Medical Definition of Diarrhea – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Medical Definition of Diarrhea
Diarrhea, also spelled diarrhoea, is the condition of having at least three loose or liquid bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss.
Or,
Diarrhea refers to the passage of liquid / feces and an increased frequency of defecation or it is the discharge of frequent loose stool to the rapid passages of content through the intestines.
Or,
Diarrhea is defined as the passage of loose, liquid or watery stools, more than three times per day.
Or,
Diarrhea is usually defined in epidemiological studies as the passage of three or more loose or watery stools (taking the shape of container) in a 24-hour period.
Causes of Diarrhea:
| A. Infective causes: | a) Viruses:
b) Bacteria:
c) Others:
|
| B. Non-infective causes: | a) Acute diarrhea:
b) Chronic diarrhea:
|

Symptoms of Diarrhea:
- Increased frequency, informed and excessive liquid stools.
- Unable to control the urge to defecate.
- At times, piercing abdominal cramps associated with diarrhea.
- Stools with mucus and blood at times.
- Nausea and vomiting.
- If diarrhea persists, irritation of the anal region.
- Fluid electrolyte loss leading to fatigue, weakness, malaise.
Type of Diarrhea
- According to duration
- Acute diarrhea (< 2 weeks)
- Chronic diarrhea (<2 Weeks or longer)
- Clinical classification
- Acute watery diarrhea (lasting for few hour to day)
- Invasive diarrhea (visible blood with stool)
- Persistent diarrhea: (<2 weeks or longer)
- According to causative agent
- Infective
- Non-infective
- Pathological diarrhea
- Osmotic diarrhea
- Secretory diarrhea
- Inflammatory diarrhea
- Abnormal motility
Assessment of a Patient with Acute Diarrhea
History
- Duration and frequency of diarrhoea
- Volume of stool
- Presence of blood
- Abdominal pain
- Questioning about appropriate suspect foods
- Fever and bloody diarrhoea suggest an invasive, dysenteric process.
- Incubation periods of less than 18 hours suggest toxin-mediated food poisoning;
- A period longer than 5 days suggests diarrhoea caused by protozoa or helminthes
- Other systemic history : Urine output,appetite & associated illness
- Treatment history
- Drug history
- Personal history
- Family or contact history: whether family or community members have been affected & social status
Examination
- Degree of dehydration can be assessed by skin turgor, with pulse and blood pressure measurement.
- Monitoring: Urine output and ongoing stool losses
Investigations
- Stool R/M/E: for blood and microscopy for leucocytes, and also an examination for ova, cysts and parasites.
- Stool culture
- An FBC and serum electrolytes will also indicate the degree of inflammation and dehydration.
- In a malarious area a blood film for malaria parasites should be obtained.
- Blood and urine cultures and chest X-ray may identify alternative sites of infection, particularly if the clinical examination is suggestive of syndrome other than gastroenteritis.
Management of Diarrhea
Principle the management of acute diarrhoea
- Fluid replacement
- Antibiotics/antimicrobial therapy
- Adjunctive antidiarrheal therapy.
Fluid replacement
Replacement of established deficit.
➤Replacement of ongoing loses.
➤ Replacement of normal daily requirement (1 – 1.5 litres/day).
Management of dehydration
➤ Prevention by Home-based fluids
➤ Rehydration by
- a) Oral Rehydration Therapy (ORT):
- Oral Rehydration Salts (ORS)
- New Formulation
- b) Intravenous rehydration :
- Initial management of severe dehydration
- Failure of ORT:
✓ Intractable vomiting
✓ High purging rate
✓ Inability to drink
- Continued Feeding
- Administration of zinc
Antimicrobial agents: According to cause
- Amoebic dysentery – Metronidazole or Tinidazole, Diloxanide furoate.
- Vibrio cholerae – Tetracycline or doxycycline
- Bacillary dysentery – Ciproflaxacin, azithromycin.
Antidiarrhoeal, antimotility and antisecretory agents
- Not recommended in acute infective diarrhoea and their use may even be contraindicated.

Definition of Cholera:
Cholera is a bacterial disease usually spread through contaminated water. Cholera causes severe diarrhea and dehydration. Left untreated, cholera can be fatal in a matter of hours, even in previously healthy people.
Or
This is an acute communicable disease, caused by Vibrio Cholera.
The incubation period is from a few hours to 2 days. The organisms are swallowed with contaminated food and water. In the small intestine they quickly multiply and produce a toxin which causes the intestinal wall to secrete a great deal of water and salts.
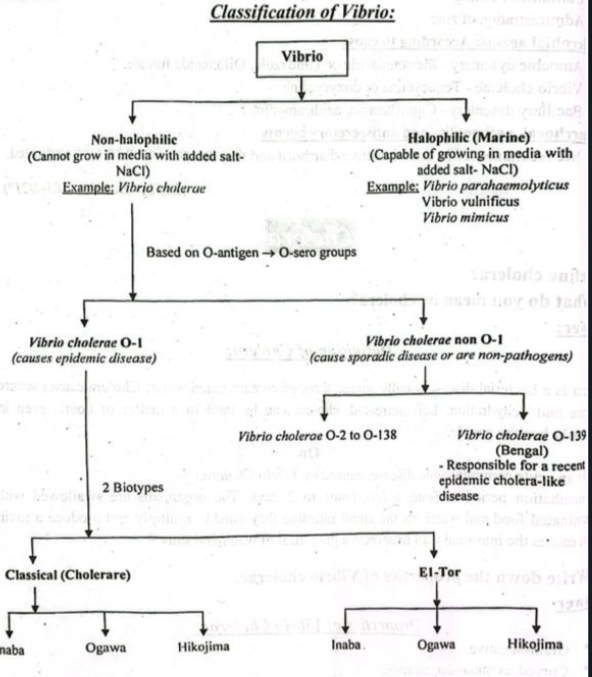
Properties of Vibrio Cholerae:
- Gram-negative.
- Curved, comma-shaped rods.
- Actively motile by means of a single polar flagellum.
- In hanging drop preparation have a ‘fish- in stream’ appearance.
- Facultative anaerobe.
- Most species are oxidase-positive.
- Non-sporing and non-capsulated.
Culture and Growth Characteristics of Vibrio Cholerae:
- Aerobe. Optimum temperature is 37°C.
- Grow at a very high pH (8.5 to 9.5).
- Grow on ordinary media.
- On Monsur’s media (Tellurite gelatin agar media): Dark colonies with characteristic hollows around them.
- On Mac Conkey’s agar: Ferments lactose slowly (colourless/pale colonies).
- On nutrient agar. Circular, smooth and translucent colonies.
- Alkaline peptone water.
Pathogenesis of Cholera:
Fecal contamination of water & food with Vibrio cholerae
↓
Ingestion of contaminated water or food (containing at least 10 Vibrio cholerae)
↓
Organisms pass the acid barrier of stomach & reach the alkaline environment of small intestine
↓
Secretion of bacterial enzyme ‘mucinase’
↓
Protective glycoprotein coat of intestinal cells is dissolved
↓
Adherence of the organisms to the cells of the brush border of the gut & multiplication
↓
Secretion of enterotoxin called choleragen [consists of 2 subunit, a A (active) subunit & a B (binding) subunit]
↓
Subunit B binds to a ganglioside receptor on enterocyte & subunit A enters into the cell.
↓
Persistent stimulation of the enzyme adenylate cylase and overproduction of cAMP
↓
Increased secretion of Cl & H₂0
↓
Massive watery diarrhoea and vomiting.
Lab. Diagnosis of Cholera:
Principle:
It is based on demonstration of Vibrio cholerae by microscopic examination. Isolation and identification is done by bacteriological techniques. Biochemical and serological tests are also helpful.
