Pleural Effusion – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Pleural Effusion
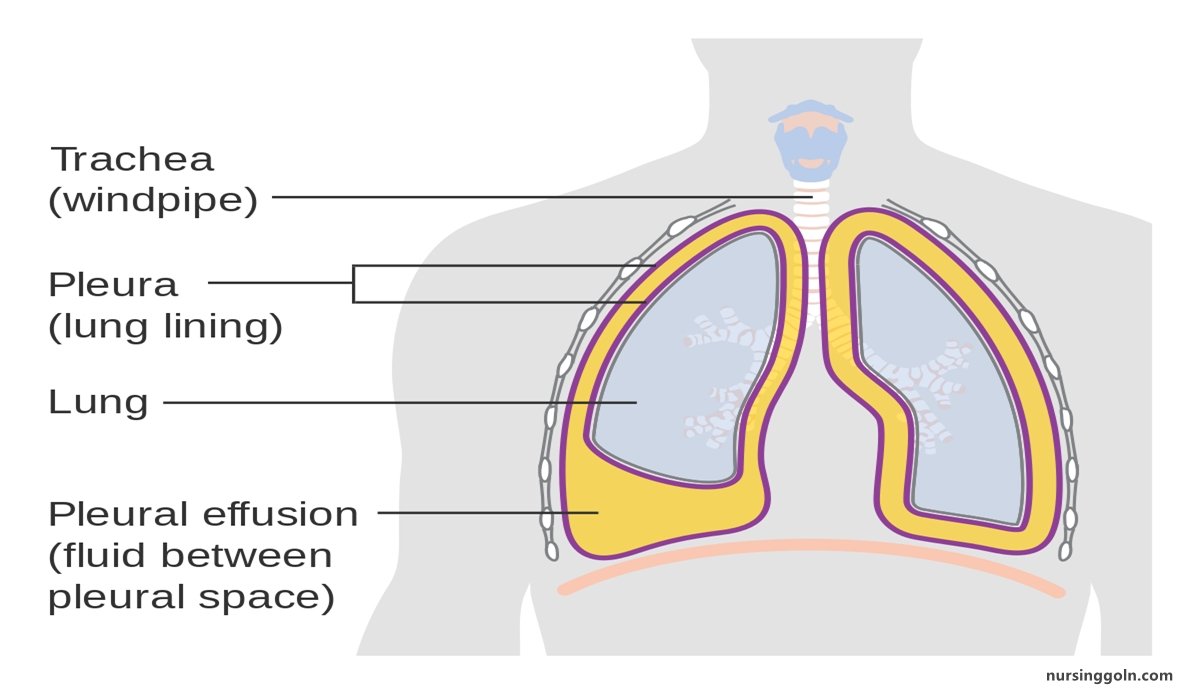
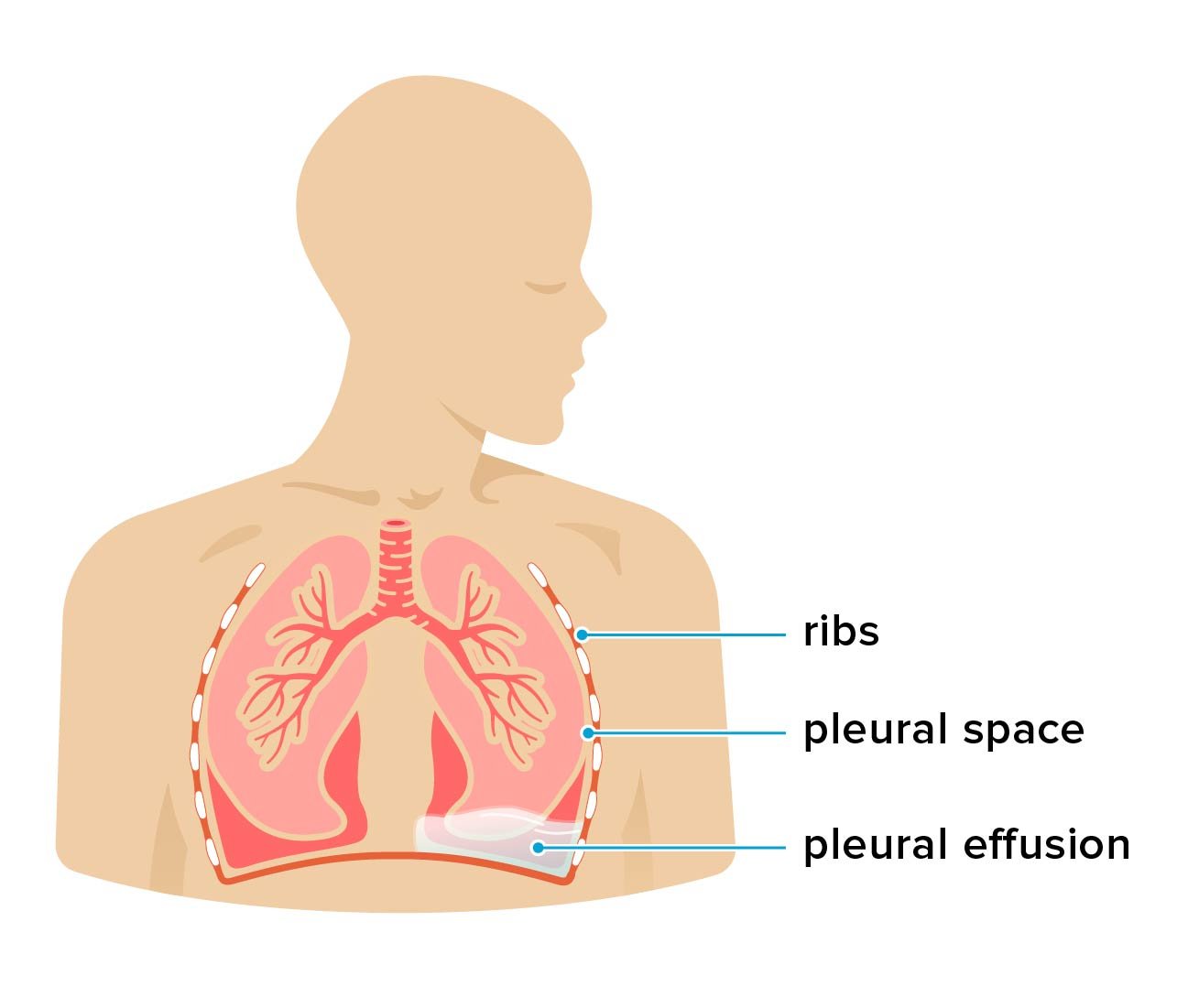
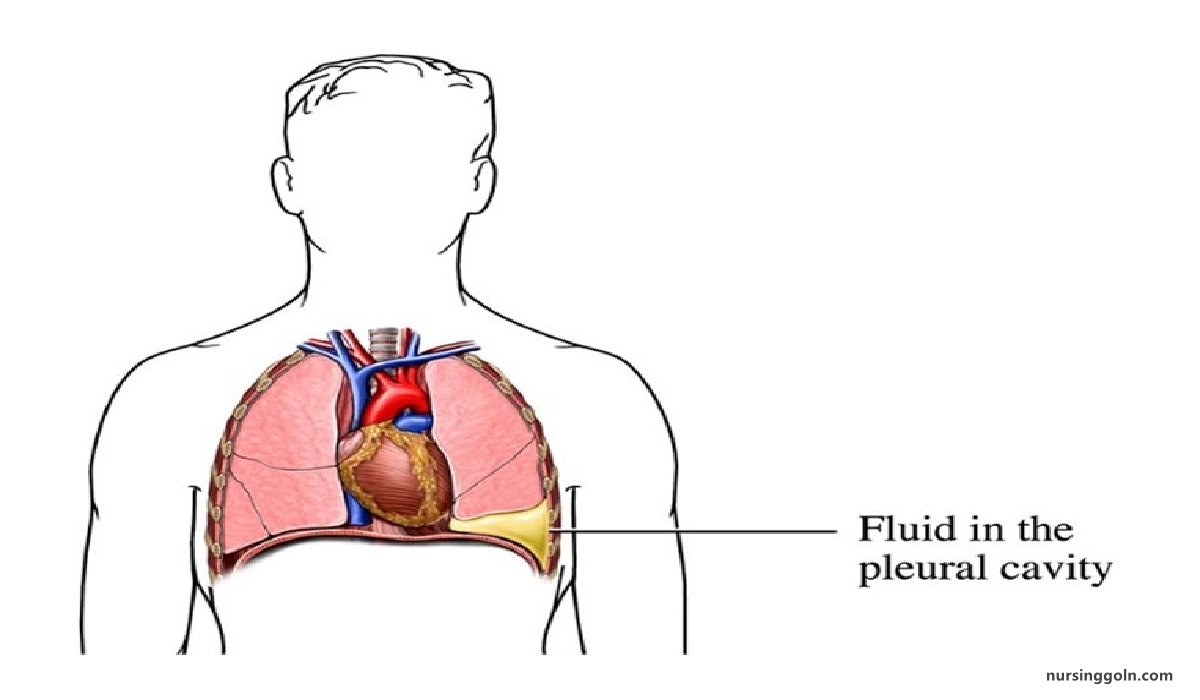
Pleural effusion, also called “water on the lung,” is an excessive buildup of fluid in the space between your lungs and chest cavity. Thin membranes, called pleura, cover the outside of the lungs and the inside of the chest cavity. There’s always a small amount of liquid within this lining to help lubricate the lungs as they expand within the chest during breathing.
Certain medical conditions can cause a pleural effusion
Pleural effusions are common, with approximately 1.5 million cases diagnosed in the United States every year, according to the American Thoracic Society. It is a serious condition associated with an increased risk of death. One study has shown that 15 percent of hospitalized people diagnosed with pleural effusions die within 30 days.
Definition of Pleural Effusion
The accumulation of serous fluid within the pleural space is termed pleural effusion. Accumulations of frank pus (empyema) or blood (haemothorax)
Definition of Pleurisy
Pleurisy is inflammation of the tissue (pleura) between the lungs and ribcage.
Causes of Pleural Effusion
A. Common causes
a) Pneumonia (‘para-pneumonic effusion’).
b) Tuberculosis.
e) Pulmonary infarction.
d) Malignant disease.
e) Cardiac failure.
f) Subdiaphragmatic disorders (subphrenic abscess, pancreatitis etc.)
B. Uncommon causes
a) Hypoproteinaemia (nephrotic syndrome, liver failure, malnutrition)
b) Connective tissue diseases (particularly systemic lupus erythematosus and rheumatoid arthritis)
c) Acute rheumatic fever.
d) Post-myocardial infarction syndrome
e) Meigs’ syndrome (ovarian tumour plus pleural effusion & ascites
f) Myxoedema
g) Uraemia,
h) Asbestos-related benign pleural effusion.
C. 4 important causes of pleural effusion
a) Tuberculosis
b) Pneumonia (para-pneumonic effusion’)
c) Malignant disease (Bronchial carcinoma)
d) Pulmonary infarction
(Ref by- Kumar & Clark clinical Medicine 8+Harrison’s internal medicine/18 +Davidson’s Medicine 661/22)
Types of Pleural Effusion
According to the nature of fluid
a) Exudative: Increased micro vascular pressure due to disease of the pleural surface itself, or injury in the adjacent lung
Examples
a) Tuberculosis
b) Pneumonia
e) Bronchogenic carcinoma
d) Lymphoma
e) Pulmonary infarction
f) Dressler syndrome
b) Transudative: Pleural fluid accumulates as a result of either increased hydrostatic pressure or decreased osmotic pressure.
Examples
a) Hypoproteinaemia
- Cirrhosis of liver (Liver failure)
- Nephritic syndrome (Renal failure)
- Malnutrition
b) Cardiac failure
c) Meig’s syndrome
d) Dressler’s syndrome
According to the site
A. Bilateral
a) All causes of transudative pleural effusion
b) Rheumatoid arthritis
c) SLE
d) Lymphoma
B. Unilateral
a) Right sided:
- Tuberculosis
- Pneumonia
- Bronchogenic carcinoma
- Pulmonary infarction
- Meig’s syndrome
- Liver abscess
b) Left sided
- Tuberculosis
- Pneumonia
- Bronchogenic carcinoma
- Pulmonary infarction
- Dressler’s syndrome
- Acute pancreatitis
- Rheumatoid arthritis
- Oesophageal rupture.
(Ref by- Kumar & Clark clinical Medicine 885/8+Harrison’s internal medicine/18)
Management of Pleural Effusion
B. Clinical Feature
A. Symptoms of pleural effusion.
a) Long history of evening rise of temperature, night sweating, hemoptysis, cough, anorexia-
-highly suggestive of pulmonary TB.
b) Short history of high grade fever, cough with yellowish sputum, chest pain.
- Fever may be associated with rigor.
- Cough is initially dry, later on there is expectoration, rusty sputum.
- Localized chest pain increase on deep inspiration.
All these features are suggestive of pneumonia.
c) Old man with cough, chest pain, hemoptysis, recurrent attack of pneumonia, H/o smoking for long time these feature are suggestive of bronchogenic carcinoma.
d) Pt. presents central chest pain, dyspnoea, apprehensive, H/O operation or prolonged immobilization – these features are suggestive of pulmonary thrombo-emboliom leading to pulmonary infarction.
C. Signs/on physical exam
a) G/E
a) Weight loss in TB, Bronchogenic Ca (BC).
b) Clubbing in BC.
c) Odema
d) Thyroid gland-Hypothyroidism
e) Palpable lymph node- for lymphoma, metastasis.
f) Temperature:
- Low grade fever-TB, Bronchogenic carcinoma.
- High grade fever – pneumonia, acute pancreatitis, liver abscess
b) On R/E
a) Inspection
- Respiratory rate is increased.
- Chest wall movement is restricted on affected side.
b) Palpation
- Trachea is shifted to the opposite side.
- Apex beat is shifted to the opposite side.
- Chest wall movemenf is restricted on the affected side.
- Chest wall expansion is reduced.
- Vocal fremitus is diminished or absent.
c) Percussion
- Stony dull in the affected side.
d) Auscultation
- Breath sound is reduced or absent.
- Vocal resonance is reduced or absent.
D. Investigations
Vocal resonance is reduced or absent.
a) Chest x-ray
b) CBC
- Hb-Decreased.
- TC/DC-Neutrophilic leukocytosis in Pneumonia, acute pancreatitis, Liver abscess & lymphocytosis in TB.
- ESR – High in TB, Bronchogenic carcinoma
c) Aspiration of fluid for analysis
d) MT.-positive in T.B.
e) Pleural biopsy by Abraham’s or Cope’s Needle (positive in 80% cases in TB and 40% in bronchial carcinoma).
f) If cough-sputum for Gram staining, C/S, AFB and mycobacterial C/S, malignant cells
g) Others
- CT scan
- USG
- Bronchoscopy & biopsy for malignancy.
- Amylase of pleural fluid high in acute pancreatitis & oesophageal rupture
- Cholesterol, LDH and rheumatoid factor of pleural fluid for rheumatoid arthritis
E. Treatment
a) Symptomatic Management
- Aspiration of pleural fluid not more than 1.5 L at a time at the post. scapular line at the 7/8 intercostals space.
- Antipyretic if fever present.
- Antibiotic if necessary
b) Management is according to underlying causes / Specefic causes
For example-
Tuberculous pleural effusion:
- Anti-TB chemotherapy + Addition of prednisolone daily by mouth for 4-6 weeks.
- Aspiration of fluid initially if the effusion is large & causing breathlessness.
c) Malignant effusion
- Draining of pleural fluid by intercostals drain tube.
- Pleurodesis by Talc & Tetracyclin.
(Ref by- Kumar & Clark clinical Medicine/7th+Harrison’s internal medicine/17th + short case Abdullah Sir/4th+Davidson’s Medicine 661-62/22)