Parenteral Nutrition (PN) – This book covers the entire syllabus of “Nutrition and Dietetics” prescribed by BNMC-for all Diploma in Nursing Science and Midwifery students. We tried to accommodate latest information and topics. This book is examination friendly setup according to the teachers’ lectures and examination’s questions.
At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourished. The unique way of presentation may make your reading of the book a pleasurable experience.

Parenteral Nutrition (PN)
It is defined as the intravenous provision of all nutritional requirements, without the use of the gastrointestinal tract.
Or,
Parenteral nutrition (PN) is the feeding of specialist nutritional products to a person intravenously, bypassing the usual process of eating and digestion.
Or,
Parenteral nutrition (PN) is intravenous administration of nutrition, which may include protein, carbohydrate, fat, minerals and electrolytes, vitamins and other trace elements for patients who cannot eat or absorb enough food through tube feeding formula or by mouth to maintain good nutrition status.
Types of Parenteral Nutrition (PN):
Partial Parenteral Nutrition
- Supplies only part of daily nutritional requirements, supplementing oral intake
- Dextrose or amino acids solutions
Total Parenteral Nutrition
- Supplies all daily nutritional requirements
- TPN solutions are highly concentration- central vein is used
Partial Parenteral Nutrition (PPN)
Definition of Partial Parenteral Nutrition (PPN):
A solution, containing some essential nutrients, is injected into a vein to supplement other means of nutrition, usually a partially normal diet of food.
Or,
Intravenous administration of nutrients to patients whose nutritional requirements cannot be fully met via the enteral route. An amino acid-dextrose solution (usually 10%) and a lipid emulsion (10% to 20%) are delivered into a peripheral vein through a cannula or catheter.
Total Parenteral Nutrition (TPN)
Definition of Total parenteral nutrition (TPN):
Total parenteral nutrition (TPN) is defined as the provision of all nutritional requirements by means of the intravenous route and without the use of the gastrointestinal tract.
Or,
TPN is a way of supplying all the nutritional needs of the body by bypassing the digestive system and dripping nutrient solution directly into a vein.
Or,
TPN is defined as provision of all nutrients essential for normal homeostasis and growth in the required amounts through parenteral route that is directly in the vein.
Indications of Total Parenteral Nutrition (TPN):
- Proximal intestinal fistula.
- Inflammatory bowel disease (especially in the pre-operative period).
- Large intestinal resection (particularly if < 100cm of small bowel).
- Ileus.
- Severe pancreatitis.
Contraindication of Parenteral Feeding:
- Cardiac failure.
- Severe liver disease.
- Disorders of fat metabolism.
- Uncontrolled diabetes.
- Shock.
- Severe blood dyscrasias.
Complications of Parenteral Nutrition:
Related to nutrient deficiency:
- Hypoglycaemia.
- Hypocalcaemia.
- Hypophosphataemia.
- Hypomagnesaemia (refeeding syndrome).
- Chronic deficiency syndromes (essential fatty acids, zinc, mineral and trace elements).
Related to overfeeding:
- Excess glucose: Hyperglycaemia, hyperosmolar dehydration, hepatic steatosis, hypercapnia, increased sympathetic activity, fluid retention, and electrolyte abnormalities.
- Excess fat: Hypercholesterolaemia and formation lipoprotein X, hypertriglyceridaemia, hypersensitivity reactions.
- Excess amino acids: Hyperchloraemic metabolic acidosis, hyperkalaemia, minoacidemia, uraemia.
Related to sepsis:
- Catheter-related sepsis.
- Possible increased predisposition to systemic sepsis.
Related to line:
- On insertion: Pneumothorax, damage to adjacent artery, air embolism, thoracic duct damage, cardiac perforation or tamponade, plural effusion, hydromediastinum.
- Long-term use: Occlusion, venous thrombosis.
Care of Clients Receiving Parenteral Nutrition:
- Pulse,respiration, blood pressure and temperature are checked minimum of four times a day.
- Intake and output record is maintained daily.
- Weight is checked on alternate days.
- Urine sugar is checked every 6 hours.
- Blood sugar, Urea, serum electrolytes are checked until patient is stable and then twice a week depending on patient’s condition.
- Calcium and phosphate are checked twice a week.
