Medical Acute glomerulonephritis – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Medical Acute glomerulonephritis
Definition of Acute Glomerulonephritis (AGN)
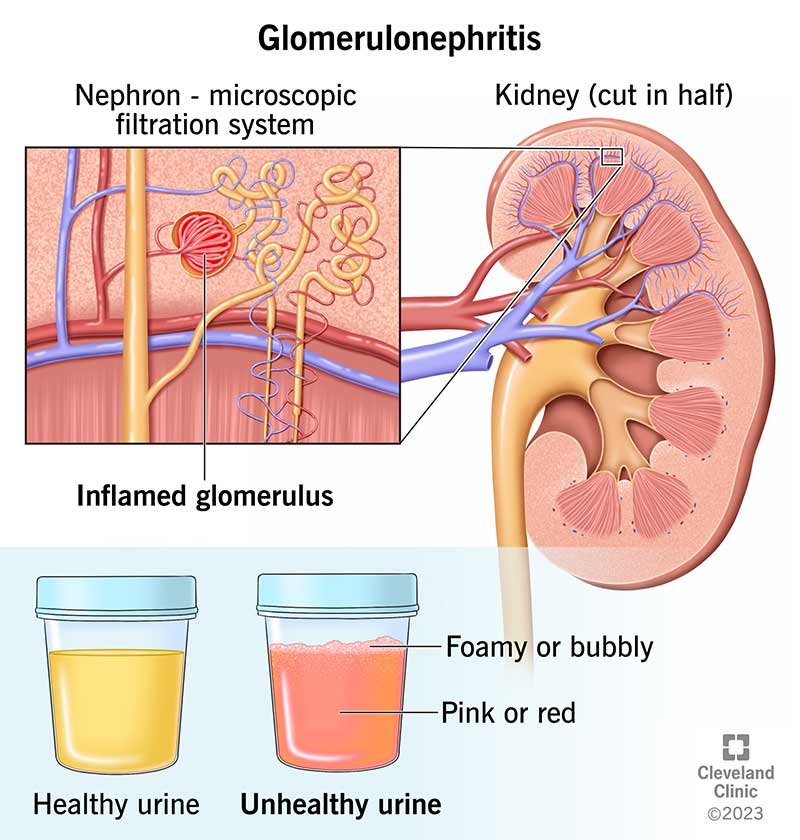
Symptom complex characterized by grossly visible haematuria, mild to moderate proteinuria, oliguria and hypertension is called AGN.
Or
Acute Glomerulonephritis (AGN) is a group of kidney diseases in which it is manifested by inflammation of the glomeruli as a defensive reaction to infection elsewhere in the body.
Causes of Acute Glomerulonephritis
A. Infectious disease:
a) Post streptococcal glomerulonephritis (GN)
- b) Non post streptococcal infection (GN)Bacterial: infective endocarditis, Sepsis.
- Viral: Hepatitis B virus, Measles, Mumps, HIV.
- Parasitic: malaria, toxoplasma.
B. Primary glomerular disease:
a) Membranous proliferative GN
b) Pure meningeal proliferative GN
c) IgA nephropathy
C. Multi-systemic disease:
a) Systemic lupus erythematous.
b) Vasculitis
c) Henoch-schonlein purpura.
D. Miscellaneous:
a) Guillain-Barre syndrome.
b) DPT vaccine.
Diagnosis of AGN
History
- Scanty micturition with high colored urine.
- Sudden onset of puffiness of face which gradually spread all over the body.
- There is H/O sore throat or skin infection few weeks prior to the appearance of S/S. (7- 20 days)
- H/O streptococcal infection (eg. tonsillitis) 1-3 weeks before may present.
C/F (Clinical feature)
Patient usually a child of 5 – 10 years of age (rare before 3 years but adults may affected)
A. Symptoms
- Swelling of face followed by swelling of other parts of body.
- High colored urine
- Scanty micturition
- Fever
- Non specific symptoms: Nausea, Vomiting, anorexia, malaise, lethargy, flank pain, low grade fever.
- Symptoms of complication: Dyspnoea, cough, haemoptysis, Hypertension (may left ventricular failure).
- Sore throat or skin infection.
- Oliguria (renal insufficiency), Proteinuria.
B. Sign’s
- Puffy face, Pallor
- Evidence of skin infection
- Raised BP
- Ascites and edema
- Sign of complication:
- Bilateral basal crepitation
- Papilledema
Investigation
- Urine for RME
- Blood for TC, DC, ESR, Hb%
- Blood urea, serum creatinine, Serum electrolytes
- Bacteriological and serological tests.
- Immunological test
- Serum electrolytes – Hyperkalaemia, hyponatraemia
- Chest X-ray: features of LVF (left ventricular failure) may present.
Pathophysiological Conditions of AGN:
Acute Glomerulonephritis involves both structural changes and functional changes.
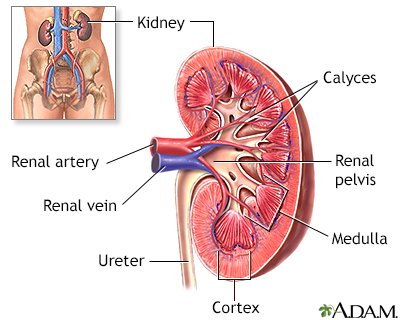
- Structurally, cellular proliferation leads to an increase in the number of cells in the glomerular tuft because of the proliferation of endothelial, mesangial, and epithelial cells. The proliferation may be endo-capillary (i.e., within the confines of the glomerular capillary tufts) or extra-capillary (ie, in the Bowman space involving the epithelial cells).
- In extra- capillary proliferation, proliferation of parietal epithelial cells leads to the formation of crescents, a feature characteristic of certain forms of rapidly progressive GN.
- Leukocyte proliferation is indicated by the presence of neutrophils and monocytes within the glomerular capillary lumen and often accompanies cellular proliferation.
- Glomerular basement membrane thickening appears as thickening of capillary walls on light microscopy.
- Electron-dense deposits can be subendothelial, subepithelial, intramembranous, or mesangial, and they correspond to an area of immune complex deposition.
- Hyalinization or sclerosis indicates irreversible injury.
- These structural changes can be focal, diffuse or segmental, or global.
- Functional changes include proteinuria, hematuria, reduction in GFR (ie, oliguria or anuria), and active urine sediment with RBCs and RBC casts.
- The decreased GFR and avid distal nephron salt and water retention result in expansion of intravascular volume, edema, and, frequently, systemic hypertension.
Management Acute Glomerulonephritis (AGN)
A. General measure:
a) Bed rest
b) Diet:
- Salt restriction (no added salt)
- Normal protein diet
- Fluid restriction- previous day output + 400ml/m² body surface.
- Avoid k containing food ge, Fruits.
B. Supportive Rx:
a) Oedema by diuretics eg, frusemide
b) Hypertension -by anti-hypertensive drug, eg. nifedipine.
e) Antibiotic – For underling streptococcal infection. Benzyl penicillin or Erythromycin for 7-10 days

C. Treatment of complication
D. Regular check up of following:
a) Blood pressure,
b) Urine input and Output chart.
c) Urine RME
d) Renal function test
e) Blood urea
f) Serum creatinine
E. Advice to come for follow up:
a) Once every month for 3 months
b) Once every 3 month for 1 year
Q. Write down the nursing management of AGN?
Nursing management of AGN:
Nursing Assessment
- Physical examination. Obtain complete physical assessment
- Assess weight. Monitor daily weight to have a measurable account on the fluid elimination.
- Monitor intake and output. Monitor fluid intake and output every 4 hours to know progressing condition via glomerular filtration.
- Assess vital signs. Monitor BP and PR every hour to know progression of hypertension and basis for further nursing intervention or referral.
- Assess breath sounds. Assess for adventitious breath sounds to know for possible progression in the lungs.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Ineffective breathing pattern related to the inflammatory process.
- Altered urinary elimination related to decreased bladder capacity or irritation secondary to infection.
- Excess fluid volume related to a decrease in regulatory mechanisms (renal failure) with the potential of water.
- Risk for infection related to a decrease in the immunological defense.
- Imbalanced nutrition less than body requirements related to anorexia, nausea, vomiting.
- Risk for impaired skin integrity related to edema and pruritus.
- Hyperthermia related to the ineffectiveness of thermoregulation secondary to infection.
Nursing Care Planning and Goals
Nursing care planning goals for a child with acute glomerulonephritis are:
- Excretion of excessive fluid through urination.
- Demonstration of behaviors that would help in excreting excessive fluids in the body.
- Improvement of distended abdominal girth.
- Improvement of respiratory rate.
- Participation and demonstration of various ways to achieve effective tissue perfusion.
Nursing Interventions
Nursing care of a child with AGN includes the following interventions:
- Activity: Bed rest should be maintained until acute symptoms and gross hematuria disappears.
- Prevent infection: The child must be protected from chilling and contact with people with infections.
- Monitor intake and output: Fluid intake and urinary output should be carefully monitored and recorded; special attentionis
- needed to keep the intake within prescribed limits.
- Monitor BP: Blood pressure should be monitored regularly using the same arm and a properly fitting cuff.
- Monitor urine characteristics: The urine must be tested regularly for protein and hematuria using dipstick tests.
Evaluation
Goals are met as evidenced by:
- Excretion of excessive fluid through urination.
- Demonstration of behaviors that would help in excreting excessive fluids in the body.
- Improvement of distended abdominal girth.
- Improvement of respiratory rate.
- Participation and demonstration of various ways to achieve effective tissue perfusion.
Documentation Guidelines
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifies of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcome.
Differential Diagnosis of Acute Glomerulonephritis (AGN)
A. Nephrotic syndrome: Because there is
- No high colored urine
- Scanty micturition.
- body swelling – Absent
- Oedema present
- BP not raised
- No massive proteinuira
B. Acute pyelonephritis:
- Oedema absent
- Loin pain and tenderness common
- Dysuria and frequency common
- Urinary red cell cast absent
- Bacteuria and pus cells present
C. Chronic renal failure
D. Henoch-Schonlein purpura.
E. Systemic lupus erythematosus.
Complication of AGN
1. Circulatory problems:
a. Congestive Heart failure
b. Hypertension
c. Endocarditis
Neurologic problems:
a. Hypertensive encephalopathy
b. Seizures
3. End-Stage Renal Disease
4. Fluid and electrolyte imbalance:
a. Hyperkalemia
b. Hyperphosphatemia
c. Hypervolemia
Read more: