Lung cancer – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Lung cancer
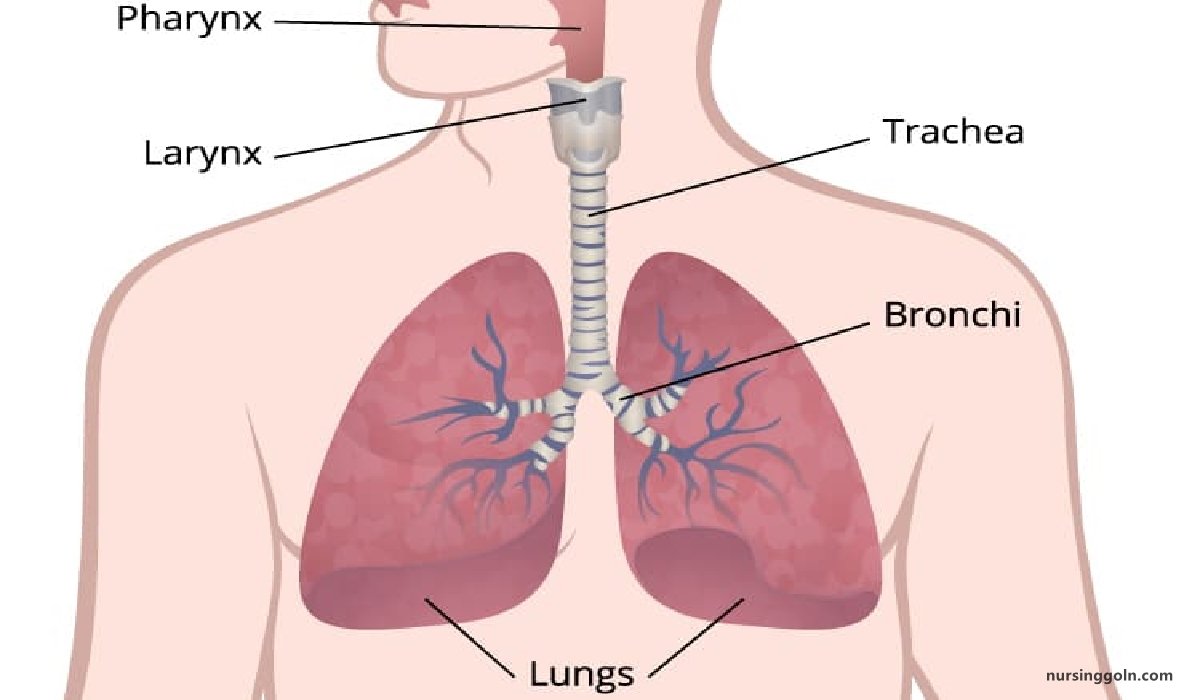
Definition of Lung Cancer:
Lung cancer is the uncontrolled growth of abnormal cells that start off in one or both lungs; usually in the cells that line the air passages. The abnormal cells do not develop into healthy lung tissue, they divide rapidly and form tumors.
Or,
Lung cancer, also known as lung carcinoma; is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung.
