube placement. Confirmation of proper endotracheal intubation is accomplished by multiple methods no single method is infallible
- Physical assessment includes visualization of the vocal cords and trachea during intubation and auscultation of bilateral breath sounds in the anterior and axillary lung fields with lack of ventilatory sounds over the stomach (epigastrium). These are the first and easiest confirmatory methods for many patients, but are not definitive. Additional objective confirmation is needed.
- End-tidal carbon dioxide detectors (ETCO₂) electronic and colorimet-ric devices are placed between the endotracheal tube and the ventilation device. These detect end-expiratory CO₂, with levels of 2% or greater indicating endotracheal placement. Semiquantitative CO2, detectors may not be accurate in low pulmonary perfusion states such as cardiac arrest, massive pulmonary emboli, severe shock, or cardiac tamponade. Outside these situations, however, expired CO₂ is very useful to confirm correct tube location. All EMS systems should utilize ETCO₂ detection, and any endotracheal tube placed in the field should be assessed using an ETCO₂ device.
- Bulb and suction devices, often referred to as esophageal detection devices, can be placed over the end of the endotracheal tube, creating negative expiratory pressure. These devices can be useful when ETCO, is unavailable or when it is negative, yet the provider believes the tube is properly placed in a patient with a low- or no-flow state that may limit or prevent delivery of CO₂ to the lungs. In general, these devices should not be the first-line confirmation device.
- Pulse oximetry (oxygen saturation monitoring) is an adjunct to assess respiratory adequacy; however, arterial desaturation can be a late finding in respiratory failure. This, coupled with notechnical difficulties with sensing in the field, particularly with a hypotensive patient, limits the utility of pulse oximetry in rapid confirmation of tracheal tube placement, although it is valuable in identifying adequate arterial oxygenation.
B. Other procedures and therapies:
- Intravenous access and fluid therapy
- Intravenous (IV) access allows the administration of crystalloids, blood products, and medications. yarn Venous catheterization of trauma patients by paramedics is done routinely, even though outcome data supporting this practice are lacking. Currently, pragmatism suggests that IV access should be attempted while not delaying transport or other interventions (especially airway management and No vidusop hemorrhage control). To limit the on-scene interval, attempts at IV placement should be made live Haim during extrication, while awaiting transport resources, or during transport to the hospital. Two large-bore (≥16 gauge) peripheral IV lines are preferred for major trauma patients.
- Failures. A number of trauma patients will arrive at the hospital without IV access because of short TRAM et blu transport times, uncooperative patients, or other more pressing priorities (e.g., airway management, spine protection, or hemorrhage control).
- Fluid therapy in the field. Significant controversy exists regarding the composition, amount, and ultimate clinical goals of fluid therapy in trauma patients. Specific heart rate or blood pressure targets to guide the amount of fluid are poorly understood. The issue does not appear to center on a “fluids: yes or no” question; rather, controlled or limited fluid resuscitation (sometimes referred to as “permissive hypotension”) appears beneficial, although the endpoint and fluid makeup are still uncertain.
- Military antishock trousers (MAST)
- Background. MAST, also referred to as the pneumatic antishock garment (PASG), have been in Sattelte use by civilian EMS providers for many years. Their use grew out of the experiences during the Vietnam War and documented clinical effects on blood pressure in the hypotensive trauma patient. ostzilammi However, little positive outcome data (especially with respect to mortality or morbidity) are available to support MAST use, and they have generally fallen out of favor.
- MAST inflation. The major effect is to increase peripheral vascular resistance, accomplished by decreasing the perfusion of the capillary beds of the lower extremities by the external pressure provided via the inflated MAST. This may increase blood flow to more vital organs. MAST may water help stabilize pelvic and femur fractures and limit blood loss.
- Indications. The following are current recommendations from the National Association of EMS Physicians (NAEMSP) regarding the use of MAST in trauma, using the American Heart ad Association’s Emergency Cardiac Care “class” system:
Class Ila. Acceptable, uncertain efficacy, weight of evidence favors usefulness and efficacy
- Hypotension due to suspected pelvic fracture.
- Severe traumatic hypotension (palpable pulse, blood pressure not obtainable)
Class IIb. Acceptable, uncertain efficacy, may be helpful, probably not harmful.
- Penetrating abdominal injury.
- Pelvic fracture without hypotension.
- Spinal shock.
Class III. Inappropriate option, not indicated, may be harmful.
- Diaphragmatic rupture.
- Penetrating thoracic injury.
- To splint fractures of the lower extremity.
- Extremity trauma.
- Abdominal evisceration.
Application and removal
- Remove any objects on the patient’s lower body that might cause the MAST or the patient to be punctured. The MAST are slid under the patient and the three sections secured atcond circumferentially. (Often, the MAST are laid on the long spine board before placing the patient on it.) The leg sections are inflated first, using a foot pump. Inflation continues until the Velcro crackles or the MAST pressure gauge reads 100 mmHg.
The abdominal section is then inflated in a similar manner. The patient’s respiratory efforts should be observed closely because inflation of the abdominal section can limit pulmonary reserve. Large-bore suction should be available in case the patient vomits.
- Deflating the MAST prematurely or rapidly can lead to hypotension that may not respond to reinflation of the MAST. As much as possible, the patient must be adequately volume resuscitated and/or have bleeding controlled before the device is removed. The abdominal section should be deflated first, in a slow and deliberate manner. A small quantity of air is released and the patient’s blood pressure is checked. If a fall of 5 to 10 mmHg occurs in the systolic blood pressure, deflation is halted. If no decrease in blood pressure ensues, deflation can proceed. Once the abdominal section is deflated, the leg sections are deflated, one at a time, in a similar fashion. Under no circumstances should the MAST be nog cut off a patient. This is both risky and renders the MAST unusable.
Complications. The most common complication of MAST use is interference with the physical boolfacexamination or gaining groin vascular access. Other complications include
- Shock after inappropriate removal
- Compartment syndrome
- Lactic acidosis
- Myoglobinuria
- Ventilatory compromise
- Hyperkalemia
- Increased cerebral edema
Needle thoracostomy
- Indications. Needle thoracostomy should be performed when a tension pneumothorax exists or is tylitthon a suspected. Any trauma patient with severe respiratory distress should be evaluated immediately for tension pneumothorax. In the field, the diagnosis is critical and must be treated before arrival at the hospital. Tension pneumothorax should be suspected in the trauma patient who is short of breath or hypotensive and with any of the following features:
- Decreased breath sounds
- Tracheal deviation (away from the involved side)
- Distended neck veins (this may not be seen in the patient who is hypovolemic) Hyperresonance to percussion of the chest (on the involved side) difficult to assess in the field environment.
- If the patient is intubated, increasing difficulty in bag-valve ventilation can be the earliest or sole indication of a developing tension pneumothorax.
Respiratory distress
- Procedure. Treatment should proceed rapidly once the diagnosis is suspected; if incorrect, the only Foldanarda harm is creating the need for a formal tube thoracostomy in the receiving facility, whereas failing to recognize and treat can lead to death. Decompress the affected side of the chest by inserting a large-bore IV catheter (12 or 14 gauge) perpendicular to the skin at the second or third intercostal space in the midclavicular line, or the third or fourth interspace in the anterior axillary line. Advance the catheter until a rush of air occurs from the open distal end, or until the hub reaches the skin. Common errors include placing the needle either too close to the sternum or cephalad to the second intercostal space (making heart or great vessel puncture possible), or placing the needle under instead of over a rib (making puncture of the neurovascular bundle, which runs in a groove under each rib, possible). After placement, withdraw the needle, but leave the catheter in place to prevent reaccumulation of pleural gas. If the patient’s condition worsens, suspect occlusion of the first catheter and place a second needle (Fig. 6-3).
- Bilateral decompression. Occasionally, especially in the patient on positive pressure ventilation or with severe obstructive lung disease, bilateral tension pneumothorax can develop. The asymmetry described above with respect to tracheal and chest findings may not be present. If uncertain, both hemithoraces should be decompressed.
- Therapy after needle thoracostomy. At the receiving facility, a chest tube is usually placed for alderive orde definitive treatment once needle decompression is performed (whether or not clinical success wav occurred with the latter). Once the chest tube is in place, the catheter(s) can be withdrawn.
Splinting
- Indications. The purposes of splinting are to prevent further injury, decrease blood loss, and limit the amount of pain the patient will have with movement of that extremity during extrication and noeyevin transport. An injured extremity should be splinted in anatomic position if possible, with the splint extending to the joints above and below the fracture site for stabilization. If the patient refuses, or if resistance to straightening exists, splint in a position of comfort. Dressings should be applied to any open wounds before splinting.
- Splint types. A large variety of splint designs will appear on patients brought to the emergency department. They can be as simple as a rolled-up newspaper, or as complex as a vacuum or traction splint:
- Cardboard splints, with or without foam padding, are intended for single use.
- Board splints, which are common and durable, are made of straight pieces of wood, metal, plastic cut to various lengths.
- Air splints, which encircle the injured extremity, are inflated with air to impart stiffness. They are usually clear to allow visualization of the underlying structures. Overinflation can cause neurovascular compromise.
