Parkinsons disease (PD) – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Parkinsons disease (PD)
Definition of Parkinsons Disease:
Parkinsons disease (PD) is a long-term degenerative disorder of the central nervous system that mainly affects the motor system.
Or,
Parkinsons disease is a progressive nervous system disorder that affects movement. Symptoms start gradually, sometimes starting with a barely noticeable tremor in just one hand. Tremors are common, but the disorder also commonly causes stiffness or slowing of movement.
Parkinsonian or akinetic-rigid syndromes: (affecting the basal ganglia)
It is characterized by combinations of –
- Slowness of movement (bradykinesia)
- Increased tone (rigidity),
- Tremor and loss of postural reflexes.
Pathogenesis Parkinsons disease:
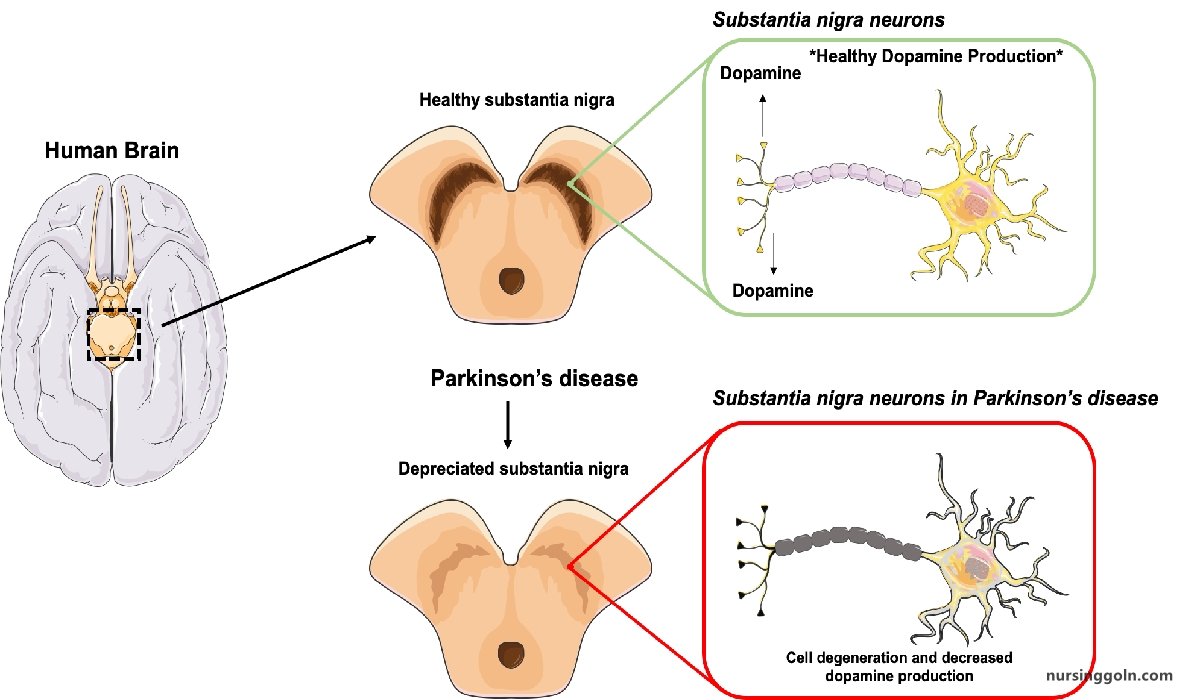
- Imbalance between cholinergic & dopaminergic influences on the basal ganglia,
- Reduced high conc. of dopamine in the basal ganglia
Pathophysiology:
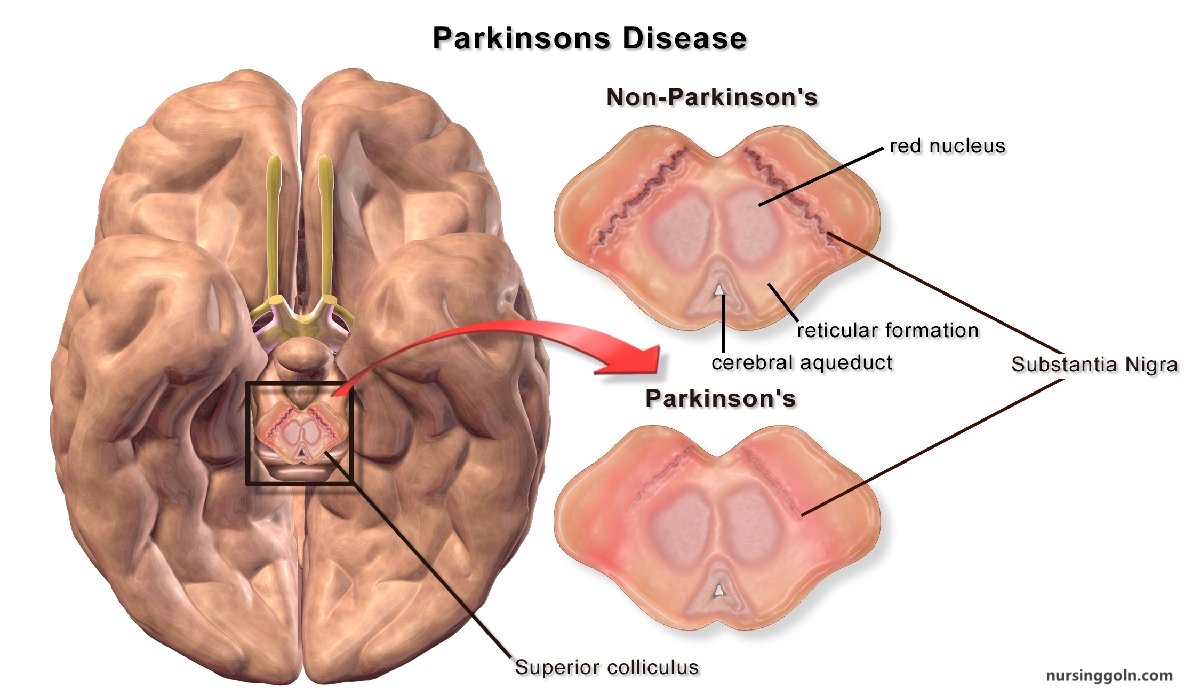
- Depletion of the pigmented dopaminergic neurons in the substantia nigra, hyaline inclusions in nigral cells, atrophic changes in the substantia nigra and depletion of neurons in the locus coeruleus.
- Reduced dopaminergic output from the substantia nigra to the globus pallidus leads to reduced inhibitory effects on the subthalamic nucleus, neurons of which become more active than usual in inhibiting activation of the cortex. This in turn results in bradykinesia.
Causes of Parkinsonism:
➤ Idiopathic: Idiopathic Parkinsons disease (Most common)
➤ Post-encephalitie: (after viral infection)
- Encephalitis/Japanese B encephalitis.
- HIV infection/SSPE
➤ Drugs: Phenothiaziue, Butyrophenones, Methyldopa, Reserpine, Cisapride, metoclorpromide etc.
➤ Neurosyphilis.
➤ Poisoning: CO, Mn, MPTP (1-Methyl 4 phenyl 1,2,3,6 tetrahydropyridine)
➤ Truma:
- Punch drunk syndrome
- Repeated head injury
➤ Neoplastic:
- Cerebral tumour (involving basal ganglia)
➤ Others:
- Wilson’s disease.
- Huntington’s disease