Clinical Feature of Lung Cancer:
Early symptoms may include:
- Lingering or worsening cough
- Coughing up phlegm or blood
- Chest pain that worsens when you breathe deeply, laugh, or cough
- Hoarseness
- Shortness of breath
- Wheezing
- Weakness and fatigue
- Loss of appetite and weight loss
As cancer spreads, additional symptoms depend on where new tumors form. For example, if in the:
- Lymph nodes: lumps, particularly in the neck or collarbone
- Bones: bone pain, particularly in the back, ribs, or hips
- Brain or spine: headache, dizziness, balance issues, or numbness in arms or legs
- Liver: yellowing of skin and eyes (jaundice)
Types of lung cancer
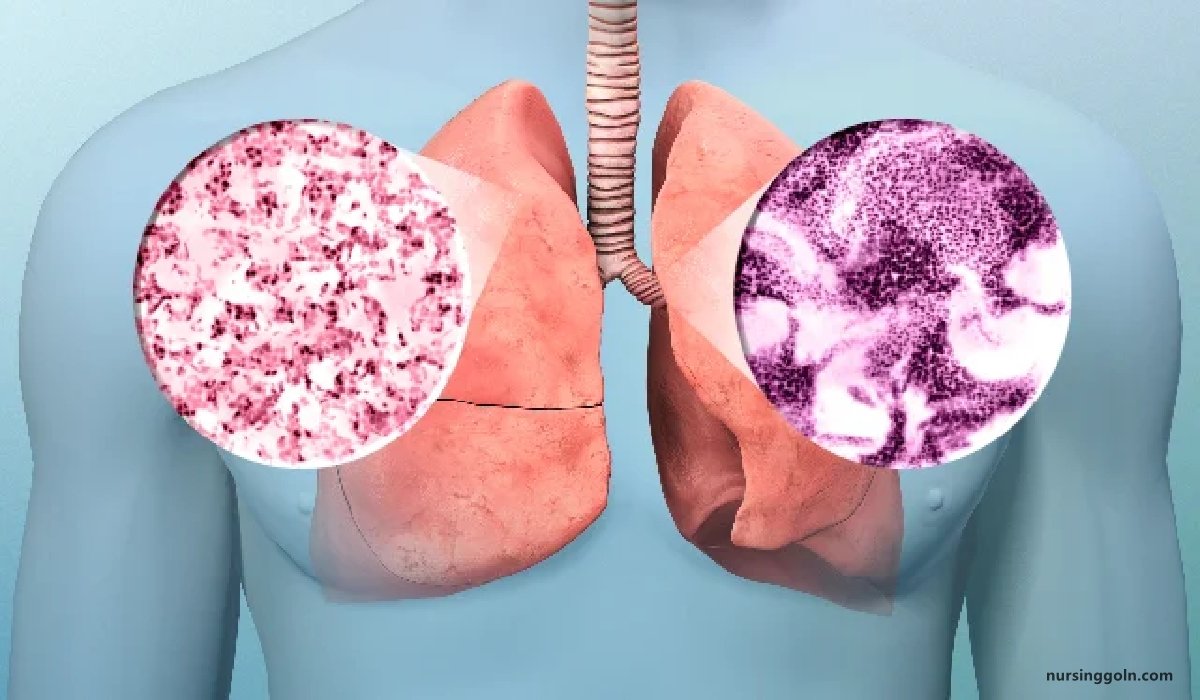
Doctors divide lung cancer into two major types based on the appearance of lung cancer cells under the microscope.
The two general types of lung cancer include:
1. Small cell lung cancer. Small cell lung cancer occurs almost exclusively in heavy smokers and is less common than non-small cell lung cancer.
2. Non-small cell lung cancer. Non-small cell lung cancer is an umbrella term for several types of lung cancers that behave in a similar way. Non-small cell lung cancers include squamous cell carcinoma, adenocarcinoma and large cell carcinoma.
Stages of Lung Cancer
Non-small cell lung cancer has four main stages:
Stage 1: Cancer is found in the lung, but it has not spread outside the lung.
Stage 2: Cancer is found in the lung and nearby lymph nodes. Stage 3: Cancer is in the lung and lymph nodes in the middle of the chest.
Stage 3A: Cancer is found in lymph nodes, but only on the same side of the chest where cancer first started growing.
Stage 3B: Cancer has spread to lymph nodes on the opposite side of the chest or to lymph nodes above the collarbone.
Stage 4: Cancer has spread to both lungs, into the area around the lungs, or to distant organs.
Small-cell lung cancer (SCLC) has two main stages. In the limited stage, cancer is found in only one lung or nearby lymph nodes on the same side of the chest.
The extensive stage means cancer has spread:
- throughout one lung
- to the opposite lung
- to lymph nodes on the opposite side
- to fluid around the lung
- to bone marrow
- to distant organs
At the time of diagnosis, 2 out of 3 people with SCLC are already in the extensive stage.
Causes of Lung Cancer:
- Cigarette smoking
- Asbestos arsenic
- Radon exposure
- Secondhand smoke
- Tuberculosis
- Air pollution
- Beryllium cadmium
- Past lung disease- COPD, TB, Chronic bronchitis, Emphysema
- Family history of lung cancer
Risk Factors of Lung Cancer:
Risk factors for lung cancer include:
1. Smoking. Risk of lung cancer increases with the number of cigarettes someone smoke each day
2. Exposure to secondhand smoke.
3. Exposure to radon gas. Radon is produced by the natural breakdown of uranium in soil, rock and water that eventually becomes part of the air you breathe. Unsafe levels of radon can accumulate in any building, including homes.
4. Exposure to asbestos and other carcinogens. Workplace exposure to asbestos and other substances known to cause cancer-such as arsenic, chromium and nickel also can increase your risk of developing lung cancer, especially if you’re a smoker.
5. Family history of lung cancer. People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Complications
Lung cancer can cause complications, such as:
- Shortness of breath.
- Coughing up blood.
- Pain.
- Fluid in the chest (pleural effusion).
- Cancer that spreads to other parts of the body (metastasis).
Treatment of Lung Cancer:
1. Surgery: About 10-30% of lung cancers can be removed surgically
2. Radiation: High energy X-ray is given if a person refuse or unfit for surgery, if the tumour has spread. Radiation is either delivered externally and internally (in sealed containers)
3. Chemotherapy: The platinum based drugs are effective.
4. Targeted therapy: Erlotinib (Tarceva) and gefitinib (Iressa) are used in lung cancer patients who are no longer responding to chemotherapy
5. Photodynamic therapy (PDT)
6. Radiofrequency ablation (RFA)
Stomach Cancer
Definition of Stomach Cancer:
Stomach cancer, also called gastric cancer, starts in the stomach. To understand stomach cancer, it helps to know about the normal structure and function of the stomach.conte
Or,
Stomach cancer, also known as gastric cancer, is a buildup of abnormal cells that form a mass in part of the stomach.
Clinical Features of Stomach Cancer:
Early symptoms of stomach cancer may include:
- A sensation of being very full during meals
- Swallowing difficulties, known as dysphagia
- Feeling bloated after meals
- Frequent burping
- Heartburn
- Indigestion that does not go away
- Stomachache, or pain in the breastbone
- Trapped wind
- Vomiting, which may contain blood
The following signs and symptoms should be seen as urgent in people at increased risk of developing stomach cancer.
- Dysphagia
- Indigestion, combined with unexpected weight loss, vomiting, or anemia, as well as fatigue and breathlessness
Risk Factors of Stomach Cancer:
1. Certain medical conditions: These include esophagitis, gastroesophageal reflux disease (GERD), peptic stomach ulcers, Barrett’s esophagus, chronic gastritis, and stomach polyps.
2. Smoking: Regular, long-term smokers have twice the risk of developing stomach cancer compared to non-smokers.
3. Helicobacter pylori infection: This bacterium is harmless for most people. However, it can cause infection and stomach ulcers in some individuals. Chronic ulcers pose some risk in the development of gastric cancer
4. Family history: Having a close relative who has or has had stomach cancer can increase the risk.
5. Consuming foods which contain aflatoxin fungus: These may be present in crude vegetable oils, cocoa beans, tree nuts, groundnuts, figs and other dried foods and spices.
6. Diet: People who regularly eat salted fish, salty foods, smoked meats, and pickled vegetables have a higher risk of developing gastric cancer.
7. Age: The risk of developing stomach cancer increases significantly after the age of 55 years.
8. Sex: Men have twice the risk of developing stomach cancer compared with women.
9. Previous or existing cancers: People who have or have had cancer of the esophagus or non-Hodgkin’s lymphoma are more likely to develop stomach cancer. Men with previous or current prostate, bladder, or testicular cancer are at higher risk, as are females with a history of cervical, ovarian, or breast cancer.
10. Some surgical procedures: Surgery to the stomach or a part of the body that affects the stomach, like the vagus nerve, can increase the risk of stomach cancer.
Causes Stomach Cancer:
- Smoking
- Being overweight or obese
- A diet high in smoked, pickled, or salty foods
- Stomach surgery for an ulcer
- Type-A blood
- Epstein-Barr virus infection
- Certain genes
- Working in coal, metal, timber, or rubber industries
- Exposure to asbestos
Stages of Stomach Cancer:
1. Stage 0: Highly abnormal precancerous cells are present in the mucosa but have not spread to other layers of the stomach or nearby lymph nodes.
2. Stage IA: The cancer has moved into one of the next layers of the stomach, such as the submucosa, but not nearby lymph nodes.
3. Stage IB: The cancer has moved into one of the next layers of the stomach and into one or two nearby lymph nodes.
4. Stage IIA: The cancer has developed into an even deeper layer, and may have spread to one or two lymph nodes. If the tumor has grown deep enough, it may not need to have spread to qualify as a stage IIA cancer.
5. Stage IIB: The tumor may not have necessarily spread as deep as a stage IIA stomach cancer but has spread to a greater number of lymph nodes, sometimes up to 15.
6. Stage IIIA: This stage sees the cancer spread to a deeper layer and up to 15 lymph nodes or start to grow through the stomach wall and spread to fewer lymph nodes. It has also started to reach nearby organs and structures.
7. Stage IIIB: The cancer has not grown as deep as a stage IIIA stomach cancer but has spread to over 16 lymph nodes. It has started to reach nearby organs and structures.
8. Stage IIIC: The cancer has either grown through most layers of the stomach and spread to over 16 lymph nodes or spread to nearby organs and structures and up to 15 lymph nodes.
9. Stage IV: The cancer has spread to distant sites. However, it may or may not have spread to nearby lymph nodes.

Diagnosis of Stomach Cancer:
More diagnostic tests will need to be done if your doctor believes that you show signs of stomach cancer. Diagnostic tests specifically look for suspected tumors and other abnormalities in the stomach and esophagus. These tests may include:
- An upper gastrointestinal endoscopy
- A biopsy
- Imaging tests, such as CT scans and x-rays
Treatment of Stomach Cancer:
1. Local therapy – removes or destroys cancer in or near the stomach
- Surgery-either partial or total gastrectomy
- Radiation-uses high energy rays to kill cancer cells
2. Systemic therapy the drug enters the bloodstream and destroys or controls cancer throughout the body
3. Chemotherapy – uses anticancer drugs
4. Complementary and alternative medicine (CAM)
5. Acupuncture
6. Massage therapy
7. Herbal products
8. Vitamins or special diets
9. Visualization
10. Meditation
11. Spiritual healing
Nursing Interventions:
1. Monitor nutritional intake and weigh patient regularly.
2. Monitor CBC and serum vitamin B12 levels to detect anemia, and monitor albumin and prealbumin levels to determine if protein supplementation is needed.
3. Provide comfort measures and administer analgesics as ordered.
4. Frequently turn the patient and encourage deep breathing to prevent pulmonary complications, to protect skin, and to promote comfort.
5. Maintain nasogastric suction to remove fluids and gas in the stomach and prevent painful distention.
6. Provide oral care to prevent dryness and ulceration.
7. Keep the patient nothing by mouth as directed to promote gastric wound healing. Administer parenteral nutrition, if ordered.
8. When nasogastric drainage has decreased and bowel sounds have returned, begin oral fluids and progress slowly.
9. Avoid giving the patient high-carbohydrate foods and fluids with meals, which may trigger dumping syndrome because of excessively rapid emptying of gastric contents.
10. Administer protein and vitamin supplements to foster wound repair and tissue building.
11. Eat small, frequent meals rather than three large meals.
12. Reduce fluids with meals, but take them between meals.
13. Stress the importance of long term vitamin B12 injections after gastrectomy to prevent surgically induced pernicious anemia.
14. Encourage follow-up visits with the health care provider and routine blood studies and other testing to detect complications or recurrence.
Preventive Measure Stomach Cancer:
Stomach cancer alone can’t be prevented. However, you can lower your risk of developing all cancers by:
- Maintaining a healthy weight
- Eating a balanced, low-fat diet
- Quitting smoking
- Exercising regularly
In some cases, doctors may even prescribe medications that can help lower the risk of stomach cancer. This is usually done for people who have other diseases that may contribute to the cancer.
You may also want to consider getting an early screening test. This test can be helpful in detecting stomach cancer. Your doctor may use one of the following screening tests to check for signs of stomach cancer:
- Physical exam
- Lab tests, such as blood and urine tests
- Imaging procedures, such as X-rays and CT scans
- Genetic tests
Definition of Oncology Nurse:
An oncology nurse is a specialized nurse who cares for cancer patients. These nurses require advanced certifications and clinical experiences in oncology further than the typical bachelorette nursing program provides.
Roles & Responsibilities of Oncology Nurse:
1. Avoid close contact with others until the treatment is completed
2. Maintain daily activities unless contra-indicated
3. Provide rest to the patient
4. Maintain a balance diet and fluid intake
5. If implant is temporary, the client should be on bed rest.
6. Excreted body fluids may be radioactive; double flash toilets after use
7. Minimize time spent in close proximity to the radiation sources
8. Maintain distance at least 6 feet
9. Use lead shields
10. Place the patient in a private room
11. Ensure proper handling and disposal of body fluids
12. Pregnant women and children are not allowed in the clients room
13. Wash marked area of the skin with plain water only and pat dry, do not wash of the treatment site marks
14. Avoid rubbing scratching or scrubbing the treatment site, do not apply extreme temperature to the treatment site
15. If shaving is necessary use electric razor
16. Wear soft loose fitting clothing over the treatment area
17. Advise the patient
- Protect skin from sun exposure during the treatment and for at least 1 year after the treatment is completed
- Maintain proper rest, diet and fluid intake
- Hair loss may occur
18. Never test vein patency with chemotherapeutic drugs
19. Monitoring client closely for anaphylactic reactions or serious side effects
20. Use caution when preparing administering or disposing chemotherapeutic agents.
Chemotherapy
Definition of Chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a category of cancer treatment that uses one or more anti-cancer drugs (chemotherapeutic agents) as part of a standardized chemotherapy regimen.
Chemotherapy may be given with a curative intent (which almost always involves combinations of drugs), or it may aim to prolong life or to reduce symptoms (palliative chemotherapy).
Or,
Chemotherapy is the subdivision of pharmacology that deals with drugs that can destroy invading organism without destroying the host.
Antineoplastic Agents:
Chemotherapeutic agents are also classified by chemical group, each with a different mechanism of action.
- Alkylating agents. Alters DNA structure by misreading DNA code, initiating breaks in the DNA molecule, cross-linking DNA strands
- Nitrosoureas. Similar to the alkylating agents, but they can cross the blood-brainbarrier.
- Topoisomerase I inhibitors. Induce breaks in the DNA strand by binding to enzyme topoisomerase I, preventing cells from dividing.
- Antimetabolites. Antimetabolites interfere with the biosynthesis of metabolites or nucleic acids necessary for RNA and DNA synthesis.
- Antitumor antibiotics. Interfere with DNA synthesis by binding DNA and prevent RNA synthesis.
