Protein Energy Malnutrition – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Protein Energy Malnutrition

Definition of Protein Energy Malnutrition (PEM):
Protein Energy Malnutrition describes as a range of clinico-pathological condition arising from co-incidental lack, in varying proportion of protein and calories, occurring mostly in infant and young children, and commonly associated with infection. (WHO – 1973)
Or
Protein energy malnutrition or PEM to mean the kind of malnutrition which results from insufficient intake of energy, protein and other nutrients.
Or
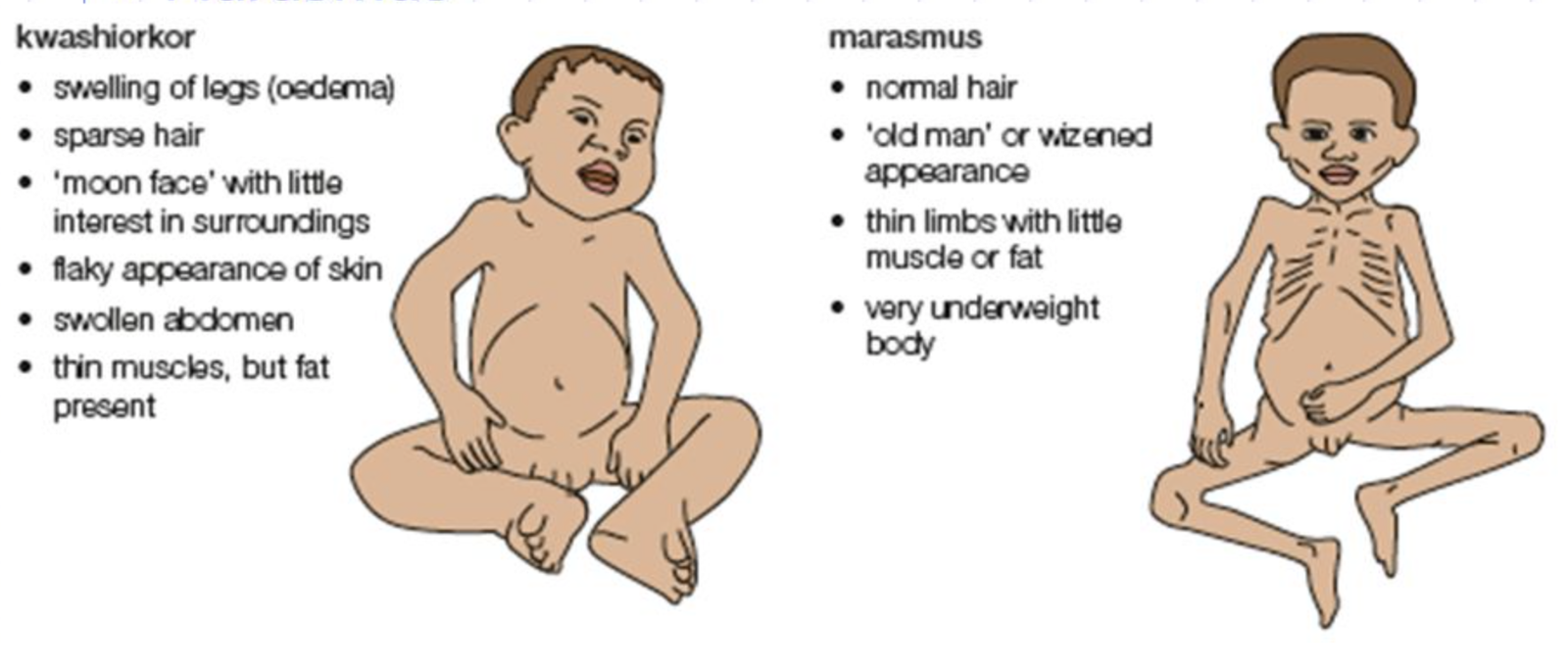
Protein-energy malnutrition (PEM) in early childhood is a spectrum of disease. At one end there is kwashiorkor, at the other end is nutritional marasmus and in the middle of the spectrum is marasmic kwashiorkor.
(Ref: K. Park/24h/679)
Risk factors for PEM:
1. An inadequate intake of food (food gap) both in quantity and quality.
2. Infection: Diarrhoea, Respiratory infections, Measles, intestinal worm.
3. Poor environmental conditions.
4. Large family size.
5. Poor maternal health.
6. Failure of lactation.
7. Premature termination of breast feeding.
8. Adverse cultural practices relating to child rearing and wearing, such as
- The use of over-diluted cow’s milk,
- Discarding cooking water from cereals,
- Delayed supplementary feeding.
(Ref by: K. Park/24th/640)
PEM Classification According to WHO/FAO:
| Types | Body weight % of international standard | Oedema | Deficit in weight for height |
| Kwashiorkor | 80-60 | Present | |
| Marasmic kwashiorkor | <60 | Present | |
| Marasmus | <60 | Absent | |
| Nutritional dwarfism | <60 | Absent | Minimal |
| Underweight child | 80-60 | Absent |
Another Answer
Classification of PEM:
A. Gomez classification:
| Weight for age (%) | Grade of PEM |
| 90-100 | Normal |
| 75-89 | Grade I, (mild malnutrition) |
| 60-74 | Grade II, (Moderate malnutrition) |
| Less than 60 | Grade III (Severe malnutrition) |
B. Welcomes classification:
| Weight for age | With edema | Without edema |
| 60-80% | Kwashiorkor | Under nutrition |
| Less than 60% | Marasmic kwashiorkor |
C. Waterlows classification:
| Stunting (height/age) | Wasting (weight/height | |
| Normal | 95 | 90 |
| Mild | 87.5-95 | 80-90 |
| Moderate | 80-87.5 | 70-80 |
| Severe | <80 | >70 |
A. Weight for age (%) = Weight of subject / Weight of a normal child of same × 100
B. Height or age (%) = Height of the subject / Height of a normal child of the same age × 100
C. Weight or height (%) = Weight of subject / Weight of a normal child of the same height x 100
(Ref by: K. Park/24th/677)

Preventive Measures of PEM (According to WHO/FAO):
| 1. Health Promotion: |
|
| 2. Specific protection: |
|
| 3.Early diagnosis & Treatment: |
|
| 4. Rehabilitation: |
|
PEM is a problem of slum people because –
1. They are the vulnerable society having poverty whose intake of food never be adequate and child’s diet doesn’t contain protein energy rich foods like milk, eggs, fresh fruits etc.
2. Infections are very common in the slum people notably diarrhea, respiratory infections, measles and intestinal worms which increase requirements for calories, proteins and other nutrients while decreasing the absorption and utilization’
3. Lack of immunization, lack knowledge about family planning and spacing of births
4. Poor environmental conditions, large family size, poor maternal health are also contributing factors.
Management of PEM:
1. Resuscitation: It includes correction of hypoglycemia, dehydration, electrolyte disturbances, acidosis, and treatment for infections.
2. Start of the cure: It includes re-feeding, gradually working up the calories to 150 kcal/kg with protein about 1.5 g/kg.
3. Nutritional rehabilitation.
For EQ
Treatment of PEM:
a. Assessment of the child:
- Dehydration: ORS/ IV fluid
- Infections: Appropriate antibiotics
- Control of hypothermia: Patient is kept warm
- Control of hypoglycemia: 25% dextrose, 4 ml/kg IV in severe cases; NG tube feeding if IV could not be given
b. Nutrition:
High protein (3.5 gm/kg/day + adequate calorie (120-140 Kcal/kg/day) + other essential nutrients. Feeding by NG tube small and frequent round the clock. Each feed contains 100 mg water + milk 70 Kcal + sugar 20 Kcal + Soybean oil 22 Kcal
c. Vitamin A: High potency (2 Lac units) on 1st, 2 ^ (nd) and 7 ^ (th) Then every 6 month up to 6 years of age
d. Iron: 2 – 4mg / k * g / d * ay
e. Blood transfusion: 10 – 15ml / k * g (PCV) if needed
f. Potassium chloride: 2-4 mmol/kg/day
g. Zinc acetate: 2 mg/kg/day
h. Fluid: In marasmus 100 – 150ml / k * g / d * ay and in kwashiorkor 80 – 100ml / k * g / d * ay
Factors Related to Malnutrition in Bangladesh:
| Women’s education | 43% |
| Health environment | 19% |
| Food availability | 26% |
| Women’s status | 12% |
Nursing Responsibilities for the Management of PEM:
- Nursing personnel can provide preventive, curative and rehabilitative services to the children with PEM at home and hospital. The nursing responsibilities include the following
- Assessment of nutritional status of the children with collection of appropriate dietary history, including history of breastfeeding, weaning, food habits, balanced diet, socioeconomie status, presence of illness etc. Physical examination and anthropometric assessment also important to detect the nutritional deficiency states.
- Assisting in diagnostic investigations whenever necessary.
- Maintenance of growth chart by regular health checkup at home, clinic or health centers for early detection of growth failure. (bab stiloe à dist
- Participating in the hospital management in complications and life threatening situations related to PEM and other related illness.
- Implementing nutritional rehabilitation activities.
- Encouraging the parents for home care and follow up at regular interval.
- Nutrition education, demonstration and counseling according to identified problems of particular child.
- Informing about breast feeding, weaning, balanced diet, food hygiene, personal hygiene (hand washing), appropriate feeding practices and food habits, cultural taboos, irrational belief, quality of common foods, foods values, food preservations etc,
- Promoting preventive measures for individual, family and community to overcome the problem of PEM.
- Co-operating with other team members and acting with different sectors for the implementation of various nutritional services.
- Maintain in implementation of national nutritional programs for prevention of various malnutrition.
Complications of PEM:cimacl
Early (Presenting) Complications of PEM:
a) Infections: ARI, Diarrhea, TB, helminthiasis, septic shock, DIC and Opportunistic Candidiasis
b) Hypothermia
c) Metabolic
- Hypoglycemia
- Hypocalcaemia
- Hypomagnesaemia
d) Fluid & electrolyte imbalance
- Dehydration
- Hypokalemia
- Hypernatremia
e) Lactose intolerance
f) Severe anemia & other nutrient deficiencies
g) Congestive cardiac failure
Late (Recovery) complications:
a) Diarrhea (lactose intolerance)
b) CCF (high protein & solute diet)
c) Unmasking of subclinical vitamin/mineral deficiencies
Long-term effects:
a) Growth retardation
b) Cognitive & learning disabilities
Read more: