Medical Peptic Ulcer Disease – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.

Medical Peptic Ulcer Disease
Definition of Peptic Ulcer Disease
The term “Peptic ulcer’ refers to ulceration in any part in the gastrointestinal tract, which are exposed to aggressive action of acid pepsin.
Or,
Ulceration in any portion of the gastrointestinal tract expose to the aggressive action of acid peptic juices ulcer penetrate the muscular is mucosa but erosion not involved.
Nice to know
| Ulcer penetrate the muscular is mucosa but erosion not involved. Age: Middle aged between 25-30 yrs M:F:
Prevalence of peptic ulcer in Bangladesh (point prevalence)
Types:
|
(Ref by: Davidson-798/23rd)
Sites of Peptic Ulcer
Lower end of oesophagus.
Sites of Peptic Ulcer
Stomach (90% on the lesser curvature usually antrum).
Duodenum (usually in the 1st part within 2.5 cm of pylorus)- 50% are on the anterior wall.
Jejunum after surgical anastomosis in stomach. (stomal ulcer).
Ileum adjacent to Meckel’s diverticulum (rare) that contain ectopic gastric mucosa 6. Throughout GIT in Zollinger-Ellison syndrome.
(Ref by: Davidson-798/23)
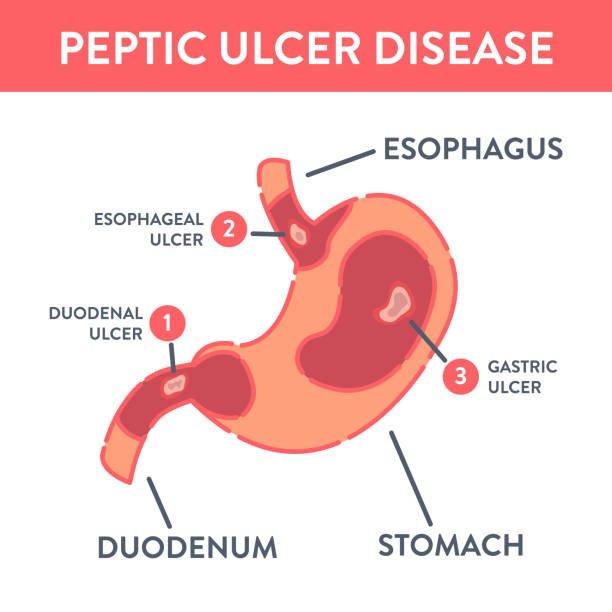
Classification of Peptic Ulcer
Peptic ulcer is classified into gastric, duodenal or esophageal ulcer.
1. Gastric ulcer: Gastric ulcer tend to occur in the lesser curvature of the stomach, near the pylorus.
2. Duodenal ulcer: Peptic ulcers are more likely to occur in the duodenum than in the stomach.
3. Esophageal ulcer: Esophageal ulcer occur as a result pf the backward flow of HCI from the stomach into the esophagus.
Cause of Peptic Ulcer Disease:
A. Most common
a) Infection: (Most common cause)
a) H. Pylori infection: Around 90% of DU pt. & 70% of GU pts. are infected with H. Pylori.
b) NSAID
b) Damage the gastric mucosal barrier & are an important etiological factor in up to 30% of GU.
c) Smoking
c) Delay’s healing & promote recurrence
B. Others
a) Acid-pepsin versus mucosal resistance:
d) An ulcer forms when there is an imbalance between aggressive factors ie the digestive power of acid & pepsin, and defensive factors, ie the ability of the gastric & duodenal mucosa to resist this digestive power.
b) Genetic (have positive family history) & blood group ‘O’:
a) 3 times more likely to develop peptic ulcer than others
c) Neurogenic:
a) Stimulation of vagus results in gastric hypersecretion & hypermotility
b) Stress & anxiety
e) Burn & CVD.
d) Endocrine
a) Zollinger-Ellison syndrome (ZES)
b) Multiple adenoma syndrome
c) Hyperparathyroidism
e) Drug abuse
a) Aspirin
f) Accessory cause
a) Alcohol
b) Inadequate mastication
e) Irregular meal
d) Vitamin deficiency
e) Ischaemia
f) Shock
(Ref: Davidson-789/23 +Robbins/8)
Management of Peptic Ulcer Disease
1. Clinical feature
A. History
a) Usually middle age, smoker.
b) Food habit- irregular.
c) Drugs -NSAIDS, steroids
d) Stress-Psychological, burn
e) Previous abdominal operation
f) Previous abdominal pain.
B. Symptoms
a) Main symptoms – Recurrent abdominal pain (three notable characteristics)
- Localization to the epigastrium
- Relationship to food
- Episodic occurrence
- Burning or gnawing in character.
- Pain may occur after meal or in empty stomach.
- Nocturnal pain
b) Nausea & vomiting
c) Anorexia in gastric ulcer but appetite duodenal ulcer.
d) Sense of undue repletion after meals.
e) A vague sense of epigastric unease
f) Persistent daily vomiting suggests gastric outlet obstruction.
g) In some patients the ulcer is completely ‘silent’, presenting for the first time with
- Anaemia from chronic undetected blood loss
- As an abrupt haematemesis or
- As acute perforation.
C. Signs:
a) G/E
- Anaemia-more in G.U.
b) Local
- Duodenal point tenderness present in D.U. (2.5cm Rt from mid-point of transpyloric plane and 1.25 cm above the point)
- Epigastric tenderness present in G.U
2. Investigations:
Epigastric tenderness present in G.U
a) Specific
Endoscopy of upper GIT
- Direct visualization of an ulcer site as well as taking biopsy for all cases of gastric ulcer.
c) Ba meal X-ray of stomach & duodenal cap series.
- Gastric ulceran ulcer niche.
- Duodenal ulcer-an ulcer crater
d) Demonstration of H. pylori status
- Non-invasive-serology, urea breath test. faecal antigen test.
- Invasive-histology, rapid urease test, microbiological culture
b) Routine
- Hb%
- CBC, ESR
- USG and ERCP [to exclude other possibilities such as acute pancreatitis, liver abscess]
- Stool for occult blood test-for evidence of chronic blood loss.
- Studies for gastric function
✔ Peak acid output test.
✔ Insulin test.
3. Management
A. Aim of Mx
a) Relieve symptoms
b) Induce ulcer healing in short time
c) Prevent recurrence
B. General measures
a) Modification of life style such as cessation of smoking
b) Avoidance of precipitating drug- aspirin, NSAID, steroid
c) Diet-Normal but avoid those food which aggravates his/her symptoms
d) Avoid spicy & fried food.
e) Regular & timely diet.
C. H. pylori eradication therapy: (Cornerstone of therapy)
a) 1st line therapy (primary) – for 07 days
- Omeprazole 20 mg 12 hrly
- Amoxycillin 1gm 12 hrly
- Clarithromycin 500 mg 12 hrly or Metronidazole 400 mg 12 hriy
b) 2nd line therapy (failure of 1st line): Quadruple therapy – for 14 days
- Omeprazole 20 mg 12 hrly
- Bismath 120 mg 6 hrly
- Metronidazole 400 mg 08 hrly.
- Tetracycline 500 mg 6 hrly
c) 3rd line therapy or rescue therapy
- If 2nd line therapy fails then therapy given after antibacterial sensitivity test
d) Maintenance therapy
- Continuous maintenance treatment should not be necessary after successful H. pylori eradication.
- For the minority who do require it, the lowest effective dose of PPI should be used.
- PPI should be continued for 2 months.
D. Surgical Rx
- Option in duodenal ulcer
- Vagotomy with gastric drainage operation
- Option in gastric ulcer
- Billroth I partial gastrectomy
- Billroth II gastrectomy
- Vagotomy, pyloroplasty
(Ref: Davidson’s/234/799-800)
Complications of Peptic Ulcer/Chronic Duodenal Ulcer
A. Acute complications
- Perforation. (5%)
- Haematemesis and/or melaena. (15-20%)
B. Intermediate complication
- Residual abscess.
C. Chronic complications
- GOO
- Penetration into neighboring viscera specially the pancreas, liver and retroperitoneal space also.
- Carcinoma (gastric ulcer).
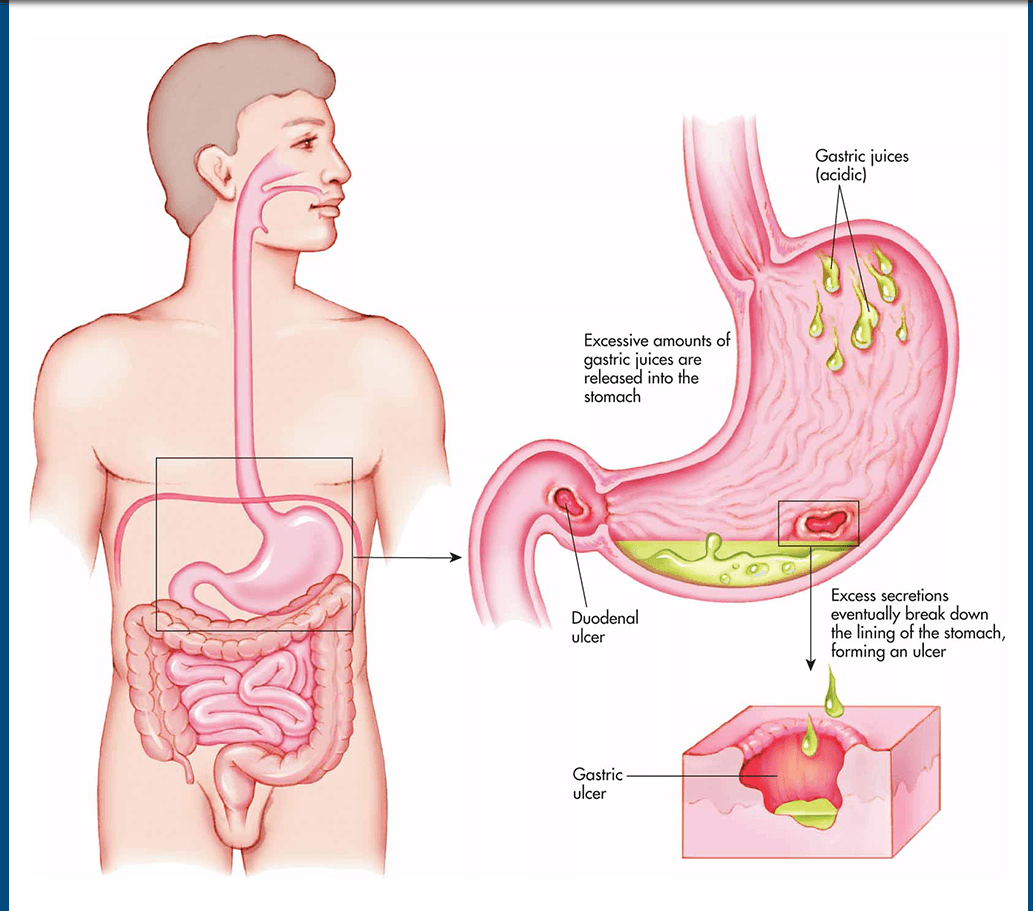
Pathophysiology of Peptic Ulcer
Peptic ulcers occur mainly in the gastro duodenal mucosa.
1. Erosion: The crosion is caused by the increased concentration or activity of acid-pepsin or by decreased resistance of the mucosa.
2. Damage: A damaged mucosa cannot secrete enough mucus to act as a barrier against HCI.
3. Acid secretion: Patients with duodenal ulcers secrete more acid than normal, while patients with gastric ulcer tend to secrete normal or decreased levels of acid.
4. Decreased resistance: Damage to the gastroduodenal mucosa results in decreased resistance to bacteria and thus infection from the H. pylori bacteria may occur.
Peptic Ulcer Disease
Helicobacter Pylori
Helicobacter pylori is the bacteria which is strongly associated with peptic ulcer disease.
Disease Caused by Helicobacter Pylori:
- Gastritis.
- Peptic ulcer disease: Duodenal ulcer & Gastric ulcer.
- Infection with H. pylori is a risk factor for gastric carcinoma.
Lab. Diagnosis of Helicobacter pylori:
Principle:
Diagnosis is based on demonstration of causative organism by microscopic examination and isolation & identification by bacteriological techniques. Serological tests are also helpful.
Steps:
➤Specimen collection:
- Biopsy specimen of gastric mucosa.
- Blood for serum antibodies.
➤Non-invasive tests:
- Urea breath test.
- Serological test: Ab detection.
- “C bicarbonate assay.
- Antigen detection in stool & urine.
- PCR in stool, dental plaque and water supplies.
➤Invasive tests:
- Endoscopy & biopsy.
- Rapid urease test (RUT).
- Histopathology & microscopy: Gram staining & Giemsa staining.
- Culture (Skirrow’s media at 42°C).
- PCR in gastric juice.
Important properties of H. pylori:
- Gram-negative.
- Curved rods.
- Urease positive.
- It has multiple flagella at one pole and is actively motile.
- Microaerophilic (i.e.- requires less O concentration for survival)
- Oxidase positive, catalase positive.
Pathogenesis of H. pylori:
Large number of H. pylori enters into the stomach
↓
Produce the enzyme urease
↓
Breakdown of urea to ammonia
↓
An alkaline media is created and therefore the bacteria escapes from the action of gastric HCI
↓
H. pylori multiply under the mucous & produce tissue degrading enzymes
↓
Peptic ulcer disease
(Ref by- LANGE review /15/156)
Nursing Management of Peptic Ulcer Disease
Nursing Assessment
Nursing assessment includes:
- Assessment for description of pain.
- Assessment of relief measures to relieve the pain.
- Assessment of the characteristics of the vomitus.
- Assessment of the patient’s usual food intake and food habits.
Nursing Diagnosis
Based on the assessment data, the patient’s nursing diagnoses may include the following:
- Acute pain related to the effect of gastric acid secretion on damaged tissue.
- Anxiety related to an acute illness.
- Imbalanced nutrition related to changes in the diet.
- Deficient knowledge about prevention of symptoms and management of the condition.
Nursing Care Planning & Goals
The goals for the patient may include:
- Relief of pain.
- Reduced anxiety.
- Maintenance of nutritional requirements.
- Knowledge about the management and prevention of ulcer recurrence.
- Absence of complications.
Nursing Interventions
Nursing interventions for the patient may include:
Relieving Pain and Improving Nutrition
- Administer prescribed medications.
- Avoid aspirin, which is an anticoagulant, and foods and beverages that contain acid-enhancing caffeine (colas, tea, coffee, chocolate), along with decaffeinated coffee.
- Encourage patient to eat regularly spaced meals in a relaxed atmosphere; obtain regular weights and encourage dietary modifications.
- Encourage relaxation techniques.
Reducing Anxiety
- Assess what patient wants to know about the disease, and evaluate level of anxiety; encourage patient to express fears openly and without criticism.
- Explain diagnostic tests and administering medications on schedule.
- Interact in a relaxing manner, help in identifying stressors, and explain effective coping techniques and relaxation methods.
- Encourage family to participate in care, and give emotional support.
Monitoring and Managing Complications
If hemorrhage is a concern:
- Assess for faintness or dizziness and nausea, before or with bleeding; test stool for occult or gross blood; monitor vital signs frequently (tachycardia, hypotension, and tachypnea).
- Insert an indwelling urinary catheter and monitor intake and output; insert and maintain an IV line for infusing fluid and blood.
- Monitor laboratory values (hemoglobin and hematocrit).
- Insert and maintain a nasogastric tube and monitor drainage; provide lavage as ordered.
- Monitor oxygen saturation and administering oxygen therapy.
- Place the patient in the recumbent position with the legs elevated to prevent hypotension, or place the patient on the left side to prevent aspiration from vomiting.
- Treat hypovolemic shock as indicated.
If perforation and penetration are concerns:
- Note and report symptoms of penetration (back and epigastric pain not relieved by medications that were effective in the past).
- Note and report symptoms of perforation (sudden abdominal pain, referred pain to shoulders, vomiting and collapse, extremely tender and rigid abdomen, hypotension and tachycardia, or other signs of shock).
Evaluation
Expected patient outcomes include: Relief of pain.
- Reduced anxiety.
- Maintained nutritional requirements.
- Knowledge about the management and prevention of ulcer recurrence.
- Absence of complications.