- Mitotic spindle poisons. Arrest metaphase by inhibiting mitotic tubular formation and inhibiting DNA and protein synthesis.
- Hormonal agents. Hormonal agents bind to hormone receptor sites that alter cellular growth; blocks binding of estrogens to receptor sites, inhibit RNA synthesis; suppress aromatase of P450 system, which decreases level.
Types Chemotherapy:
1. Primary Chemotherapy: Initial cancer treatment with curative intent; used for Hodgkin’s disease, lymphoma, leukemia’s, testicular cancer.
2. Adjuvant Chemotherapy: Treatment of residual cells after surgical removal or tumor reduction (e.g. after mastectomy for breast cancer). Neoadjuvant chemotherapy shrinks large tumor for surgical removal. Both curative if tumor is removed.
3. Palliative Chemotherapy: For incurable cancer. prolongs and improves quality of life, reduces tumor size, symptoms
Side-Effects of Chemotherapy:
1. Generalized effects-
- Nausea,
- Vomiting,
- Pain,
- Sore mouth & throat,
- Anorexia,
- Change in taste and smell
2. Acute effects-occur within 30 minutes after treatment- pain at insertion site, cold feeling along the vein selected, and hypersensitivity
3. Long term effects- occur after 7 days. Affect major body organs- bone marrow, liver, kidney etc
4. Chemotherapy drugs are carcinogenic and teratogenic. Precautions should be taken to avoid any extravasation
Before The Procedure
1. Explain the importance of the procedure to the patient.
2. Provide privacy.
3. Teach the patient on how the procedure is done.
4. A number of medical tests are done before chemotherapy is started. The oncologist will determine how much the cancer has spread from the results of x rays and other imaging tests and from samples of the tumor taken during surgery.
5. Review- The chemotherapy drugs prescription which should have
- Name of anti-neoplastic agent.
- Dosage
- Route of administration
- Date and time that each agent to be administered.
- Accurately identify the client
6. Medications to be administered in conjunction with the chemotherapy e.g antiemetics, sedatives etc.
7. Assess the clients condition including
- Most recent report of blood counts including hemoglobin hematocrit, white blood cells and platelets.
- Presence of any complicating condition which could contraindicate chemotherapeutic agent administration i.e. infection, severe stomatitis, decreased deep tendon reflexes, or bleeding.
- Physical status
- Level of anxiety
- Psychological status
8. When a chemotherapy treatment takes a long time, advise the patient that he may prepare for it by wearing comfortable clothes. Bringing a book to read or a tape to listen to may help pass the time and ease the stress of receiving chemotherapy. Some patients bring a friend or family member to provide company and support during treatment.
9. Advise Sometimes, patients taking chemotherapy drugs known to cause nausea are given medications called antiemetics before chemotherapy is administered. Anti-emetic drugs help to lessen feelings of nausea. Two anti-nausea medications that may be used are Kytril and Zofran.
10. Other ways to prepare for chemotherapy and help lessen nausea are:
11. Regularly eat nutritious foods and drink lots of fluids.
12. Eat and drink normally until about two hours before chemotherapy.
13. Eat high carbohydrate, low-fat foods and avoid spicy foods.
During The Procedure
1. Prepare measures when administering chemotherapy.
2. Use gloves when handling chemotherapy drugs and excretions from clients receiving chemotherapy.
3. Wear disposable long-sleeves gowns when preparing and administering chemotherapy.
4. Use Luer-lock fittings on IV tubing used in delivering chemotherapy.
5. Observe the 10 Rights
After The Procedure
1. Dispose of all equipment used in chemotherapy preparation and administration in designated containers.
2. Dispose all chemotherapy wastes as hazardous materials.
3. Monitor client for symptoms of anaphylactic reaction Urticaria (hives), pruritus (itching), sensation of lump in the throat, shortness of breath.
4. Asses for electrolyte imbalances.
5. Teach client and family to report excessive fluid loss or gain, change in level of consciousness, increased weakness or ataxia, paresthesia, seizures, persistent, headache, muscle cramps or twitching, nausea and vomiting/diarrhea.
6. Prevent extravasation of vesicant drugs, implement measures to treat extravasation of vesicant medications if it occurs.
7. Teach the client to increase fluid intake to 2500 to 3000 ml/day unless contraindicated.
8. Assess for signs of bone marrow depression: decreased White blood Cell and Red Blood Cell, granulocyte, platelet counts.
9. Assess for signs of bleeding and infection.
10. Monitor for signs of renal insufficiency.
- Elevated urine specific gravity
- Abnormal electrolyte values
- Insufficient urine output (< 30 ml/hour)
- Elevated bp, bun, serum creatinine
Radiotherapy
Definition of Radiotherapy
Radiation therapy is a type of cancer treatment that uses beams of intense energy to kill cancer cells. Radiation therapy most often uses X-rays, but protons or other types of energy also can be used
Or,
Radiation therapy is a treatment used for cancer and, less commonly, thyroid disease, blood disorders, and noncancerous growths.
Indication of Radiotherapy:
- Brain tumours
- Head and neck tumours
- Bronchial tumours
- Oesophageal tumours
- Breast tumours
- Pancreas tumours
- Cervix uteri tumours
- Endometrial tumours
- Prostate tumours
- Bladder tumours
- Rectum tumours
- Testicular tumours
- Soft tissue Sarcoma
- Lymphoma
- Skin tumours
(FOR SAQ)
Nursing Management in Radiation Therapy:
1. Assessment: The nurse assesses the patient’s skin and oropharyngeal mucosa regularly when radiation therapy is directed to these areas, and also the nutritional status and general well- being should be assessed.
2. Symptoms: If systemic symptoms, such as weakness and fatigue, occur, the nurse explains that these symptoms are a result of the treatment and do not represent deterioration or progression of the disease.
3. Safety precautions: Safety precautions used in caring for a patient receiving brachytherapy include-
- Assigning the patient to a private room,
- Posting appropriate notices about radiation safety precautions,
- Having staff members wear dosimeter badges,
- Making sure that pregnant staff members are not assigned to the patient’s care,
- Prohibiting visits by children and pregnant visitors,
- Limiting visits from others to 30 minutes daily, and seeing that visitors maintain a 6 foot distance from the radiation source.
(FOR EQ)
Nursing Responsibilities for either External or Internal Radiation Therapy:
- Carefully assess and manage any complications, usually in collaboration with the radiation oncologist
- Assist in documenting the results of the therapy; for example, clients receiving radiation for metastases to the spine will show improved neurologic functioning as tumor size diminishes.
- Provide emotional support, relief of physical and psychologic discomfort, and opportunities to talk about fears and concerns. For some clients, radiation therapy is a last chance for cure or even just for relief of physical discomfort.
EXTERNAL RADIATION
Prior to the start of treatments, the treatment area will be specifically located by the radiation oncologist and marked with colored semi-permanent ink or tattoos. Treatment is usually given 5 days per week for 15 to 30 minutes per day over 2 to 7 weeks.
| Nursing Responsibilities |
|
| Client and Family Teaching |
|
INTERNAL RADIATION
The radiation source called an implant is placed into the affected tissue or body cavity and is sealed in tubes, containers, wires, seeds, capsules, or needles. An implant may be temporary or permanent. Internal radiation may also be ingested or injected as a solution into the bloodstream or a body cavity or be introduced into the tumor through a catheter. The radioactive substance may transmit rays outside the body or be excreted in body fluids.
| Nursing Responsibilities |
|
| Client and Family Teaching |
|
Side Effect/Complications of Radiotherapy:
| Part of body being treated | Common side effects |
| Any part |
|
| Head and neck |
|
| Chest |
|
| Abdomen |
|
| Pelvis |
|