Organophosphate Poisoning (OPC poisoning) – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination setup according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Organophosphate Poisoning (OPC poisoning)
Management of OPC poisoning:
A. General management (non-pharmacological approach):
- Immediate ABCD resuscitation, if needed.
- A short & complete history: to confirm about the poisoning & to make the treatment plan.
- Examination of vital signs: BP, pulse, respiratory rate, temperature, urine output, pupil, lung base & heart.
- Contaminated clothing’s should be removed & stored for medico-legal purpose.
- Contaminated skin should be washed by normal saline.
- Gastric suction: By 2% KMn04.
- Catheterization (before giving the 1″ dose of Atropine).
B. Specific management pharmacological approach):
- Atropine (I/V): 0.6-2 mg IV, repeated every 10-25 minutes until full atropinization
- Pralidoxime (I/V): 2 g IV over 4 minutes, repeated 4-6 times daily.
- Diazepam: If convulsion present.
C. Follow up:
- After discharging from the hospital, the patient should be advised to take rest for at least 6 weeks for re-synthesis of the cholinesterase enzyme.
- Patient should be advised to consult with a psychiatrist after discharge.
Atropinization:
The signs produced after atropine administration in OPC poisoning, is called Atropinization. In OPC poisoning I/V Atropine must be continued up to Atropinization & then Atropine should be stopped, otherwise there is chance of atropine toxicity.
- Signs of atropinization:
- Mydriasis.
- Loss of light reflex.
- Tachycardia.
- Dry mouth.
- Dry skin.
- Raised temperature.
- Patient becomes restless.
- Disappearance of crepitation in lungs.
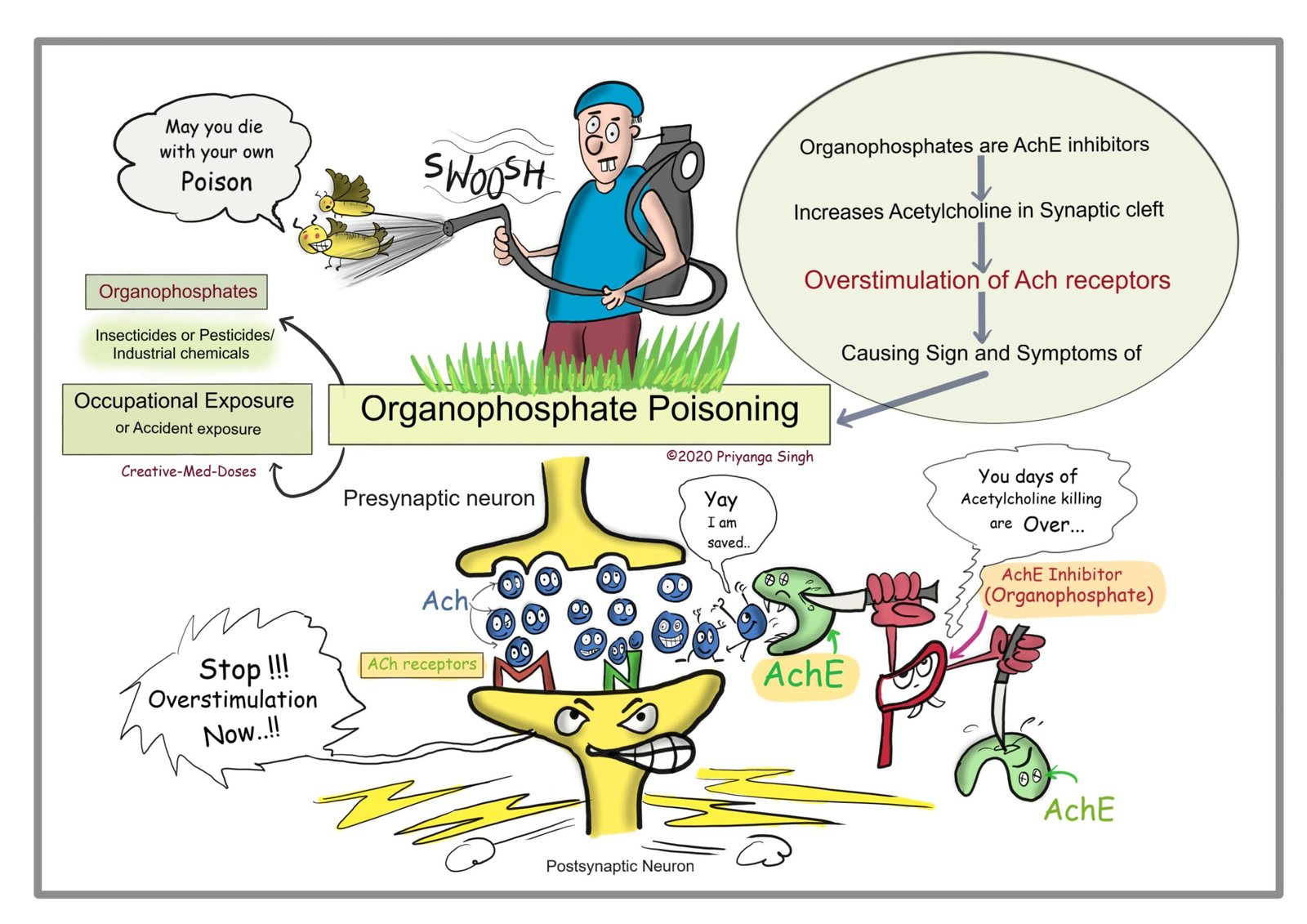
In OPC poisoning:
OPC irreversibly binds with cholinesterase enzyme by a covalent bond and prevents hydrolysis of Acetylcholine (ACh)
⇩
As a result, there is increased concentration of Acetylcholine at cholinoceptors and causes toxic effects of excess acetylcholine (ACh)
⇩
Role of Atropine:
Atropine binds with cholinergic receptors & antagonizes the action of Acetylcholine
⇩
So, Atropine reverses the toxic effects of Acetylcholine excess in OPC poisoning (Competitive reversible antagonism)
⇩
That’s why Atropine is used in OPC poisoning as antidote.
Anti-cholinergic drugs:
Two types
A. Anti-muscarinic drugs: Block muscarinic receptor.
B. Anti-nicotinic drugs: Block nicotinic receptors.
1. Ganglion blocker.
2. NMJ blocker.

Anti-spasmodic/in bronchial asthma
Classification of anti-muscarinic drugs:
A. According to source:
a. Naturally occurring:
1. Atropine.
2. Hyoscine
b. Sythetic & semi-synthetic:
1. Omternary compounds: (Water soluble, do not cross BBB and no CNS effects)
- Propantheline.
- Isopropamide.
2. Tertiary compounds: (Lipid soluble, cross BBB & cause CNS effects)
- Tropicamide.
- Cyclopentolate.
- Oxybutynin.
- Homatropine.
- Pirenzepine.
B. According to clinical use/ therapeutic use/indication:
a. Mydriatics/ophthalmic anti-muscarinic;
1. Atropine.
2. Scopolamine.
3. Homatropine.
4. Cyclopentolate.
5. Tropicamide.
b. In CVS disorder:
1. Atropine.
c. As bronchodilator/in respiratory disorder:
1. Ipratropium bromide.
2. Tiotropium.
d. Anti-parkinsonism:
1. Procyclidine.
2. Benztropine mesylate.
3. Biperidine.
4. Orphenadrine.
5. Trihexyphenidyl.
e. In anaesthetic pre-medication;
1. Atropine.
2. Scopolamine.
f. Anti-secretory;
1. Pirenzepine.
2. Telenzepine.
g. Anti-spasmodic/spasmolytic:
1. Propantheline.
2. Dicyclomine.
3. H-N Butyl bromide.
4.Tiemonium methylsulphate.
h. Anti-motion sickness:
1. Scopolamine,
2. Hyoscine.
i. In urinary disease:
1. Oxybutynin.
2 Trospium.
3. Tolterodin.
4. Fesoterodine.
5. Darifenacin.
6. Solifenacin.
7. Propiverine
Indication of anti-muscarinic drugs:
A. As antidote: In the treatment of OPC poisoning (most important & commonest use of Atropine).
B. Respiratory disorders: (As bronchodilator)
1. Bronchial asthma.
2. COPD.
C. CNS disorders:
1. Parkinson’s disease.
2. Motion sickness.
D. Ophthalmologic disorder:
1. In uveitis & iritis: To prevent synechia (adhesion) formation (Scopolamine).
2. Accurate measurement of refractive error in non-cooperative patients (young children) for ciliary paralysis.
3. Ophthalmologic examination of retina for mydriasis.
E. CVS disorders;
1. Vasovagal attack.
2. Initial treatment of MI
F. Anaesthetic use; Atropine / Glycopyrrolate are used,
1. In case of reversal from general anaesthesia. Atropine/Glycopyrrolate are used to antagonize the CVS action (bradycardia, hypotension) of Neostigmine.
2. In case of anaesthetic premedication for bronchodilatation & to reduce bronchial secretion (not-used routinely).
G. GIT disorder, Peptic ulcer disease (PUD). H. Spasmodic abdominal visceral pain.
I. Traveler’s diarrhoea
J. Minor inflammatory bladder disorder to relief urinary urgency.
[Ref-katzung/14/130]
Indications of Atropine:
A. OPC poisoning.
B. Ophthalmic use:
1. Uveitis & iritis.
2. Accurate measurement of refractive error in non-cooperative patients.
3. Ophthalmologic examination of retina for mydriasis.
C. Anesthetic use:
1. Anaesthetic premedication for Broncho dilatation & to reduce bronchial secretion.
2. During reversal from general anaesthesia along with Neostigmine.
D. in CVS disorders:
1. Vasovagal attack.
2. Sinus bradycardia.
3. Initial treatment of MI.
Contraindications of Atropine & other anti-muscarinic drugs:
1. Old MI.
2. Glaucoma (except glaucoma secondary to uveitis).
3. BPH & old age male.
4. Patients with psychosis & schizophrenia