- Vacuum splints incompletely encircle the injured limb. Instead of air being blown intothem, air is withdrawn and a vacuum is produced, which stiffens the splint. Traction splints are used for femur fractures.
- Thomas half-ring splints and Hare traction splints are those most commonly used. Specific training is required for proper placement.
- Ladder splints are made from heavy gauge wire in a ladder shape. They are useful for splinting extremities that cannot be straightened because they are bendable and can be shaped to match the extremity. The SAM Splint, with a flexible aluminum alloy core covered with closed-cell foam, is similarly flexible.
- Complications. Although splinting is safe and effective in most patients, complications can develop, including:
- Neurovascular compromise. Whichever splint is used, distal neurovas-cular status must be checked before and after application of the splint. Also, if any patient movement has occurred, the patient reports more pain, or the extremity is noted to be cyanotic or edematous distal to the splint, reexamine the extremity and splint. It is also advisable to periodically check the neurovascular status, even if none of the above occur. When impaired neurovascular status is seen distal to an injury, the splint should be loosened or adjusted, and the neurovascular status rechecked.
- Pain. When the patient reports pain, search for neurovascular compromise or malpositioning. Gentle repositioning should resolve this condition.
Axial spine immobilization
- Prehospital indications. Historically, despite the lack of supporting literature, the entire axial spine is immobilized by prehospital personnel whenever the mechanism of injury, injury pattern, or physical examination indicate the possibility of any spinal injury. Most major trauma patients have
experienced kinematic forces that warrant the precautionary application of spinal immobilization devices until definitive clinical and/or radiographic examinations can be performed in the ED. Patients with obvious physical findings (e.g., bony crepitation, palpable step-offs) or those with neurologic findings (e.g., paresthesia, weakness, paralysis) consistent with spine or cord injury should always receive complete immobilization before transport - Clinical assessment of the spine often cannot be performed by field personnel because of time, space, distracting injury, altered consciousness, and other concerns (e.g., airway, bleeding control, vascular access) that can preclude adequate in-field evaluation to rule out spinal injury. While the rule in prehospital care is to maintain a high index of suspicion for such injuries with liberal application of spinal immobilization, it is well established that field personnel, with proper training and medical oversight, can safely assess which patients do and do not require spine immobilization. The protocols that EMS systems use for this purpose generally exclude major trauma patients from consideration for this assessment, requiring full spine immobilizing.
- The need for spinal immobilization occurs at the injury scene and continues through extrication, transportation, and stabilization in the ED. Immobilization is accomplished with the least possible neck movement, and ends only when physical and/or radiographic findings definitively rule out injury.
- Types of immobilization devices. No single method or combinations of methods of immobilization consistently place the spine in neutral position or prevent all motion in the axial spine.
Cervical collars (c-collars) are numerous in design and efficacy. These rigid one or two- piece devices encircle the cervical spine and soft tissues of the neck, providing (when properly fitted) a snug fit between the tip the chin and the suprasternal notch of the anterior chest, and between the occiput and the suprascapular region of the back. These collars limit movement of the head in the coronal and transverse planes, minimizing lateral and rotary motion. They do not, however, provide adequate immobilization in the sagittal plane (flexion-extension motion). For this reason, a rigid cervical collar
alone is inadequate for effective spinal immobilization and is always used in conjunction disin with a cervical immobilization device (CID) and a spine board (short or long). Soft neck collars (foam supports covered with loose-weave material) are ineffective at limiting motion of the head in all planes, and are not intended for use in spinal immobilization.
CIDs are made of plastic, cardboard, or foam. They act to pad the lateral aspects of the head (limiting both lateral and rotary motion), and possess restraining straps that are positioned over the patient’s forehead and chin, encircling the back of a short or long spine board. The CID affixes the patient’s head and c-collar to a rigid spine board, limiting the head movements of flexion and extension. A CID can be fashioned from blanket rolls, blocks, or sandbags placed alongside the head, with fixation to the spine board via wide (2- to 3-inch) silk tape placed over the forehead and chin.
Spine boards are termed “short” or “long,” depending on the most distal portion of the patient immobilized. Short boards limit flexion and extension from the head to the hips, minimizing movement in all portions of the spine (cervical, thoracic, lumbar). Short boards are primarily used if patient access is limited (e.g., entrapment in a vehicle, or confined space extrication) and stability in the axial spine is needed before and during the extrication process. Once extrication is performed and complete access to the patient is achieved, the short board and patient are typically secured to a long spine board.
Long spine boards limit flexion and extension from the head to the feet. Straps provide fixation points at the thorax, hips, and lower extremities (above the knees). Data suggest that including the lower extremities in the immobilization process aids in stabilizing the lumbosacral spine and limits lateral motion of the torso if lateral tilting of the board is needed to manage emesis. Padding between the lower extremities and under the knees pizad diew animalite enhances both stabilization and patient comfort.
Secondary pain after immobilization. With any of these devices, immobilization itself can produce symptoms of discomfort (e.g., occipital headache; neck, back, head, mandible pain). This should not preclude the liberal application of spinal immobilization devices in most patients with significant trauma. Padding behind the occiput and in the areas of lordosis and kyphosis make intuitive sense, and may be especially important in the pediatric and elderly population, given their anatomy.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 7]
Traumatic Arrest :
The term “traumatic arrest” refers to the end result of a variety of pathologic processes in response to injury and is not a single clinical entity.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 6]
Management of traumatic arrest :
At the scene. Time on scene (excluding extrication) should typically be <10 minutes.
Ensure scene safety before entry, particularly in cases involving assaults, fire, hazardous materials, confined spaces, and vehicular traffic. Law enforcement or fire service assistance may be needed to secure the scene prior to EMS operations. Field personnel should not put themselves at risk for a patient with a negligible chance of survival.
- Recognize cardiac arrest.
- Determine whether to initiate resuscitation (see Section B).
- Assess for the presence of special conditions such as hypothermia or a primary medical cause that might influence decision or course of resuscitation.
- Maintain manual spinal immobilization.
- Open airway using jaw thrust without head tilt. Inspect oral cavity, and suction or manually remove debris (blood, teeth, etc.).
- Ventilate patient with basic techniques (e.g., bag-valve-mask) at a rate of 12 to 16 breaths/minute. Use supplemental high-flow oxygen as soon as available.
- Perform chest compressions at rate of 100/minute.
- Control severe external hemorrhage.
- Determine ECG rhythm (note that above steps may be carried out while assessing rhythm to decide whether to proceed with resuscitation):
- Defibrillate up to three times for ventricular fibrillation.
- Note the presence of an organized rhythm (pulseless electrical activity) as this confers a greater likelihood of a reversible condition.
- Attempt endotracheal intubation (refer to Chapter 11).
- If able to intubate, confirm proper tube position and carefully secure tube.
- If unable to perform intubation, determine effectiveness of ventilation using basic techniques:
If able to ventilate adequately (chest rise and fall), continue ventilation with basic maneuvers.
If unable to ventilate adequately with a mask device, and if the rescuer is properly trained and qualified, either insert an alternative airway device (e.g., Combitube or laryngeal mask airway [LMA]) or perform jet ventilation or surgical cricothyroidotomy; otherwise (as is often the case in most EMS situations), initiate rapid transport and continue to attempt ventilation with basic maneuvers.
- Assess patient for tension pneumothorax.
- Signs: unilateral (or bilateral) decreased breath sounds, poor or worsening lung compliance (especially with positive pressure ventilation), tracheal deviation, subcutaneous emphysema.
- If pneumothorax is suspected, perform needle decompression.
- Immobilize the patient’s spine on long backboard with straps, rigid cervical collar, and head immobilization device.
- Transfer the patient rapidly to the vehicle, and initiate transport.
En route to the hospital
- Ensure ongoing optimal ventilation (using means above, ensuring tube position if present).
- Reassess for tension pneumothorax.
- Contact direct medical oversight and/or receiving facility, based on local protocol.
- Initiate intravenous (IV) access, or intraosseous (IO) access if intravenous access cannot be obtained and the rescuer is qualified.
- Two large-bore IV lines (≥16 gauge) are optimal.
- The role of fluid resuscitation is controversial. A pragmatic approach is to guide EMS providers to control any external hemorrhage first, and provide isotonic crystalloid fluid to help approach normal circulating volume but not to seek “normal” vital signs until hemorrhage is controlled. In many cases, the latter cannot occur until after hospital arrival.
Advanced interventions for physicians and other advanced providers may be indicated in some situations, especially when transport time is 15 to 20 minutes, or there is prolonged entrapment:
- Surgical airway
- Cricothyroidotomy
- Translaryngeal jet ventilation
- Venous access
- Central vein access
- Cutdown of saphenous vein at groin or ankle
- Tube thoracostomy Needle decompression can produce inadequate or only temporary decompression of pneumothorax and is inadequate for drainage of hemothorax.
Termination of efforts. Termination of resuscitation efforts should be considered for traumatic arrest patients with 15 minutes of unsuccessful resuscitation efforts and cardiopulmonary resuscitation (CPR).
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 3]
