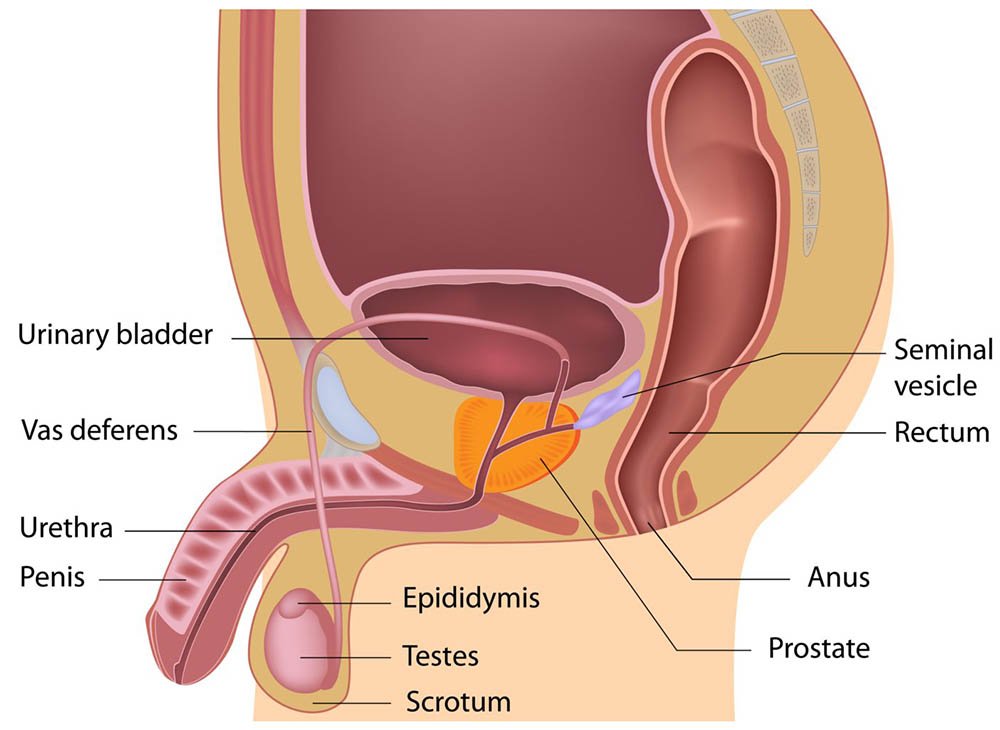
Today our topic of discussion is ” Anatomy and Physiology of the Male Reproductive System “. The male reproductive system is a complex network of organs, ducts, and glands that work in unison to ensure the production, maturation, and transportation of sperm, the male sex cell, and the secretion of sex hormones. Understanding the anatomy and physiology of the male reproductive system not only illuminates how reproduction occurs but also provides insight into the potential disorders that can affect male fertility and overall health.
Anatomy and Physiology of the Male Reproductive System : The Reproductive System
Anatomy of the Male Reproductive System
The primary structures of the male reproductive system include the testes, epididymis, vas deferens, ejaculatory ducts, urethra, seminal vesicles, prostate gland, bulbourethral glands, and the penis.
Testes
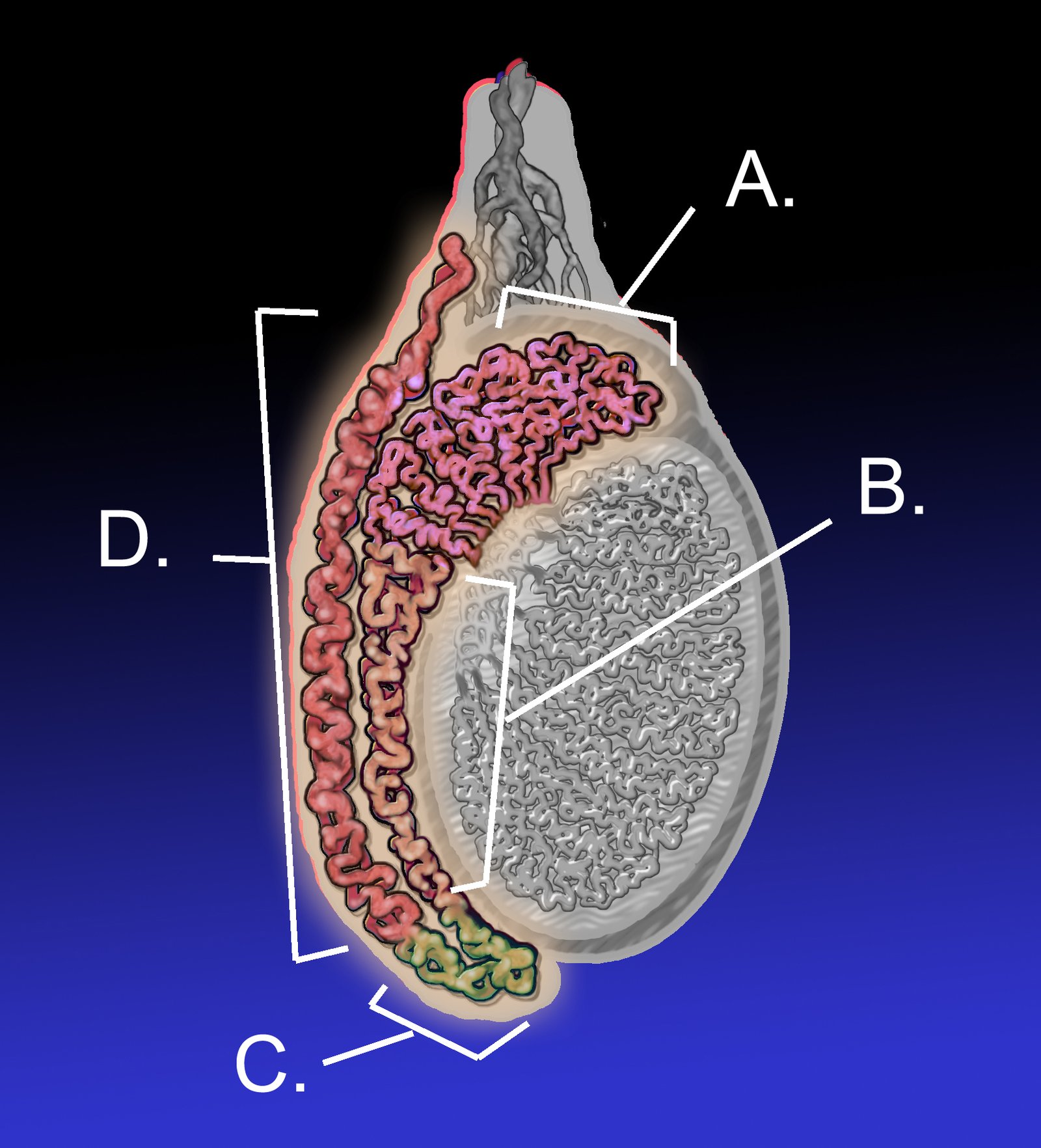
The testes, or testicles, are a pair of oval-shaped organs housed within the scrotum, a skin-covered sac that hangs outside the male body. This external location is vital as it provides a temperature around 2-3 degrees Celsius below body temperature, which is necessary for sperm production.
Each testis is divided into lobules containing seminiferous tubules where spermatogenesis – the production of sperm – occurs. The Leydig cells, located between the seminiferous tubules, are responsible for the production of testosterone, the primary male sex hormone.
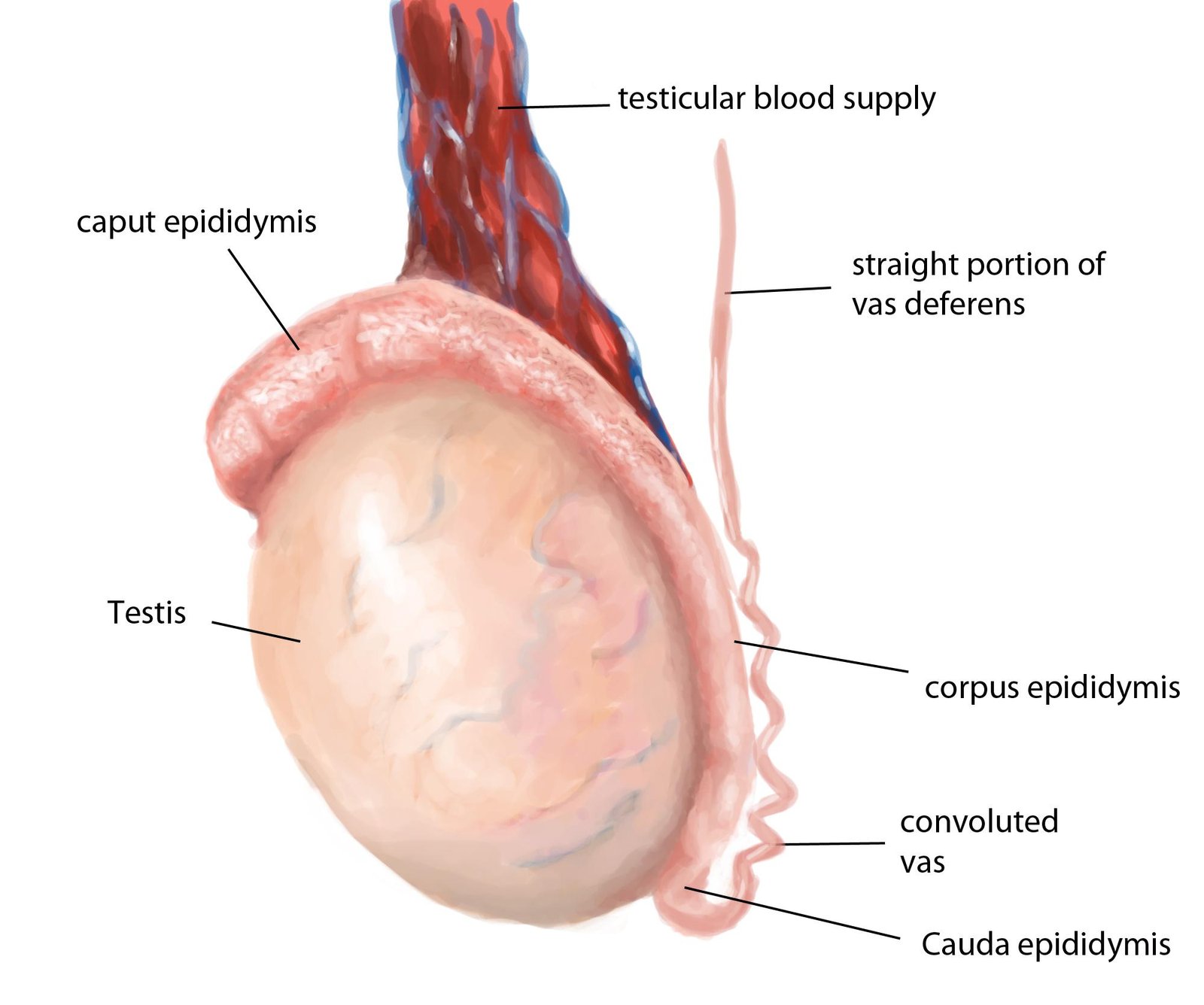
Epididymis
