Complication that might occur in Rh negative female-The course is designed for the basic understanding of anatomical structures and physiological functions of human body, musculoskeletal system, digestive system, respiratory system; cardiovascular system; urinary system, endocrine system, reproductive system, nervous system, hematologic system, sensory organs, integumentary system, and immune system.The aim of the course is to acquire knowledge and skills regarding anatomy and physiology.
Complication that might occur in Rh negative female
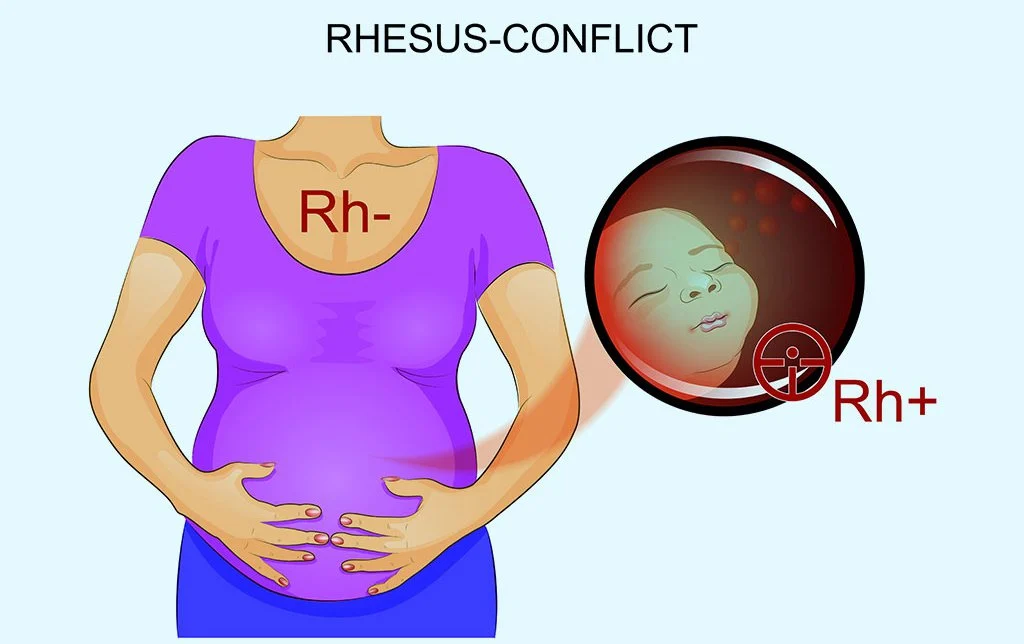
Erythroblastosis fetalis is a disease of the fetus and newborn child characterized by agglutination and phagocytosis of the fetus’s RBCs. In most instances of Erythroblastosis fetalis, the mother is Rh negative and the father is Rh positive.
The baby has inherited the Rh positive antigen from father, and mother develops anti-Rh agglutinins from exposure to the fetus’s Rh antigen. In turn, the mother’s agglutinins diffuse through the placenta into the fetus and causes RBC agglutination.
Complication of Rh-negative female:
If the Rh negative female contains Rh-positive fetus, Rh incompatibility may develop which may lead to the following complications:
- Erythroblastosis fetalis.
- If the hemolysis is severe, kernicterus & hydrops fetalis may develop. (Ref: Guyton and Hall, 13th ed, P-449).
Erythroblastosis fetalis: In this condition, hemolysis occurs. If the hemolysis is severe, the following condition may developed-
- kernicterus.
- Hydrops fetalis.
Treatment:
Exchange transfusion by Rh(-ve) blood.
Prevention:
Mother should receive an anti-D injection during
- 28 and 34 week of gestation
- Within 72 hours after delivery
Blood Clotting factors and blood clotting factors
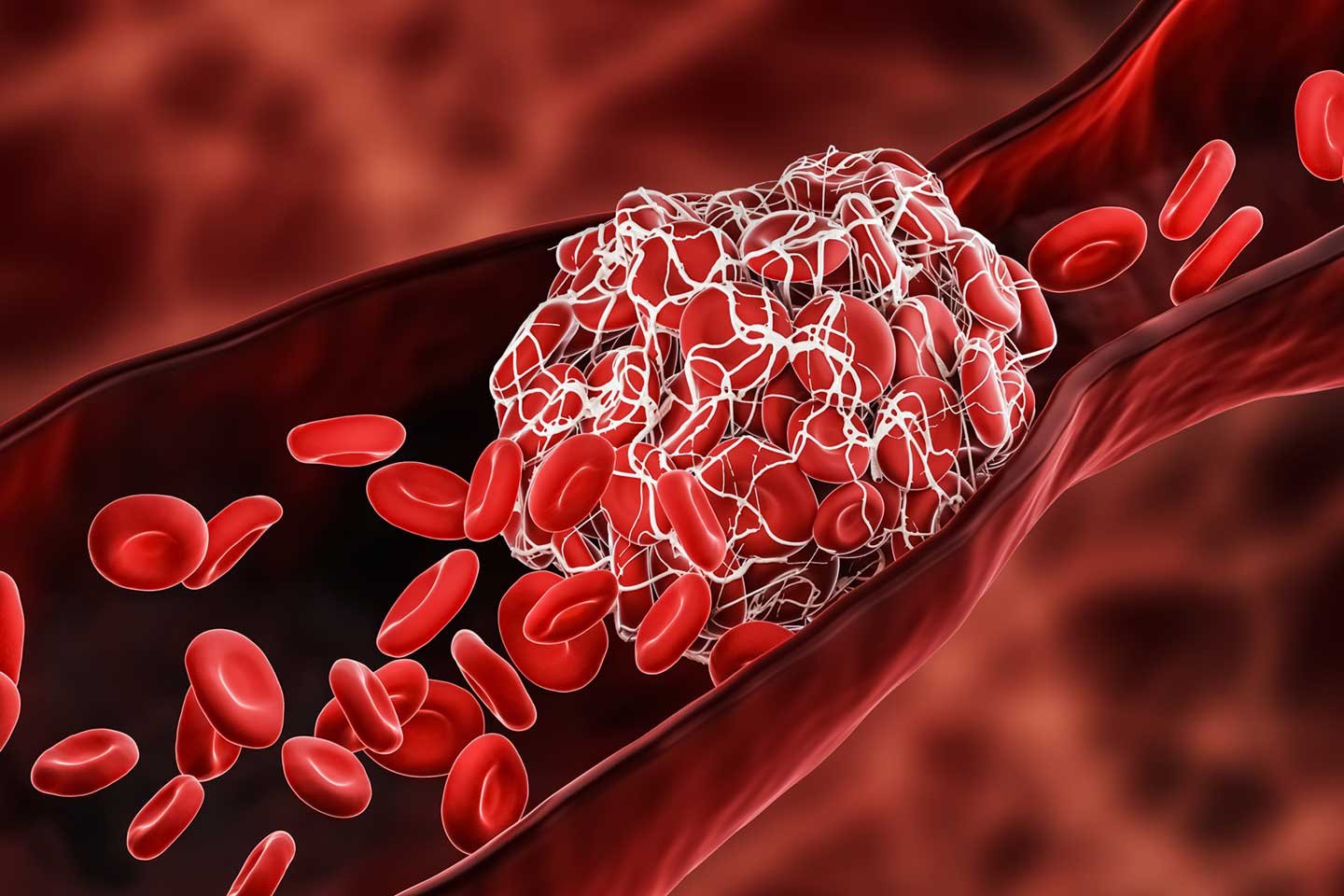
Normally, blood remains in its liquid form as long as it stays within its vessels. If it is withdrawn from the body, however, it thickens and forms a gel. Eventually, the gel separates from the liquid. The straw-colored liquid, called serum, is simply plasma minus the clotting proteins.
The gel is called a clot and consists of a network of insoluble protein fibers called fibrin in which the formed elements of blood are trapped. In haematology, the term coagulation refers to clotting or the process of clot formation.
A blood clot is a thrombus that forms inside of a blood vessel. It forms when blood changes its form from liquid to a gel. it occurs to prevent blood loss from a damaged or injured blood vessel. This is one of the initial steps in tissue injury repair and wound healing.
The process of clot formation, called clotting (coagulation), is a series of chemical reactions that culminates in the formation of fibrin threads. If blood clots too easily, the result can be thrombosis, clotting in an unbroken blood vessed.
If it takes too long to clot, hemorrhage can result. Clotting is a complex process in which various chemicals known as clotting factors activate each other. Clotting (coagulation) factors include calcium ions (Ca2), several enzymes that are made by liver cells and released into the blood, and various molecules associated with platelets or released by damaged tissues. Many clotting factors are identified by Roman numerals. Clotting occurs in three stages
- Prothrombinase is formed.
- Prothrombinase converts prothrombin (a plasma protein formed by the liver with the help of vitamin K) into the enzyme thrombin.
- Thrombin converts soluble fibrinogen (another plasma protein formed by the liver) into insoluble fibrin. Fibrin forms the threads of the clot. (Cigarette smoke contains substances that interfere with fibrin formation.)
Prothrombinase can be formed in two ways, by either the extrinsic or the intrinsic pathway of blood clotting. The extrinsic pathway of blood clotting occurs rapidly, within seconds. It is so-named because damaged tissue cells release a tissue protein called tissue factor (TF) into the blood from outside (extrinsic to) blood vessels.
Following several additional reactions that require calcium ions (Ca2) and several clotting factors, tissue factor is eventually converted into prothrombinase. This completes the extrinsic pathway. The intrinsic pathway of blood clotting is more complex than the extrinsic pathway, and it occurs more slowly, usually requiring several minutes. The intrinsic pathway is so-named because its activators are either in direct contact with blood or containedwithin (intrinsic to) the blood.
Blood clotting factors
| Factor | Name | Function | Pathway |
| I | Fibrinogen | Converted to fibrin | Common |
| II | Prothrombin | Converted to thrombin (enzyme) | Common |
| III | Tissue thromboplastin | Cofactor | Extrinsic |
| IV | Calcium ions (Ca) | Cofactor | Intrinsic,Extrinsic and Common |
| V | Proaccelerin | Cofactor | Common |
| VI | Factor VI is no longer referenced; it is now believed to be the same substance as activated factor V. | ||
| VII | Proconvertin | Enzyme | Extrinsic |
| VIII | Antihemophilic factor | Cofactor | Intrinsic |
| IX | Plasma thromboplastin component ;Christmas factor | Enzyme | Intrinsic |
| X | Stuart-Prowers factor | Enzyme | Common |
| XI | Plasma thromboplast in antecedent | Enzyme | Intrinsic |
| XII | Hageman factor | Enzyme | Intrinsic |
| XIII | Fibrin stabilizing factor | Enzyme | Common |