Management of Parkinsons Disease:
Clinical features:
Non-specific symptoms (Initially):
- Tiredness
- Aching limbs
- Mental slowness
- Depression and
- Small handwriting (micrographia).
Specifics symptoms:
- Bradykinesia
- Rigitidy causing stiffness & flexed posture
- Always unilateral presentation & gradual bilateral involvement is the rule
- Difficulty with rapid fine movements such as difficulty with fastening buttons, shaving or writing
- Speech becomes softer & indistinct in advance diseases
Physical abnormalities:
| Cardinal feature of Parkinsons diseases: i. Resting tremor. ii. Rigidity iii. Bradykinesia iv. Postural imbalance. |
General:
- Expressionless face
- Greasy skin
- Soft, rapid, indistinct speech
- Flexed posture
- Impaired postural reflexes.
Gait:
- Slow to start walking
- Shortened stride
- Rapid, small steps, tendency to run (festination)
- Reduced arm swing
- Impaired balance on turning.
Tremor:
a. Resting 4-6 Hz:
- Usually first in fingers/thumb
- Coarse, complex movements, flexion/extension of fingers
- Abduction/adduction of thumb
- Supination/pronation of forearm
- May affect arms, legs, feet, jaw, tongue
- Intermittent, present at rest and when distracted
- Diminished on action.
b. Postural 8-10 Hz
- Less obvious, faster, finer amplitude
- Present on action or posture, persists with movement
Rigidity:
- Cogwheel type, mostly upper limbs
- Plastic (leadpipe) type, mostly legs.
Bradykinesia
- Slowness in initiating or repeating movements
- Impaired fine movements, especially of fingers
So The classical syndrome consists of (Clinical triad)
- Tremor
- Rigidity and
- Bradykinesia
Investigations
- Diagnosis is usually made in clinical grounds.
- Investigations are done for specific cases to exclude other causes
i. Serological test for syphilis.
ii. CT scan/MRI of brain when –
- Age < 50 yr
- Pyramidal sings, cerebellar signs or autonomic involvement or the Dx is in doubt.
iii. In younger pt- Screening for Wilson’s disease
- S. copper
- S. ceruloplasmin
- 24 hrs urinary copper.
- Liver function test.
- Slit lamp exam of eye for K-F ring.
Treatment of Parkinsons Disease:
i. Any identifiable cause should be treated.
ii. Drug therapy:
a. Dopaminergic drugs: Levodopa combined with a peripheral-acting dopa-317 decarboxylase inhibitor (Carbidopa) provides the of treatment in Parkinsons disease
- Levodopa is particularly effective at improving bradykinesia and rigidity.
- The initial dose is 50 mg 8- or 12-hourly, increased if necessary.
b. Anti-cholinergic agents: improving tremor and rigidity
- Benzhexol (1-4 mg -8 hrly) or orphenadrine (50-100 mg 8 hrly)
c. Drugs which release dopamine from stores & inhibit reuptake:
- Amantidine 100 mg 8 or 12 hrly.
d. Selective inhibitors of dopamine metabolism:
- MAO inhibitors: Selezeline 5-10 mg in morning. (Inhibits metabolism of dopaniine)
- COMT (catechol-O-methyl-transferase) inhibitors: Entacapone (200 mg with each dose of levodopa)
e. Dopamine agonists:
- Bromocriptine I mg initially, increases to 2.5 mg 8 hrly & then upto 30 mg/day
- Others: lisuride, pergolide, cabergoline, ropinirole and pramipexole
iii. Surgery:
- Stereotactic thalamotomy- can be used to treat tremor
- Pallidotomy- in case of drug induced dyskinesia.
- Implantation of foetal mid-bain/ adrenal tissue into the basal ganglia- to enhance dopaminergic activity.
iv. Physiotherapy & speech therapy.
Nursing Management of Parkinsons Disease:
Nursing Assessment
- Bradykinesia, abnormal slowness of movement, and sluggishness of physical and mental responses.
- Akinesia
- Monotonous speech
- Handwriting that becomes progressively smaller
- Tremors in hands and fingers at rest (pill rolling)
- Tremors increasing when fatigued and decreasing with purposeful activity or sleep.
- Rigidity with jerky interrupted movements
- Restlessness and pacing
- Blank facial expression-mask-like facies
- Drooling
- Difficulty swallowing and speaking
- Loss of coordination and balance.
- Shuffling steps, stooped position, and propulsive gait.
Primary Nursing Diagnosis
- Self-care deficit related to rigidity and tremors
Nursing Interventions
- Assess neurological status.
- Assess ability to swallow and chew.
- Provide high-calorie, high-protien, high-fiber soft diet with small, frequent feedings.
- Increase fluid intake to 2000 mL/day.
- Monitor for constipation.
- Promote independence along with safety measures.
- Avoid rushing the client with activities.
- Assist with ambulation and provide assistive devices.
- Instruct client to rock back and forth to initiate movement.
- Instruct the client to wear low-heeled shoes.
- Encourage the client to lift feet when walking and avoid prolonged sitting.
- Provide a firm mattress, and position the client prone, without a pillow, to facilitate proper posture.
- Instruct in proper posture by teaching the client to hold the hands behind the back to keep the spine and neck erect.
- Promote physical therapy and rehabilitation.
- Administer anticholinergic medications as prescribed to treat tremors and rigidity and to inhibit the action of acetylcholine.
- Administer antiparkinsonian medications to increase the level of dopamine in the CNS.
- Instruct the client to avoid foods high in vitamin B6 because they block the effects of antiparkinsonian medications.
- Instruct the client to avoid monoamine oxidase inhibitors because they will precipitate hypertensive crisis.
Documentation Guidelines
- Ability to ambulate, perform the activities of daily living, progress in an exercise program
- Use of verbal and nonverbal communication
- Statements about body image and self-esteem
- Discomfort during activity
Discharge and Home Healthcare Guidelines
- Be sure the patient or caregiver understands all medications, including the dosage, route, action, and adverse reactions. Avoid the use of alcohol, reserpine, pyridoxine, and phenothiazine while taking levodopa.
- In general, recommend massage and relaxation techniques, and reinforce exercises recommended by the physical therapist. Several techniques facilitate mobility and enhance safety in Parkinson’s disease patients.
- Instruct the patient to try the following strategies:
➤ To assist in maintaining balance, concentrate on taking larger steps with feet apart, keeping back straight and swinging the arms;
➤ To overcome akinesia, tape the “frozen” leg to initiate movement;
➤To reduce tremors, hold objects (coins, keys, or purse) in the hand;
➤ To obtain partial control of tremors when seated, grasp chair arms;
➤To reduce rigidity before exercise, take a warm bath;
➤ To initiate movement, rock back and forth;
➤ To prevent spine flexion, periodically lie prone and avoid using a neck pillow; and
➤ Teach the patient to eliminate loose carpeting, install grab bars, and elevate the toilet seat. Use of chair lifts can also be beneficial.