Marasmus and Kwashiorkor – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Marasmus and Kwashiorkor
Definition of Marasmus:
Marasmus is the result of a child having a very low intake of energy and nutrients. It often follows severe illness or a period of frequent infections. Marasmus usually occurs in the first 2 years of life, but it can occur at any age, particularly during famines.
Or
Marasmus is a severe form of protein-energy malnutrition that results when a person does not consume enough protein and calories. Without these vital nutrients, energy levels become dangerously low and vital functions begin to stop.
Definition of Kwashiorkor:
Kwashiorkor is more complicated. It is commonest in children aged 1-3 years, but it can occur in order or younger children.
Or
Kwashiorkor is a form of acute malnutrition that most commonly occurs in children. This condition is extremely serious and results from such severe protein deficiencies that a child experiences edema or swelling.
(Ref: Nutrition for Developing Countries/2/222)
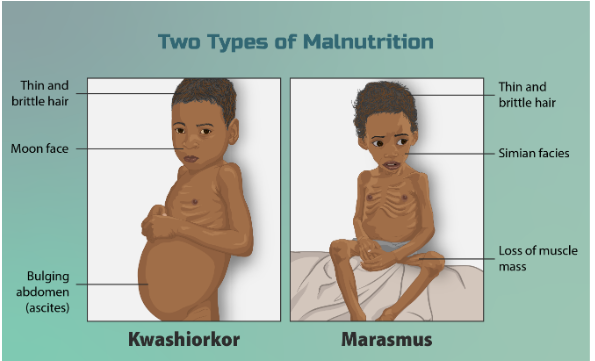
Difference between Kwashiorkor and Marasmus:
| S.N | Biochemical parameter | Kwashiorkor | Marasmus |
| 1. | Age of onset | Pre-school children (1-5 years) | Weaned infants(<1 year) |
| 2. | Nutritional cause | Low protein intake | Low Protein & calorie intake |
| 3. | Weight of body | 60-80% of normal | Less than 60% of normal |
| 4. | Growth | Mild retardation | Severe retardation |
| 5. | Oedema | Present | Absent |
| 6. | Facial appearance | Moon face | Like old man’s face |
| 7. | Abdomen | Protruding | Shrunken |
| 8. | Skin | Dermatitis | Dry and atrophic |
| 9. | Muscles | Undergo wasting | Weak and atrophic |
| 10. | Subcutaneous fat | Present | Absent |
| 11. | Appetite | Poor | Voracious feeder |
| 12. | Serum albumin | 0.5-2 g/dl | 2-3 g/dl |
| 13. | Ribs | Not very prominent | Become very prominent |
| 14. | Serum K+ | Decreased | Normal |
| 15. | Serum cortisol | Normal or decreased | Increased |
| 16. | Hair | Hair changes absent | Hair changes common. |
| 17. | Prognosis | Better | Worse |
Clinical Features:
1. Muscle wasting: Obvious
2. Fat wasting: Severe loss of subcutaneous fat.
3. Oedema: None
4. Weight for height: Very low
5. Mental changes: Sometimes quiet and apathetic
6. Appetite: Usually good
7. Diarrhea: Often (current and past) 8. Skin changes: Usually none
9. Hair changes: Seldom
10. Hepatic enlargement: None

Clinical Features Of Kwashiorkor Patient:
1. Muscle wasting: Sometimes hidden by oedema and fat.
2. Fat wasting: Fat often retained but not firm.
3. Oedema: Present in lower legs, and usually in face and lower arms.
4. Weight for height: Low but may be masked by oedema.
5. Mental changes: Irritable, moaning, apathetic.
6. Appetite: Poor.
7. Diarrhea: Often (current and past)
8. Skin changes: Diffuse pigmentation, sometimes ‘flaky paint dermatosis’.
9. Hair changes: Sparse, silky, easily pulled out.
10. Hepatic enlargement: Sometimes,
11. Due to accumulation of fat.
(Ref: K. Park/24h)
Management of Diet of Kwashiorkor Baby:
Severe PEM whether kwashiorkor baby is death with 3 phases:
- Resuscitation: Correction of dehydration, acidosis, hypoglycaemia and treatment for infection.
- Start of the cure: Re-feeding, gradually working up the calories of 150 kcal/kg with protein about 1.5 g/Kg.
- Nutritional rehabilitation.

Complication of Marasmus & Kwashiorkor:
1. Diarrhoea: Malnourished children may have acute diarrhea, due to the same types of infection that all children may get, such as viruses, bacteria and Giardia.
2. Dehydration: Malnourished children with diarrhea may become dehydrated. This increases the risk of death and requires urgent treatment.
3. Infections: Most severely malnourished children have an infection, for example, otitis media, pneumonia, a urinary tract infection or septicemia.
4. Hypoglycaemia (Low body sugar).
5. Hypothermia (Low body temperature): A child who is severely malnourished easily becomes too cold and may develop hypothermia that is a body temperature below 35.5°C,
6. Anorexia (loss of appetite): Severely malnourished children may not want to eat, which makes it difficult to feed them. This is commonest with children who have kwashiorkor or marasmic kwashiorkor.
7. Anaemia: Most severely malnourished children are anaemic due to iron deficiency and sometimes folate deficiency. (Ref: Nutrition for Developing Countries/2nd/224-225)
Read more: