Nutritional assessment – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Nutritional assessment

Concept about Nutritional Assessment
Nutritional assessment is an in-depth evaluation of both objective and subjective data related to an individual’s food and nutrient intake, lifestyle, and medical history.
Once the data on an individual is collected and organized, the practitioner can assess and evaluate the nutritional status of that person. The assessment leads to a plan of care, or intervention, designed to help the individual either maintain the assessed status or attain a healthier status.
Nutritional Assessment:
Nutritional assessment is an in-depth evaluation of both objective and subjective data related to an individual’s food and nutrient intake, lifestyle, and medical history.
Or
Nutrition is one of the most essential aspects in life for all. Diet, whether therapeutic or regular, has a major impact on a person’s health, maintenance and recovery from an illness. Nutritional behavior is a lifestyle that is influenced by culture; it must be considered as the nurse provides advice and guidance to individuals and families.
Or
Nutritional assessment is the interpretation of anthropometric, biochemical (laboratory), Clinical and dietary data to determine whether a person or groups of people are well nourished or malnourished (over- nourished or under-nourished).
Purposes of Nutritional Assessment:
- To identify individuals or population groups at risk of becoming malnourished
- To identify individuals or population groups who are malnourished
- To develop health care programs that meet the community needs which are defined by the assessment
- To measure the effectiveness of the nutritional programs & intervention once initiated
Anthropometric Assessment
Anthropometric measurements are a series of quantitative measurements of the muscle, bone, and adipose tissue used to assess the composition of the body. The core elements of anthropometry are height, weight, body mass index (BMI), body circunferences (waist, hip, and limbs), and skinfold thickness.
Or
Anthropometric measurements are used to assess the size, shape and composition of the human body. Learn about common methods used to gather these measurements, such as BMI, waist-to- hip ratio, skin-fold test and bioelectrical impedance.
Indications
There are several possible indications for anthropometric measurements. In children, indications include stunting, wasting, and being “aderweight. Stunting is when children have a low height-for-age, wasting is a low weight-for-height, and underweight is a low weight-for-age.
Mid-upper arm circumference (MUAC) is a viable measurement in children or pregnant women as a marker of nutritional status. BMI is another commonly employed index of nutritional status and used as a gauge of malnutrition in children and adults. BMI is useful to identify obesity and the severity of obesity. Anthropometric measurements are often also used as part of the evaluation of fitness in athletes.
Contraindications
There are few contraindications to anthropometric measurement. The contraindications would be those that result from a condition that would make taking the measurement impossible or inaccurate, such as amputations or casting.
Nutritional Anthropometry:
Anthropometric measurements include.
1. Height (cm) and weight (kg): Weight is judged in relation to age and height, also height is judged in relation to age.
a) Weight for age: This is used an index of malnutrition. But major difficulty is that, in most cases, the ages of the children are unknown.
b) Height for age: This gives a picture of past nutritional history. But this is also age
dependent.
c) Weight for height: This is age independent and is used as an index of current nutritional status.
2. Arm circumference: The left arm circumference is measured at the mid-point between the acromial process of scapula and olecranon process of ulna.
3. Skin fold thickness: It is measured by skin calipers over the triceps and sub scapular region.
In young children, additional measurements, such as head circumference and chest circumference are made.
(Ref: June D Thompson/2nd/253)
Methods of Nutritional Assessment:
Direct Methods of Nutritional Assessment
These are summarized as ABCD
- Anthropometric methods
- Biochemical, laboratory methods
- Clinical examination methods
- Dietary evaluation methods
Indirect Methods of Nutritional Assessment
These include three categories:
- Ecological variables / factors.
- Economic factors e.g. per capita income, population density & social habits
- Vital health statistics particularly infant & under 5 mortality & fertility index
(Ref: K. Park/25/648+ Handout)
Nutritional Surveillance:
Nutritional surveillance has been defined as “Keeping watch over nutrition, in order to make decisions that will lead to improvement in nutrition in population”. Three distinct objectives have been defined for surveillance systems:
1. To aid long-term planning in health and development.
2. To provide input for program management and evaluation.
3. To give timely warning and intervention to prevent short-term food consumption crises.
(Ref: K. Park/25/649)
Nutritional Status
Definition Of Nutritional Status:
Nutritional status is the condition of health of the individual as influenced by the utilization of the nutrients. It can be determined only by the correlation of information obtained through a careful medical and dietary history, a thorough physical examination and appropriate laboratory investigations.
(Ref: Robinson’s Normal and Therapeutic Nutrition/14th/6)
Nutritional Status Indicators:
Nutritional status is a positive health indicator. Three nutritional status indicators are considered important as indicators of health status. They are-
1. Anthropometric measurements of preschool children, e.g, weight and height, mid-arm circumference.
2. Height (and sometimes weights) of children at school entry.
3. Prevalence of low birth weight (less than 2.5kg).
(Ref: K. Park/25/648-650)
Assessment Methods of Nutritional Status:
Direct Methods of Nutritional Assessment
These are summarized as ABCD
- Anthropometric methods
- Biochemical, laboratory methods
- Clinical examination methods
- Dietary evaluation methods
Indirect Methods of Nutritional Assessment
These include three categories:
- Ecological variables / factors.
- Economic factors e.g. per capita income, population density & social habits
- Vital health statistics particularly infant & under 5 mortality & fertility index
Direct Methods of Nutritional Assessment
A. Anthropometric methods/ Nutritional Anthropometry:
a) Height & weight
- Gomez’ classification (height for age)
- Well come classification (weight for age)
- Waterlow’s classification (weight for Height)
b) Arm circumference
c) Skin fold thickness.
B. Biochemical evaluation:
a) Laboratory tests: Hemoglobin (Hb) estimation, stool examination, Urine examination,
b) Biochemical tests: Serum iron, Serum retinol, Urinary iodine, Serum folate.
C. Clinical examination:
A WHO Export Committee classified signs used in nutritional surveys into 3 categories as those:
a) Not related to nutrition: e.g. alopecia, pyorrhoea, pterygium
b) That needs further investigation: e.g. malar pigmentation, corneal vascularization, geographic tongue.
e) Known to be of value: e.g. angular stomatitis, Bitot’s spots & enlargement of thyroid gland etc.
D. Dietary survey/ Assessment of dietary intake:
A diet survey may be carried out by one of the following methods:
a) Weighment of raw foods
b) Weighment of cooked foods.
c) Oral questionnaire method.
Indirect Methods of Nutritional Assessment
A. Vital & Health statistics:
a) Infant mortality rate
b) Neonatal mortality rate
c) Still birth rate, etc.
B. Ecological studies:
a) Food balance sheet e.g. per capita supply
b) Socio-economic factors e.g. family size
c) Health and educational services e.g. PHC service
d) Conditioning influences e.g. viral infection.
Others
Functional Assessment:
a) Structural integrity,
b) Host defense,
c) Hemostasis,
d) Reproduction,
e) Nerve function,
f) Work capacity.
Signs of Nutritional Imbalance:
| SL | Area of concern | Possible deficiency | Possible excess |
| 1 | Hair:
|
|
|
| 2 | Head and neck
|
|
|
| 3 | Eyes
|
| |
| 4 | Skin
|
|
|
| 5 | Nails
|
| |
| 6 | Mouth
|
| |
| 7 | Abdomen:
|
|
|
| 8 | Heart:
|
|
|
| 9 | Neurologic:
|
|
|
| 10 | Musculoskeletal, extremities:
|
|
|
(Ref: June D Thompson/2nd/300-301)
Poor Clinical Signs of Nutritional Status:
1. General appearance: Restless, apathetic, cachexic.
2. Hair: Stringy, dull brittle, de-pigmented.
3. Neck glands: Thyroid enlarged.
4. Skin, face, neck: Greasy, discolored, scaly.
5. Eyes: Dryness, signs of infection, increased vascularity, glassiness, thickened Conjunctivae
6. Lips: Dry, scaly, swollen, angular lesions (stomatitis)
7. Tongue: Papillary atrophy, smooth appearance, swollen, red, beefy (glossitis)
8. Gums: Marginal redness or swelling, receding, spongy.
9. Teeth: Unfilled cavities, absent teeth, worn surface, mottled, mal-positioned.
10. Skin, general: Rough, dry, scaly, pale, pigmented, irritated.
11. Abdomen: Swollen.
12. Legs, feet: Edema, tender caft, tingling, weakness.
13. Skeleton: Bowlegs, knock-knee, chest deformity at diaphragm, beaded ribs, prominent scapula’s.
14. Weight: Overweight or underweight.
15. Muscles: Flaccid, poor tone, undeveloped, tender.
16. Nervous control: Inattentive, irritable.
17. Gastrointestinal function: Anorexia, indigestion, constipation or airhead.
18. General vitality: Easily fatigued, no energy, falls asleep in school, looks tired, apathetic.
(Ref: June D Thompson/2nd/773-774)
Signs of Good Nutritional Status:
1. General appearance: Alert, responsive.
2. Hair: Shiny, lustrous, healthy scalp,
3. Neck glands: No enlargement.
4. Skin, face, neck: Smooth, slightly moist, good color, reddish pink mucous membranes,
5. Eyes: Bright, clear, no fatigue circles.
6. Lips: Good color, moist.
7. Tongue: Good pink color, surface papillae present, no lesions.
8. Gums: Good pink color, no swelling or bleeding firm.
9. Teeth: Straight, no crowding, well-shaped jaw, clean, no discoloration.
10. Skin, general: Smooth, slightly moist, good color.
11. Abdomen: Flat.
12. Legs, feet: No tenderness, weakness, swelling, good color.
13. Skeleton: No malformation.
14. Weight: Normal for height, age, body builds.
15. Muscles: Well-developed, firm.
16. Nervous control: Good attention span for age, does not cry easily, not irritable or restless.
17. Gastrointestinal function: Good appetite and digestion, normal, regular elimination.
18. General vitality: Endurance, energetic, sleeps well at night, vigorous.
(Ref: June D Thompson/2nd/773-774)
Measurement of Nutritional Anthropometry:
A. Measuring Weight and Height: Formula for approximate average weight and height of normal infants and children
| Weight: | Height |
| At birth = Average-2.5 kg. | At birth: 50 cm |
| 3 to 12 month= {Age (month) +9}+2 | At 1 Year: 75 cm |
| 1-6 years (Age (yr) x 2} +8 | 2-12 years: Age (yr) x 6) +77 cm |
| 7-12 years ((Age x 2)+8} +2 |
B. Measuring Occupito-Frontal Circumference (OFC): It is generally measured in infants and children less than 3 years of age by a flexible, non-stretchable measuring tape.
Procedure of measurement:

Average OFC of a child:
| At birth | At 3 months (cm) | At 6 months (cm) | At 1 year (cm) | At 1 year (cm) |
| 35 | 41 | 44 | 47 | 49 |
C. Measuring the MUAC of children A special tape is used for measuring the MUAC of a child (see Figure 2.3). The tape has three colours, with the red indicating severe acute malnutrition, the yellow indicating moderate acute malnutrition and the green indicating normal nutritional status. Figure 2.4 shows you how to use the tape to measure a child’s MUAC.
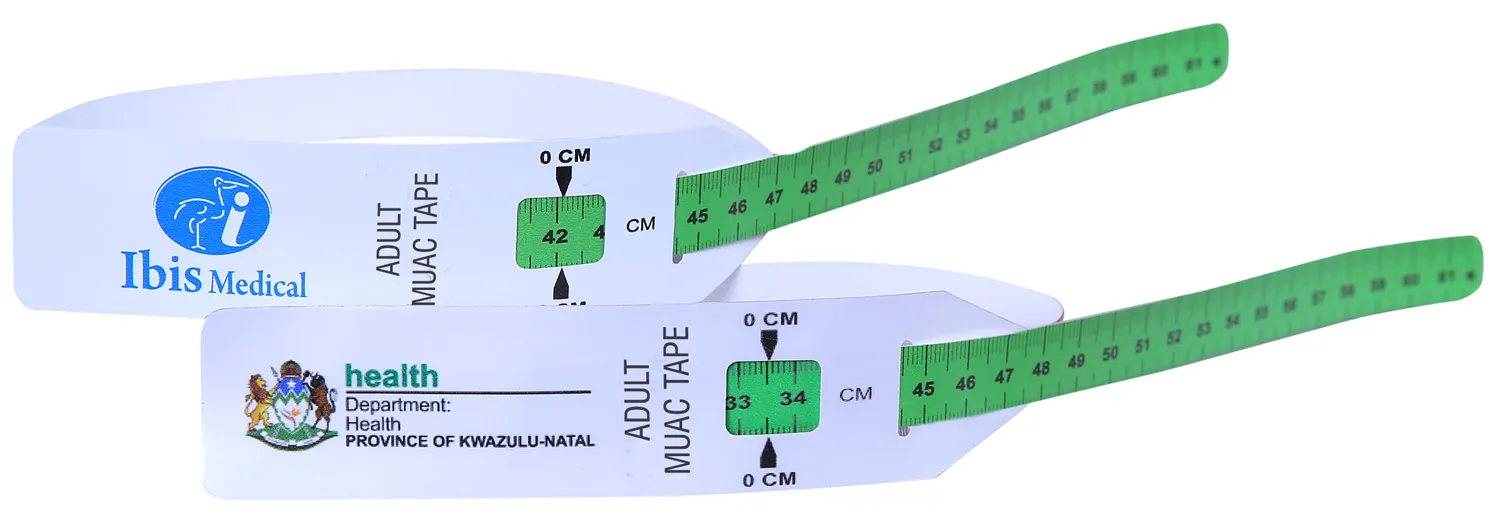
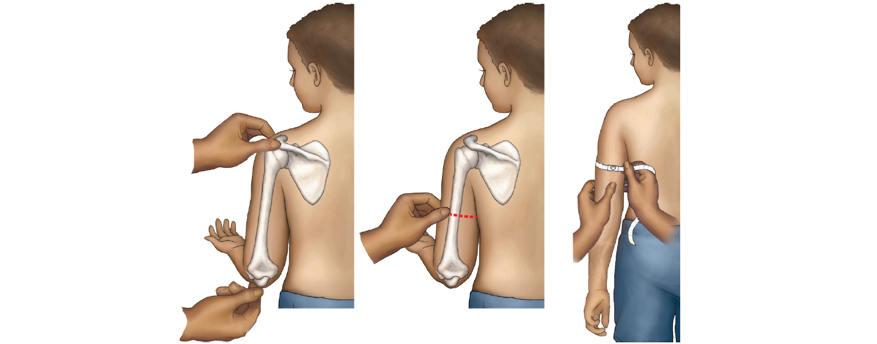
Procedures for measuring MUAC
- Ask the mother to remove any clothing that may cover the child’s left arm. If possible, the child should stand erect and sideways to the measurer.
- Estimate the midpoint of the left upper arm (arrow 6).
- Straighten the child’s arm and wrap the tape around the arm at the midpoint. Make sure the numbers are right side up. Make sure the tape is flat around the skin (arrow 7).
- Inspect the tension of the tape on the child’s arm. Make sure the tape has the proper tension (arrow 7) and is not too tight or too loose (arrows 8 and 9). Repeat any step as necessary.
- When the tape is in the correct position on the arm with correct tension, read the measurement to the nearest 0.1 cm (arrow 10).
- Immediately record the measurement.
| Level of nutrition | MUAC |
| Normal | >13.5 cm (green) |
| Borderline PEM. | 12.5-13.5 cm (yellow) |
| Malnourished. | <12.5 cm (red) |
D. BMI (Body Mass Index): The body mass index (BMI) or Quetelet index is a value derived from the mass (weight) and height of an individual. The BMI is defined as the body mass divided by the square of the body height, and is universally expressed in units of kg/m², resulting from mass in kilograms and height in meters.

Formula:
| Metric BMI Formula | Imperial BMI Formula |
|
|
Example Using Formula
For an adult with height of 180 cm and weight of 75 kg. Our first step needs to be to convert the height into meters (British spelling: metres). As there are 100cm in a meter, we divide our figure by 100. This gives us 1.8m.
Let’s plug those figures into our formula:
BMI = 75 ÷ (1.8×1.8)
BMI = 75 ÷ 3.24
This gives us a BMI figure of 23.15.