Medical genetics – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.

Medical genetics
Medical genetics
Medical genetics is the application of this knowledge for understanding health and disease, while clinical genetics is the application for diagnosis, prevention and management of patients with genetic disorders.
Classification of genetic disorders
1. Chromosomal disorders: Entire chromosome or segments of them are missing, duplicated or altered.
2. Examples: Down syndrome (DS), Turner syndrome
3. Single gene disorders (also known as monogenic disorders): Disorders in which single genes are altered-often called “Mendelian” conditions since they follow, Mendelian mode of inheritance. Examples: Thalassemia, Spinal muscular atrophy, Hemophilia
4. Mitochondrial disorders: A relatively small number of diseases are caused by alterations in the small cytoplasmic mitochondrial DNA and are inherited in non- Mendelian fashion
5. Multifactorial disorders: Results from a combination of multiple genetic and environmental causes. Examples:
6. Birth defects like cleft palate/cleft lip, neural tube defect, and common diseases like diabetes, psychiatric illnesses and hypertension
7. Somatic cell genetic disorders: Cancers are caused by additive effects of mutations in several genes in a somatic cell. Other disorders included in this group are autoimmune disorders and aging process.
Congenital anomalies
A WHO document described the terms, the congenital anomaly beingused to include all biochemical, structural and functional disorders present at birth and the congenital malformation should beconfined to structural defects only, present at birth.
Or
The term ‘congenital malformations’ is used to describe developmental defectsthat are present at birth. Approximately 3% of all live births have a detectable malformation and 15-20% of stillborn babies have amajor malformation.
Or
Congenital anomalies are also known as birth defects, congenital disorders or congenital malformations. Congenital anomalies can be defined as structural or functional anomalies (e.g. metabolic disorders) that occur during intrauterine life and can be identified prenatally, at birth or later in life.
Etiology/causes of congenital anomalies
Genetic factors -25%
1. Chromosomal defect:
- Trisomy 21 or Down syndrome
2. Gene defect:
- Single gene defect or unifactorial:
➤ Sickle cell anemia
➤ Polycystic kidney disease - Multifactorial:
➤ Diabetes mellitus
➤ Cleft lip/cleft palate
Environmental factors
1. Intrauterine infections especially by STORCH (Syphilis, Toxoplasmosis, Rubella, Cytomegalovirus and Herpes Virus).
2. Drugs intake by the mother during pregnancy like steroid hormones, stilbestrol, anticonvulsants, folate antagonists, cocaine, lithium, thalidomide, etc.
3. X-ray exposure during pregnancy.
4. Maternal diseases like diabetes, cardiac failure, malnutrition, folic acid deficiency, iodine deficiency disorders, endocrine abnormalities, etc.
5. Abnormal intauterine environment like bicornuate uterus, septed uterus, polyhydromnios, oligohydromnios, fetal hypoxia, etc.
6. Maternal addiction with alcohol, tobacco or smoking (active or passive).
7. Environmental pollution, especially air pollution.

Risk factors of congenital anomalies
Some factors are considered to be significantly associated with incidence of congenital anomalies.
- Advanced maternal age, e.g. elderly mother has risk of birth of baby with Down’s syndrome or other congenital anomalies.
- Consanguinity i.e. Baby born out of consanguineousmarriages (among, blood relations), e.g. marriage with first cousin or uncle- niece, are at risk of congenital defects like mental retardation
- Maternal malnutrition especially folic acid deficiency can lead to CNS defects and iodine deficiency can lead to mental retardation or other congenital anomalies.
Congenital anomalies in children
1. Congenital heart diseases:
- Ventricular septal defect (VSD)
- Atrial septal defect (ASD)
- Patent ductus arteriosus (PDA)
- Coarctation of aorta
- Transposition of great vessels
- Tricuspid atresia
- Truncus arteriosus
- Fallot’s tetralogy
- Aortic stenosis
- Pulmonic stenosis
- Aortic or pulmonary artery dilatation
- Mitral or aortic regurgitation
- Ebstein’s anomaly
- Dextrocardia, etc.
2. Musculoskeletal abnormalities:
- Club foot, (talipes)
- Congenital dislocation of hip
- Osteogenesis imperfecta
- Polydactyl
- Webbed fingers and toes
- Amelia
- Phocomelia
- Congenital scoliosis
- Marfanslmdrome
- Mucopolysaccharidoses (hurler syndrome, hunter syndrome)
- Muscular dystrophies, etc.
3. Respiratory system abnormalities:
- Choanal atresia
- Tracheoesophageal fistula
- Congenital atelectasis
- Pulmonary agenesis
- Congenital stridor
- Congenital cyanosis, etc.
4. Blood disorders:
- Thalassemia
- Hemophilia
- Sickle cell anemia
- Congenital spherocytosis
5. Metabolic disorders:
- Cystic fibrosis
- Phenylketonuria (PKU)
- G-6PD deficiency
- Porphyria
- Congenital lactose intolerance,
- Glycogen storage diseases,
- Mucopolysaccharidoses
- Tay-Sachs disease
- Gaucherdisesase
- Wilson’s disease
- Galactosemia
- Inborn errors of metabolism, etc.
6. Endocrinal abnormalities:
- Congenital hypopituitarism (dwarfism)
- Congenital hypothyroidism (cretinism)
- Congenital adrenogenital hyperplasia
- Congenital goiter
- Diabetes mellitus.
7. Abnormalities of genitourinary system:
- Renal agenesis
- Congenital hydronephrosis
- Congenital polycystic kidney
- Horse-shoe kidney,
- Posterior urethral valves (pliv)
- Hypospedias
- Epispedias
- Ectopiavasicae
- Congenital phimosis
- Congenital hydrocele
- Undescended testis
- Congenital inguinal hernia
- Ambiguous genitalia
- Malformations of reproductive organs, etc.
8. Gastrointestinal system abnormalities:
- Tracheoesophageal fistula
- Esophageal atresia
- Congenital pyloric stenosis
- Duodenal atresia
- Meconium ileus
- Malrotation of gut
- Exomphalos
- Umbilical hernia
- Diaphragmatic hernia
- Femoral hernia
- Congenital intestinal obstruction
- Gastroschisis, etc.
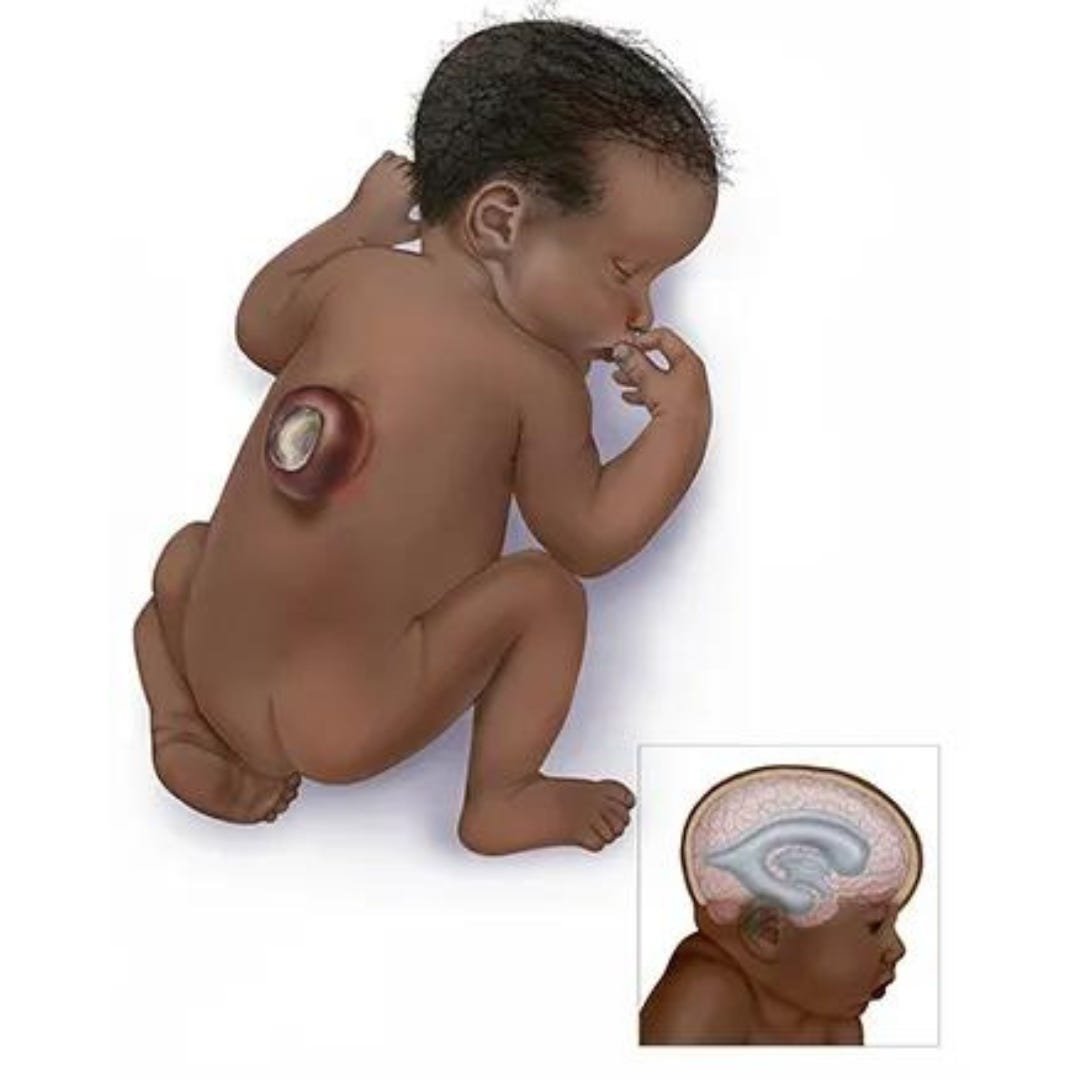
9. Central nervous system defects:
- Anencephaly
- Spina bifida occulta
- Spina bifida cystica (meningocele, meningomyelocele, meningoencephalocele, encephalocele)
- Hydrocephalus
- Microcephaly (microencephaly)
- Macrocephaly
- Syringomyelia
- Tethered spinal cord
- Diastematomyelia
- Porencephaly
- Schizencephaly
- Agenesis of cranial nerves, etc.
10. hromosomal abnormalities:
- Down’s syndrome (trisomy 21)
- Pataut syndrome (trisomy-13)
- Edward’s syndrome (trisomy-18)
- Turner syndrome (xo)
- Klinefelter’s syndrome
- Cri du chat syndrome (cat like cry of infant).
11. Miscellaneous:
- Congenital cataract
- Congenital glaucoma
- Retinoblastoma
- Color blindness
- Congenital deafness
- Deaf and dumb
- Mental retardation
- Microagnatha
- Albinism
- Hemangioma
- Pseudohermophroditism
- Situs inversus,
- Prader-willi syndrome
- Apert syndrome
- Congenital biliary atresia
Nursing responsibilities towards congenital anomalies
The nurse is usually the first person with whom the family has contact. The nurse can help the family by the following ways –
1. Collection of detail history of prenatal, natal and postnatal period.
2. Preparation of pedigree chart by interview and home visit
3. Identification of present problems, its nature and severity, for necessary interventions.
4. Participation in diagnostic investigations, treatment, follow-up and research project.
5. Provide necessary information to the parents and family members.
6. Motivate the family members for genetic counseling and referring to the genetic clinic
7. Participating in genetic counseling process with special training, personal experience, knowledge and competency
8. Provide emotional support and answer questions asked by the counselee
9. Guide the family for rehabilitation, of the child and for available, social and economical support.
10. Promote public awareness about the prevention of Congenital anomalies by individual or group health education or by mass media information.
Prevention of congenital anomalies
1. Genetic counseling is the true preventive measure of congenital anomalies.
2. Reducing and discouraging consanguineous marriages.
3. When blood relatives marry each other there is an increased risk in the offspring of traits controlled by recessive genes and those determined by polygenes.
4. Avoiding late marriage of females and avoidance of pregnancy beyond the age of 35 years.
5. Promotion of health of girl child and pre-pregnant health status of the females by prevention of malnutrition, anemia, folic acid deficiency, iodine deficiency, etc.
6. Encouraging the immunization of all girl child by MMR (Mumps, Measles, and Rubella).
7. Increasing attention to the protection of individuals and whole communities against mutagens such as X-ray and other ionizing radiations and also for chemical mutagens (drugs, alcohol).
8. Immunization by anti-D immunoglobulin to the ‘Rh negative’ mothers after abortion or first child birth to prevent Rh-hemolytic disease of the newborn which is a genetically determined immunological disorder.
9. Elimination of active and passive smoking of tobacco by mothers.
10. Avoidance of drug intake without consulting physician in the first trimester of pregnancy.
11. Prevention of intrauterine infections and promotion of sexual hygiene along with general hygienic measures.
12. Efficient antenatal care especially removal of teratogens, periconceptional supplementation of folic acid, and prevention of maternal malnutrition by adequate diet prenatal diagnosis of suspected genetic disorders and maternal diseases, appropriate treatment of maternal diseases and infections, prevention of fetal hypoxia, etc.
13. Promotion of therapeutic abortion of abnormal fetus and fetus with gross congenital anomalies, after prenatal diagnosis.
14. Discouraging reproduction after birth of a baby with congenital anomalies, without genetic counseling. The risk of malformations in subsequent pregnancies is increased by 10 times.
15. Increasing public awareness about the risk factors and etiological factors of congenital
anomalies and their preventive measures.
16. Promotion of detection of genetic carriers, e.g. both partners should arrange to test for thalassemia carrier before marriage.
17. Reducing the frequency of hereditary disease and disability in the community to as low as possible by negative eugenics. The persons who are suffering from serious hereditary disease are debarred from producing children or sterilized, there should be no serious objection to marriage.