Steps:
➤ Specimen collection:
- Stool
- Vomit
- Rectal swab
First day:
➤ Microscopic examination:
- Gram staining: Gram-negative comma shaped bacilli.
- Hanging drop preparation: Typical motility (‘a fish in stream’ appearance).
- Dark ground illumination (DGI): Shooting star in dark sky appearance.
Isolation and culture:
- Monsur’s media (Tellurite taurocholate gelatin agar media): Small black
colonies surrounded by characteristic hollows.
- Thiosulphite-Citrate-Bile-Sucrose agar (TCBS agar): Large yellow coloured
colony.
➤ Biochemical tests: Oxidase-positive.
Second day and onwards:
➤ Serological tests:
- Slide agglutination test (mostly used).
- Indirect haemagglutination test.
- ELISA.
Management of Cholera:
- Clinical feature
- a) Symptoms
- Watery diarrhea (sometimes in large volumes)
- Rice-water stools
- Fishy odor to stools
- Vomiting
- Rapid heart rate
- Loss of skin elasticity
- Dry mucous membranes (dry mouth)
- Low blood pressure
- Thirst
- Muscle cramps (leg cramps, for example)
- Restlessness or irritability (especially in children)
- Unusual sleepiness or tiredness

Other symptoms that may occur, especially with more severe disease, include the following:
- Abdominal pain (cramps)
- Rectal pain
- Fever
- Severe vomiting
- Dehydration
- Low or no urine output
- Weight loss
- Seizures
- Shock
- Death
- b) O/E
- Dehydration- present.
- Shock may be present:
✓ Cold & clammy skin
✓ Rapid thready halse
✓ Hypotension
- Eyes- Shunken
- Coma, confusion and death may occur from circulatory failure.
- Investigation:
- a) Stool for R/M/E (Dark field microscopy) – shooting star motility of Vibrio cholera.
- b) Culture of stool or rectal swab.
- Treatment:
- a) Assessment of dehydration & IV channel open. a
- Correction of fluid & electrolyte by IV:
✓ Ringer’s lactate
✔ Cholera saline
✔ Hartman’s solution.
- After blood pressure and pulse is stable, rest of the estimated deficit replacemer slowly by ORS.
- Total fluid requirement is calculated every 8 hourly from urine volume, stool vomit output and insensible loss (5 L/ day in hot climate)
- Total fluid requirement may exceeds 50 litres over 2-5 days.
- b) Tetracycline 250 mg 6 hourly
Or,
Doxicycline 300 mg a single dose Or,
Ciprofloxacin 1 gm daily.
- c) Rx of renal failure if already developed.
Causes of Cholera
- Food poisoning (Salmonella)
- Campylobacter jejuni infection.
- E. coli
- Shigella
- Giardia
- Amoeba
- Rota virus
| Traits | Diarrhea | Cholera |
| 1. Causative organisms | Diarrhea is caused by bacteria, viruses and parasites, which is due to unwise drinking/eating. | Cholera is caused by vibrio cholera. |
| 2. Transmission | Diarrhea is transmitted through impure food and water. | Cholera is transmitted through infected food and water plus direct contact with feces and vomitus. |
| 3. Stages | Diarrhea is not divided into stages but acute and chronic forms. | Cholera has two stages i.e. stage of evacuation and stage of collapse. |
| 4. Diagnosis | Diarrhea is purely a clinical disease but stool examination is carried out to determine the cause. | Cholera is diagnosed through presence of vibrio cholera in stools, culture of stools or rectal swabs.v |
| 5. Treatment | Diarrhea is a self-limiting disease is treated through fluid and electrolyte replacement. | In cholera, along with fluid and water replacement, antibiotics like ciprofloxacin and tetracycline are given. |
| 6. Prevention/ Vaccination | There is no vaccination against diarrhea but only hygienic conditions cause improvement. | Vaccination is present for cholera |