- Hemoglobin, prothrombin time, live function tests and total iron binding capacity are checked once a week.
Difference Between partial parenteral nutrition (PPN) & Total parenteral nutrition (TPN):
| Partial Parenteral Nutrition (PPN) | Total Parenteral Nutrition (TPN) |
| PPN stands for Partial Parenteral Nutrition | TPN stands for Total Parenteral Nutrition |
| The Partial parenteral nutrition is a kind of partial nutrition given to a patient, whereby he or she can still take nutrition from other sources. | The total parenteral nutrition is given in higher concentration, and it is administered through the larger veins, usually in the neck or chest. |
| The Partial parenteral nutrition is given in a lesser concentration, and it is usually administered through in the smaller veins. | The TPN contains minerals, glucose, and even electrolytes, which make it more caustic than PPN |
Advantages of Parenteral Nutrition:
- Extensive return to oral or internal nutrition is recommended as soon as possible.
- Doing so reduces the risk for sepsis, decreases cost and prevent wasting and deterioration of the GI tracts.
- Prevention of potential complications associated with total parenteral rut requires vigilance and careful monitoring.
- Can provide total nutritional support for longer period of time.
- Parenteral nutrition of lower percent of infections.
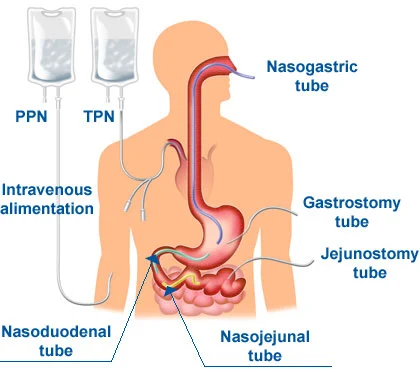
Methods of Nutritional Supplements:
1. Enteral nutrition (Predominant):
- By mouth.
- By nasogastric tube.
- By tube enterostomy.
- By gastrostomy.
- By jejunostomy.
2. Parenteral nutrition (less common): Intravenous feeding.
Indication of Nutritional Support:
1. Preoperative nutritional depletion.
2. Postoperative complications.
- Ileus more than 4 days.
- Sepsis.
- Fistula formation.
3. Massive bowel resection.
4. Intestinal fistula.
5. Management of-
- Pancreatitis.
- Malabsorption syndrome.
- Ulcerative colitis.
- Radiation enteritis.
- Pyloric stenosis.
6. Anorexia nervosa.
7. Intractable vomiting.
8. Maxillo-facial trauma.
9. Traumatic coma.
10. Multiple traumas.
11. Burns.
12. Malignant diseases.
13. Renal failure.
14. Liver disease.
15. Cardiac valve disease
Methods of Enteral Feeding:
1. By mouth.
2. By nasogastric tube.
3. By tube enterostomy: it is the operative placement of a tube or catheter into the GIT. It is indicated when the passage of a fine-bore NG tube is not possible or when more than 4 weeks of enteral feeding is anticipated.
4. By gastrostomy: There are two long-term types of gastrostomy-
- Stamm temporary gastrostomy.
- Janeway temporary gastrostomy.
5. By jejunostomy: There are two types of feeding jejunostomy-
- Witzel jejunostomy.
- Needle jejunostomy
Indications of Enteral Feeding:
- Protein-energy malnutrition with inadequate oral intake.
- Dysphagia, except for fluids.
- Major trauma (including surgery) when return to required dietary intake is prolonged.
- Inflammatory bowel disease.
- Distal, low-output (<200ml) enterocutaneous fistulas.
- To enhance adaptation after massive enterectomy.
Contraindications:
- Small bowel obstruction or ileus.
- Severe diarrhoea.
- Proximal small intestinal fistulas.
- Severe pancreatitis.

Complications:
Related to feeding tube:
- Malposition.
- Dislodgement.
- Blockage.
- Breakage/leakage.
- Local complication e.g. erosion of skin / mucosa.
Gastrointestinal:
- Diarrhoea.
- Bloating, nausea, vomiting.
- Abdominal cramps.
- Aspiration.
- Constipation.
Metabolic/biochemical:
- Electrolyte disorders.
- Vitamin, mineral, trace element deficiencies.
- Drug interactions.
Infective:
- Exogenous (handling contamination)
- Endogenous (patient)