Preterm Labour – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Preterm Labour
Nursing care for high risk pregnancy
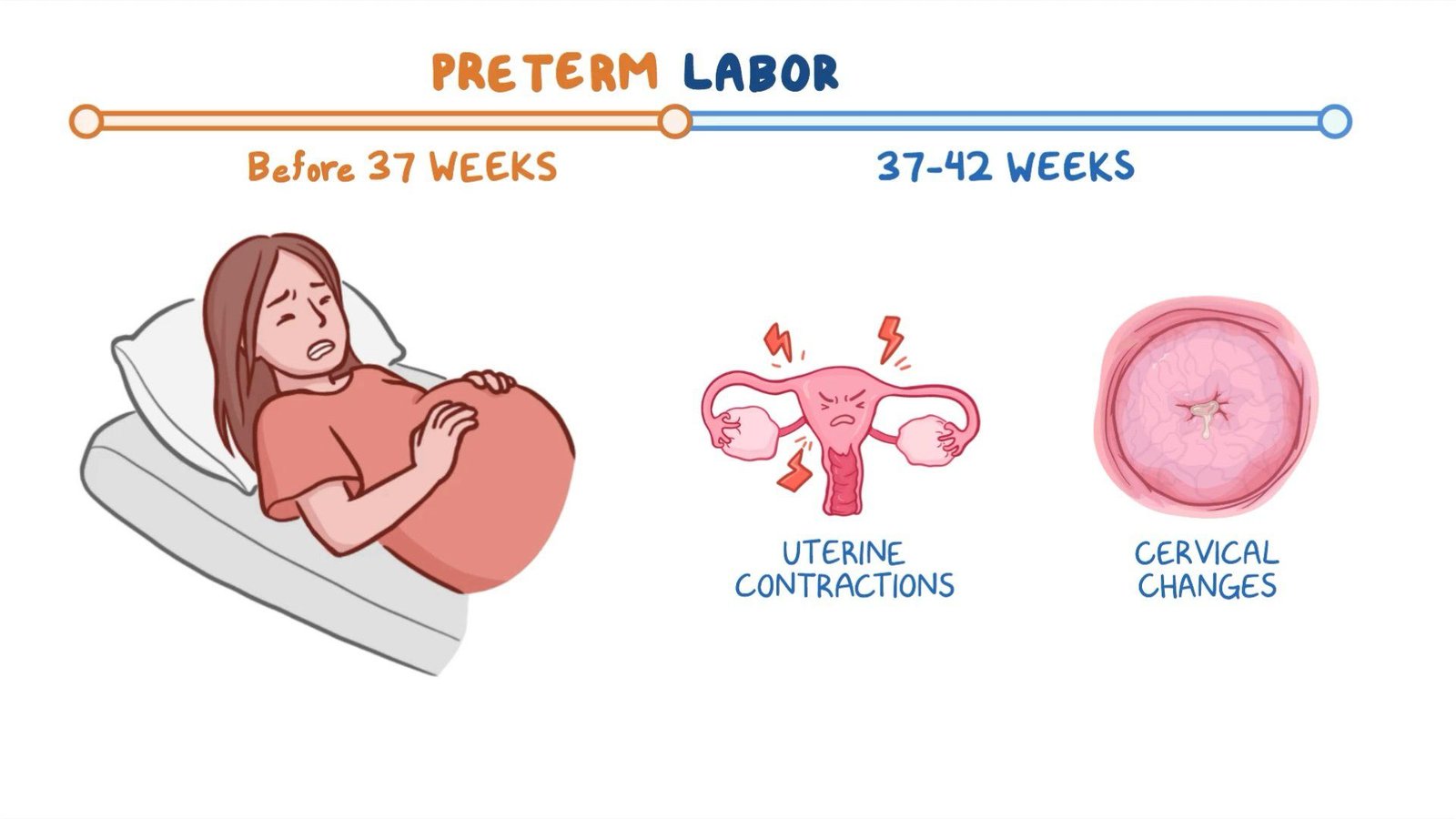
Preterm Labour:
Preterm labor is defined as regular contractions of the uterus resulting in changes in the cervix that start before 37 weeks of pregnancy. Changes in the cervix include effacement (the cervix thins out) and dilation (the cervix opens so that the fetus can enter the birthcanal).
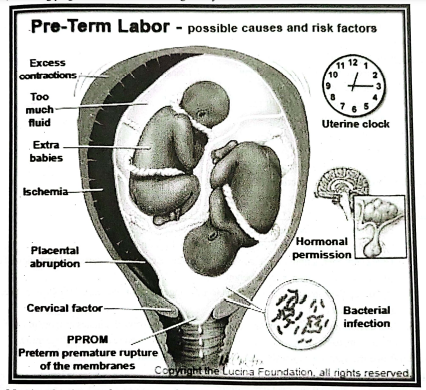
Causes of preterm labor:
➤ Premature rupture of membranes.
➤ Preterm labor (no known cause).
➤ Anaemia
➤ Multiple gestation.
➤ Medical complications such as DM, HTM.
➤ Uterine anomaly.
➤ Hydramnios
➤ UTI
➤ Gonorrhoea
➤ vaginosis
➤ Bleeding during pregnancy (antepartum hemorrhage).
➤ Hypertensive disorders of pregnancy.
➤Weak cervix (incompetent cervix),
➤ Poor education.
Risk factors of preterm labor:
➤ Smoking
➤ Being very overweight or underweight before pregnancy.
➤ Not getting good prenatal care.
➤ Previous preterm labor or premature birth.
➤ Pregnancy with twins, triplets or other multiples.
➤ Drinking alcohol or using street drugs during pregnancy.
➤ Having health conditions, such as high blood pressure, preeclampsia, diabetes, blood clotting disorders, or infections.
➤ Stressful life events, such as the death of a loved one.
➤ Red blood cell deficiency (anemia), particularly during early pregnancy.
➤ Too much amniotic fluid (polyhydramnios).
➤ Pregnancy complications, such as preeclampsia.
➤ Vaginal bleeding during pregnancy.
➤ Presence of a fetal birth defect.
➤ Being pregnant with a baby from in vitro fertilization.
➤ Being pregnant with twins or other multiples.
➤ A family or personal history of premature labor.
➤ Getting pregnant too soon after having a baby.
Clinical features of preterm labor:
➤ Regular or frequent contractions a tightening sensation in the abdomen.
➤ Backache
➤ Contractions every 10 minutes or more often.
➤ Cramping lower alsdomen or menstrual-like cramps. These can feel like gas pains that may come with diarrhea.
➤ Urinary frequency.
➤ Pelvic pressure.
➤ Fluid leaking from vagina.
➤ Flu-like symptoms such as nausea, vomiting, or diarrhea.
➤ Increased pressure in pelvis or vagina.
➤ Increased vaginal discharge.
➤ Vaginal bleeding, including light bleeding.
Diagnostic criteria of preterm labor:
➤ Uterine contraction 4 times/20 minutes or 8 times/60 minutes.
➤ Cervical dilatation > 1 cm.
➤ Cervical effacement 80% or more.
➤ Laboratory tests:
✔ CBC
✔ Urine analysis
✔ vaginal fluid culture
Checking for contractions is a key way of spotting early labor:
1. Place fingertips on the abdomen.
2. If feel uterus tightening and softening, that’s a contraction occur.
3. Time every contractions. Write down the time when a contraction starts, and write down the time at the start of the next contraction.
4. Try to stop the contractions. Get off the feet. Change position and relax. Drink two or three glasses of water.
5. Call doctor or midwife if continue to have contractions every 10 minutes or more often, if any of symptoms get worse, or if women have pain that’s severe and doesn’t go away.
Laboratory tests needed for preterm labour:
Laboratory tests
In patients with a history of midtrimester loss, laboratory tests for risk assessment include the following:
➤ Rapid plasma reagin test
➤ Gonorrheal and chlamydial screening
➤ Vaginal pH/wet smeat/whiff test
➤ Anticardiolipin antibody (eg, anticardiolipin immunoglobulin [Ig] G and IgM, anti-beta2 microglobulin)
➤ Lupus anticoagulant antibody
➤ Activated partial thromboplastin time
➤ One-hour glucose challenge test.
Manage a case of premature labor with a premature baby:
1. Care of mother:
If doctor or midwife thinks pregnant womens are going into premature labor, they probably need to go to the hospital. Midwife, or nurse will:
➤ Ask about medical history, including medicines that have been taking during pregnancy.
➤ Check pulse, blood pressure, and temperature.
➤ Put a monitor on belly to check baby’s heart rate and contractions.
➤ Swab for fetal fibronectin, which helps predict the risk of delivering early.
➤ Check cervix to see if it is opening.
➤ Assess fetal wellbeing.
If you are diagnosed with premature labor, pregnant women may need treatment, which may include:
➤ Hydration is used to decrease the frequency of uterine contraction.
➤ Tocolytic is the use of medications to stop labor.
➤ Avoid delivery prior to 34 weeks
✓ Bed rest
✓ IV fluids
✓ Hydration and position changes
✓ Treatment of UTI and other infection if present
✓ Medicine to relax uterus and stop labor
✓ Medicine to speed up the development of baby’s lungs
✓ Antibiotics
✓ Being admitted to the hospital
Pharmacological agents:
Medicines used according to doctors order that are helpful for managing preterm labour includes:
➤ Magnesium sulfate (MgSO4): Widely used as the primary tocolytic agent because it has similar efficacy to terbutaline (one of the previous agents of choice), with far better tolerance.
➤Indomethacin: An appropriate first-line tocolytic for early preterm labor (< 30 wk) or preterm labor associated with polyhydramnios.
➤Nifedipine: Despite its unlabeled status, several randomized studies have found nifedipine to be associated with a more frequent successful prolongation of pregnancy than other tocolytics.
➤ Glucocorticoids to accelerate fetal lung matuirity.
Health education:
➤ Rest 2 to 3 times a day lying on the left side
➤ Drink 2-3 litres water each day. Avoid smoking/caffeine.
➤ Avoid lifting objectives.
➤ Empty bladder at least 2 hours during waking hours.
➤ Avoid prenatal preparation of the breastsames
➤ Take prescribed tocolytic medication on time to maintain a constant blood level.
➤ Eliminate or decrease sexual activity.
➤ Monitor FHR and uterine contraction daily.
➤ Report signs of UTI
➤ Report signs of PROM or vaginal bleedingan
2. Care of baby:
A. Immediate management:
1. Cord to be clamped quickly to prevent hypervolaemia and development of hyperbilirubinemia.
2. Cord length to be 10-12 cm for use if exchange transfusion is required.
3. Air passage to be cleared of mucus promptly.
4. Adequate oxygenation to be provided (not exceeding 35%).
5. The baby should be wrapped including head in a sterile warn towel to prevent hypothermia and its sequelae such as hypoxia, hypoglycemia and metabolic acidosis.
6. Injection of vitamin K to be given to prevent haemmorhagic problems.
B. Intensive care:
1. Monitor body temperature at regular intervals to prevent hypothermia and hyperthermia. The temperature should be maintained between 35.5° to 37.2°C or (96- 99° F).
2. Smaller babies are to be nursed in incubator where temperature and humidity can be regulated.
3. Oxygen to be administered to tide over maintain desirable level of saturation.
4. Prophylactic antibiotic therapy. the initial cyanotic phase and later to
5. Nutrition: Gavage feeding of parenteral nutrition depending on age and vigour of the baby
C. Nursing care:
1. Temperature twice daily or according to institutional policy.
2. Weight every day to know if the newborn is over hydrated or under hydrated
3. Continuous observation and monitoring in the first 48 hours
4. Visitation of mother.
5. Providing manually expressed breast milk to haby until able to suck and swallow.
D. Observation for signs of progress such as
1. Colour pink all the time.
2. Smooth and regular breathing.
3. Increasing vigour exhibited by limb movements and cry.
4. Progressive gain in weight after the first week.
5. Teach mother about the feeding to be continued, vitamin supplements, immunization and check-up.
[Ref-Annamma Jacob/2/451-452]
Prevention of preterm labor:
➤ Seek regular prenatal care.
➤ Quit smoking
➤ Avoid drinking alcohol and using recreational drugs.
➤ Maintain an adequate amount of weight gain throughout pregnancy.
➤ Eat a nutritious and well-balanced diet. Nutrition and optimal prenatal care are especially important.
➤ Avoid heavy lifting and work, and standing for long periods of time.
➤ Minimize the stress in life whenever possible, and deal with stress using relaxation techniques, exercise, nutrition, and rest.
➤ Go to prenatal classes.
➤ Avoid infections as much as possible.
➤ Some chronic maternal illnesses can lead to premature birth if they are not treated properly during pregnancy. They need to be appropriately managed during pregnancy,
➤ Eat a healthy diet.
➤ Avoid risky substances
➤ Consider pregnancy spacing.
➤ Be cautious when using assisted reproductive, technology (ART)d alt otsail
➤ Taking preventive medications,
➤ Limiting certain physical activities.
➤ Managing chronic conditions
Complications of preterm labor:
➤ Immature Lungs
Immature lungs are associated with the following complications:
✓ Respiratory Distress Syndrome (RDS),
✓ Transient tachypnea.
✓ Bronchopulmonary Dysplasia (BPD).
✓ Pneumonia
✓ Meningitis.
✓ Apnea and Bradycardia.
➤ Infection
➤ Jaundice
➤ Intraventricular hemorrhage (IVH).
➤ Cerebral palsy.
➤ Mental retardation.
➤Intracranial hemorrhage occurs in about 1/3 of babies born at 24-26 weeks gestation.
➤ Inability to maintain body heat.
➤ Immature gastrointestinal and digestive system.
➤ Anemia
➤ Patent Ductus Arteriosus (PDA).
➤ Retinopathy of Prematurity (ROP).
➤ Necrotizing Enterocolitis (NEC).
➤ Sepsis
Different terms related to preterm labour:
➤ Late preterm, born between 34 and 36 weeks of pregnancy.
➤ Moderately preterm, born between 32 and 34 weeks of pregnancy.
➤ Very preterm, born at less than 32 weeks of pregnancy.
➤ Extremely preterm, born at or before 25 weeks of pregnancy,
➤ Most premature births occur in the late preterm stage.