Spermatozoa produced in the seminiferous tubules move into the epididymis, a long, coiled tube that sits atop the testes. Here, sperm mature and gain the ability to swim, a process that takes about two weeks. The epididymis also serves as a storage site for sperm until ejaculation.
Vas Deferens
The vas deferens, or ductus deferens, are muscular tubes that transport mature sperm from the epididymis to the ejaculatory ducts in anticipation of ejaculation. They are part of the spermatic cord, which also includes blood vessels, nerves, and the cremaster muscle that helps regulate the temperature of the testes by raising or lowering the scrotum.
Ejaculatory Ducts and Urethra
The ejaculatory ducts form from the fusion of the vas deferens and the ducts of the seminal vesicles. They pass through the prostate gland and empty into the urethra, the channel that runs through the penis and carries urine out of the body from the bladder, as well as semen during ejaculation.
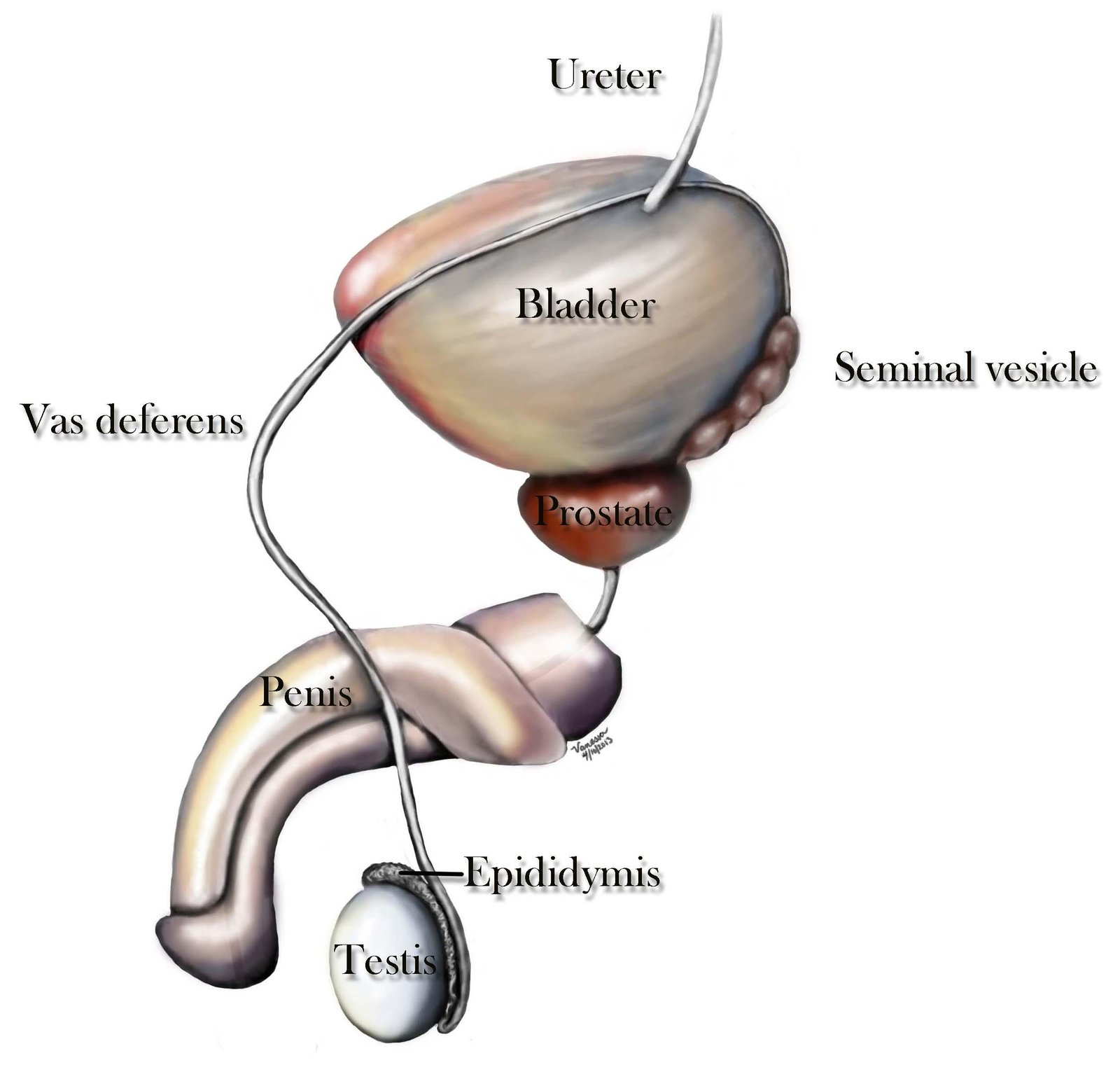
Seminal Vesicles
The seminal vesicles are two small glands that secrete a fluid rich in fructose, which provides energy for the sperm. This secretion makes up about 60-70% of the volume of semen.
Prostate Gland
The prostate is a walnut-sized gland located below the urinary bladder, surrounding the urethra. It produces a slightly alkaline fluid that constitutes about 30% of the semen volume. This fluid helps to neutralize the acidic environment of the vagina, prolonging the lifespan of sperm after ejaculation.
Bulbourethral Glands
Also known as Cowper’s glands, these are pea-sized structures located on either side of the urethra below the prostate. They secrete a clear, mucous fluid that lubricates and neutralizes any acidity in the urethra before the passage of semen during ejaculation.
Penis
The penis serves as the organ of copulation and the conduit for the elimination of urine from the bladder. It consists of a root attached to the pelvic wall, a body or shaft, and an enlarged tip called the glans penis. The penis contains three columns of erectile tissue: two corpora cavernosa on the dorsal side and one corpus spongiosum containing the urethra on the ventral side. During sexual arousal, these tissues fill with blood, causing the penis to become erect, which is essential for sexual intercourse.

Physiology of the Male Reproductive System
The physiology of the male reproductive system encompasses the processes of spermatogenesis, hormone production, and the mechanisms of erection and ejaculation.
Spermatogenesis
Spermatogenesis is the process by which haploid sperm cells are produced from diploid germ cells in the testes. It begins at puberty and continues throughout life, occurring in the seminiferous tubules. The process involves three major phases: mitosis of spermatogonia, meiosis of spermatocytes, and spermiogenesis. This process is regulated by various hormones, including follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland, as well as testosterone.

Hormonal Regulation
The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary gland to secrete FSH and LH. FSH encourages the maturation of germ cells, while LH triggers the Leydig cells to produce testosterone. Testosterone is crucial for the development of male secondary sexual characteristics, maintenance of libido, and the stimulation of spermatogenesis.
Erection and Ejaculation
Sexual arousal initiates a complex reflex that involves the nervous system and the vascular system. Erection results from the dilation of blood vessels leading to the erectile tissues of the penis, coupled with the restriction of venous outflow. The nervous system plays a key role, with both autonomic and somatic fibers involved in the process.
Ejaculation is the expulsion of semen from the male reproductive tract and involves two phases: emission and expulsion. During emission, semen is collected in the urethral bulb. This is followed by expulsion, which is the forceful release of semen through the urethra, facilitated by rhythmic contractions of the pelvic musculature.
Conclusion
The male reproductive system is a marvel of biological engineering, designed to ensure the continued survival of the species through reproduction. Its complexity and precision exemplify the intricate balance of structure and function within the human body.
Understanding the anatomy and physiology of the male reproductive system is not only fundamental to the field of medicine and human biology but also essential for addressing the various health issues that can arise within this system. Through continued research and advances in medical science, we can hope to maintain and improve the reproductive health of males worldwide.
Read more: