Premature Rupture Of Membrane (PROM) – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Premature Rupture Of Membrane (PROM)
Premature rupture of membrane (PROM):
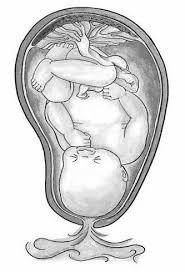
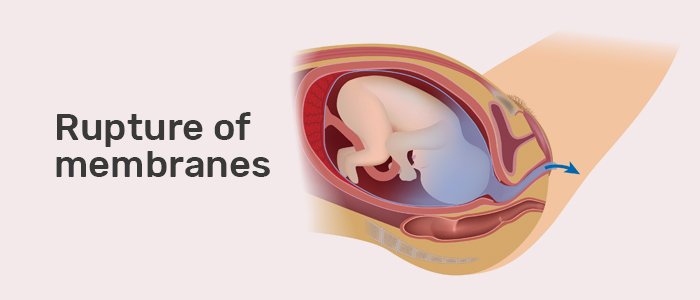
Premature rupture of membranes (PROM), or pre-labor rupture of membranes, is a condition that can occur in pregnancy. It is defined as rupture of membranes (breakage of the amniotic sac), commonly called breaking of the mother’s water(s), more than 1 hour before the onset of labor.
Or
Premature rupture of membranes is the rupture of membranes during pregnancy before 37 weeks’ gestation.
Causes of premature rupture of membrane (PROM):
➤ Poor nutrition or dehydration.
➤ Smoking during pregnancy.
➤ An infection in the cervix, uterus or vagina.
➤ Prior cervical surgery or biopsy.
➤ Prior preterm PROM.
➤ Prior preterm labor and delivery fetuses or too much amniotic fluid (hydramnios).
➤ An infection in the vagina or uterus (chorioamnionitis, Group B strep, bacterial vaginosis, urinary tract infections).
➤ Previous cervical surgery, including cone biopsies or cerclage.
➤ Overstretching of the uterus and amniotic sac, which sometimes occurs with multiple.
Risk factors of premature rupture of membrane (PROM):
➤ Maternal sepsis
➤ Cord prolapse
➤ Malpresentation of the baby.
➤ Low socioeconomic status.
➤ Smoking
➤Poor nutrition or dehydration.
➤ Polyhydramnios.
➤ Prior cervical surgery or biopsy.
➤ Prior preterm PROM.
Signs and symptoms of premature rupture of membrane (PROM):
➤ Fluid leaking from the vagina.
➤ Sweet odor may be meconium stained,
➤ Contractions of the uterus.
➤ tachycardia
➤ Increased temperature and heart rate (in the mother).
➤ Tenderness of the uterus.
➤ Foul-smelling vaginal discharge.
➤ Increased white blood cell count or a change in the pattern of white blood cell type.
➤ An increase in the baby’s heart rate.
Injuries that are associated with PROM and PPROM:
➤ Prolapsed umbilical cord.
➤ Infection.
➤ Malpresentation.
➤ Premature birth.
➤ Hypoxic ischemic encephalopathy (HIE).
➤ Death of the fetus may occur in the worst case scenarios of PROM.
Diagnosis of premature rupture of membrane (PROM):
➤ Vaginal pooling of amniotic fluid or visible vernix or meconium.
Evaluation of vaginal fluid showing ferning or alkalinity (blue color) on Nitrazine paper.
➤ Sometimes ultrasound-guided amniocentesis with dye for confirmation.
➤ Fern test
➤ Ultrasound examination shows oligohydramnios.
Investigations needed for premature rupture of membrane (PROM):
Do not routinely perform a digital vaginal examination, as this will increase the risk of ascending infection,
➤ Diagnosis of rupture of membranes:
✔Actually seeing amniotic fluid draining from the cervix and pooling in the vagina after the woman has been lying down for 30 minutes is the most accurate test. Sterile speculum examination: check for liquor and for the umbilical cord,
✔ Testing for insulin-like growth factor binding protein-1 or placental alpha- microglobulin-1 may aid diagnosis but results should not be considered in isolation.
✔ Nitrazine testing is no longer recommended, as urine, semen and other contaminants may give a false positive test result.
✔ Regular pad checks.
✔The Vision Amniotic Leak Detector (ALD) is a non-invasive diagnostic liner that can be attached to underwear. Its use in the community to prevent unnecessary and inconvenient admissions to hospital is encouraged.
✔ Ultrasound may be useful to check for gestation and liquor volume.
➤ Temperature monitoring at least 12-hourly for ascending infection:
✔ High vaginal swab.
✔If infection is suspected, check FBC (for WCC), CRP, MSU and blood cultures; start appropriate antibiotic treatment if tests, along with clinical signs, confirm intrauterine infection.
Fetal monitoring.
[NB: regular weekly vaginal swabs and/or maternal blood tests (e.g. CRP) are not usually indicated but evidence is lacking to guide management in this situation.]
Treatment of premature rupture of membrane (PROM):
Specific treatment for PROM will be determined by your doctor based on:
➤ pregnancy, overall health, and medical history
➤ Extent of the condition. latest gu boat
➤ tolerance for specific medications, procedures, or therapies. VIZUR
➤ Expectations for the course of the condition.
Treatment for premature rupture of membranes may include:
➤ Hospitalization
➤ Expectant management (in very few cases of PPROM, the membranes may seal over and the fluid may stop leaking without treatment, although this is uncommon unless PROM was from a procedure, such as amniocentesis, early in gestation).
➤ Monitoring for signs of infection, such as fever, pain, increased fetal heart rate, and/or laboratory tests.
➤ Giving the mother medications called corticosteroids that may help mature the lungs of the fetus (lung immaturity is a major problem of premature babies). However, corticosteroids may mask an infection in the uterus.
➤ Antibiotics (to prevent or treat infections).
➤ Tocolytics. Medications used to stop preterm labor.
➤ Women with PPROM usually deliver at 34 weeks if stable. If there are signs of abruption, chorioamnionitis, or fetal compromise, then early delivery would be necessary.)
Management of premature rupture of membrane (PROM):
1. Early diagnosis of signs and symptoms.
2. Assessment of followings:
➤ Gestational age.
➤ Whether the patient is in labor or not.
➤ Any evidence of sepsis.
➤ Degree of oligohydramnios.
➤Sonographic myometrial thickness.
➤ Number of fetuses.
➤ Pregnancy complications.
3. Aseptic vaginal examination with a sterile speculum is done, not only to confirm the diagnosis but also to note the state of cervix and to detect any cord prolapsed.
4. Vaginal-digital examination is generally avoided.
5. Patient is put to bed rest and sterile vulval pad is applied to observed any further leakage.
6. Maternal pulse, temperature and FHR are monitored 4 hourly.
7. If pregnancy is <34 weeks:
➤ Corticosteroids given to the mother of a baby at risk of being born prematurely can speed up fetal lung development and reduce the risk of death of the infant, RDS, IVH, and Necrotizing enterocolitis.
➤ The younger the fetus, the longer it takes for labor to start on its own, but most women will deliver within a week.
➤ Watch carefully for infection, placental abruption, umbilical cord compression, or any other fetal emergency that would require quick delivery by induction of labor.
8. Prophylactic antibiotics are given to minimise maternal and perinatal risk of infection. Intravenous ampicillin, amoxycillin or erythromycin for 48 hours followed by oral therapy for 5 days or until delivery is recommended.
Or (Another answer)
Management of premature rupture of membrane (PROM):
1. Refer urgently to hospital if:
a. P-PROM is suspected.
b. Ascending infection is suspected: maternal or fetal tachycardia, temperature, abdominal tenderness.
2. Women are usually seen in hospital and admitted for the first 48 hours. After this time, management at home which includes taking 4- to 8-hourly temperatures may be possible for some women.
3. Antibiotic administration:
a. Prophylactic antibiotics for P-PROM appear to reduce complications due to preterm delivery and postnatal infection. However, there is no evidence of long- term safety from this strategy and benefits in a high-income healthcare setting may be small.
b. Use of erythromycin 250 mg qds for 10 days (or until labour is established if this is sooner) following the diagnosis of P-PROM (unlicensed use).
c. If Group B streptococcus is isolated from a swab or if erythromycin is contra- indicated then penicillin or clindamycin is usually recommended.
d. Co-amoxiclav should not be used for prophylaxis in P-PROM.
4. Tocolytics eg, atosiban, nifedipine or ritodrine are no longer recommended, as they do not significantly improve perinatal outcome.
5. Amnioinfusion is not currently recommended for routine clinical management of P- PROM.
6. Antenatal steroids should be given if gestation is between 24 and 34 weeks. Antenatal steroids are associated with a significant reduction in rates of neonatal death, respiratory distress syndrome and intraventricular haemorrhage and are safe for the mother.
Delivery or expectant management:
1. There is currently insufficient evidence to guide clinical practice on the benefits and harms of immediate delivery compared with expectant management for women with P- PROM.
2. Delivery should usually be considered at 34 weeks.
3. If the pregnancy continues over 36 weeks then the mother should be informed that she has an increased risk of chorioamnionitis and a reduced risk of respiratory problems for the neonate.
4. It is recommended that women with PROM at term should not exceed 96 hours following membrane rupture. The risk of maternal and fetal infection increases with longer time between the rupture of membranes and the onset of labour.
Complication of premature rupture of membrane (PROM):
A. Maternal complications:
➤ Early Delivery
➤ Infection
➤ Placental abruption
➤ Retained placenta
➤ Umbilical prolapse
➤ Respiratory distress syndrome
➤ Postpartum hemorrhage (PPH)
➤ Endometritis
B. Neonatal complications
➤ Prematuirity
➤ Pneumonia and early neonatal sepsis
➤ Pulmonary hypoplasia
➤ Fetal death

Prevention of premature rupture of membrane (PROM):
Unfortunately, there is no way to actively prevent PROM. However, this condition does have a strong link with cigarette smoking and mothers should stop smoking as soon as possible
➤ Women who have previously had a preterm birth or pregnancy loss between 16 and 34 weeks, should be offered either intravaginal progesterone or cervical cerclage.
➤ Women with no history of a preterm birth or pregnancy loss between 16 and 34 weeks, should be offered intravaginal progesterone.
➤ Women who have had P-PROM in a previous pregnancy or have a history of cervical trauma, should be offered cervical cerclage,
1. Spontaneous rupture of membrane (SROM): SROM refers to the naturally-occurring rupture of the fetal membranes during or after the onset of labor. This is a perfectly normal part of pregnancy and requires no additional intervention.
2. Artificial rupture of membrane (AROM): In certain cases, an obstetrician may deem it necessary to induce artificial rupture of the fetal membrane (AROM). AROM is typically induced when any further prolonging of pregnancy can put the baby at risk.
3. Premature rupture of membrane (PROM): PROM is a common complication of
pregnancy in which the amniotic sac breaks prior to the onset of labor but at or after 37
weeks of gestation. The causes of premature rupture of membrane vary, though the condition
occurs in 8-10% of pregnancies.
4. Preterm premature rupture of membrane (PROM): PROM refers to any incidence of
PROM that occurs prior to 37 weeks. It is a more serious condition which requires immediate
intervention to prevent consequences ranging from infection to perinatal death.
