Puerperal Sepsis – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Puerperal Sepsis
Puerperal sepsis
An infection of genital tract which occurs as a complication of delivery is termed puerperal sepsis.
Or
Infection in the female genital tract within 10 days of childbirth, miscarriage, or abortion. There is fever, pain in the lower abdomen and an ill-smelling vaginal discharge.
Causes of puerperal sepsis
A. Organisms:
a) Aerobic
- E. coli (most common).
- Streptococcus pyrogens (group A & B).
- Staphylococcus aureus.
- Klebsiella.
- Pseudomonas.
b) Anaerobic:
- Bacteroids (fragilis)
- Cl. Welchii.
- CL tetani.
B. Predisposing factors of puerperal sepsis
1. Antepartum factors
- Malnutrition & anaemia.
- Preterm labour.
- Pre-delivery factors: existing malnutrition, anaemia, diabetes or sexually transmitted diseases.
- Premature rupture of cervico-vaginal membrane.
- Premature rupture of membrane.
- Prolonged rupture of membrane (>18 hours).
2. Intrapartum factors-.
- Repeated vaginal examinations.
- Prolonged rupture of membranes (>18 hours).
- Dehydration &kitoacidosis during labour.
- Traumatic operative delivery.
- Haemorrhage (antepartum & postpartum)
- Retained bits of placental tissue of membranes.
- Cesarean section
Women are prone to puerperal sepsis after birth because
1. Repeated vaginal examination: Vagina is repeatedly examined during labour to determine if its stretching well. The instruments, gloves etc may introduce the bacteria thriving in the vagina to the uterus causing puerperal sepsis.
2. Infection may be passed on through foreign substances or even sexual activity.
3. Wounds at placenta site: After delivery, placenta detaches. This then becomes a raw wound and may be easily attacked by bacteria.
4. Torn vagina and cervix, damaged uterine surface all are wound sites which may contain lacerations and hence become a breeding ground for bacteria.
5. Sometimes, pieces of placenta may remain behind after childbirth which can cause puerperal sepsis. This is the leading cause for this condition.
6. Prolonged labour.
7. If dead tissue remain in the uterus or are introduced during examination, this may cause puerperal sepsis.
8. The untreated cuts or wounds in vagina which may become infected.
9. C-section increases the chances of developing puerperal sepsis. 1 in 800 C-section develops puerperal sepsis.
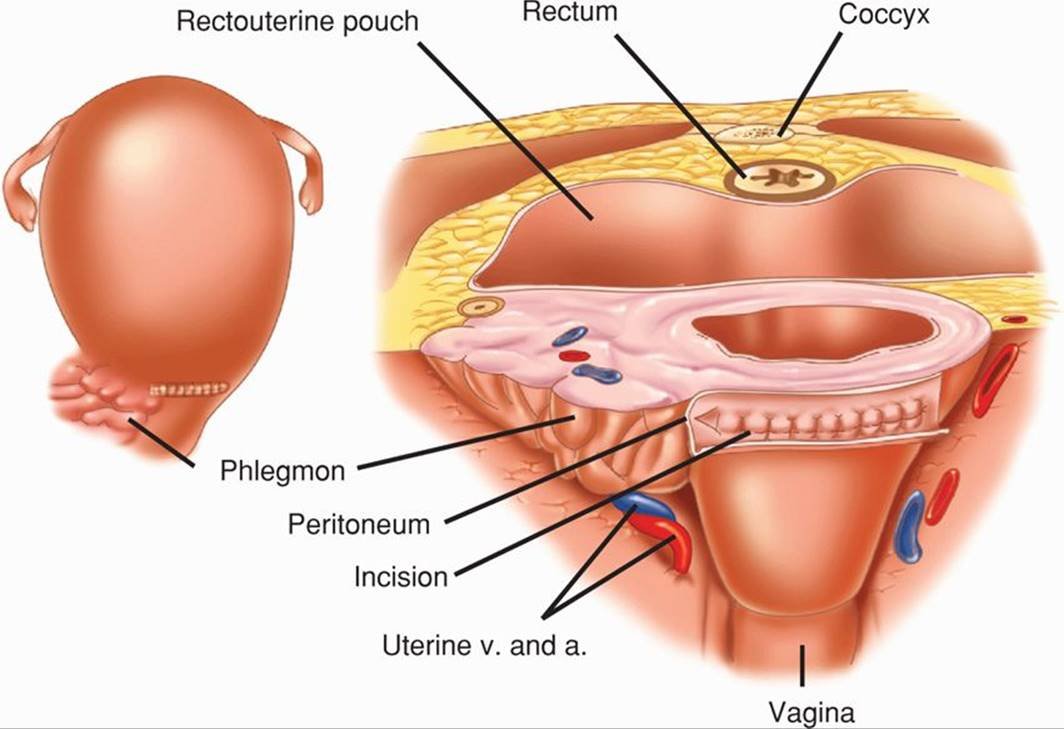
Consequences of puerperal sepsis
- Parametritis.
- Pelvic peritonitis.
- General peritonitis.
- Thrombophlebitis.
- Bacteraemia,
- Septicaemia.
- Endotoxic or septic shock.
Management of puerperal sepsis
- Fever & tachycardia.
- Local discharge becomes offensive and copius.
- Sub-involution of uterus & becomes tender.
- The local would becomes red & swollen.
Severe
- High rise of temperature with chills & rigor.
- Lochia may be scanty and odorless.
- Sub-involution, tender & softer uterus.
- Associated wound infection (Perineum, vagina, cervix).
- Pus may form which leads to disruption of the wound.
- Onset on 7th to 10th day.
- Sustained rise of temperature.
- Constant pelvic pain.
- Tenderness on either side.
- Per vaginal examination: Unilateral tender indurated mass.
- Pyrexia with increase pulse rate.
- Lower abdominal pain & tenderness.
- Pervaginal examination: Tenderness on the fornix & movement of the cervix.
- High rise of temperature & vomiting.
- Generalized abdominal pain.
- Tender & distended abdomen rebound tenderness of ten.
- High rise of temperature with tachycardia.
- Blood culture is positive.
Investigations
A case of puerperal pyrexia is considered to be due to genital sepsis unless proved otherwise:
- High vaginal &endocervical swabs for culture in aerobic & anaerobic media and sensitivity test to antibiotics.
R/M/E of urine & culture sensitivity test (clean catch midstream specimen). - Blood for TC, DC, Hb%.
- Thick peripheral blood film (for malaria)
- Blood culture (if fever with chills & rigor).
- Others-
✓ Pelvic ultrasound (to defect any retained bits of placenta or abscess).
✓ CT & MRL
✓ Blood urea & electrolytes.
Treatment
General care:
- Adequate fluid & caloric
- Anaemia is corrected by oral iron-tab ferrous-sulfate 200 (pg) 2 times daily for 3 months
- Pain is relieved by adequate analgesics.
- An indwelling catheter is used.
- A chart is maintained by recording pulse, respiration, temperature, lochial discharge and fluid intake, & output.
Specific management:
Antibiotic: Cap cephradine 500 mg, 4 times daily for 7 days (or 14 days if UTI).
Tab, metronidazole, 400 mg, 3 times daily for 7 days, or /v.
Tab, paracetamol (500 mg), 3 times daily until fever subside.
Tab calcium (200 mg), 1 times daily for 3 months.
Surgical treatment
- Perineal wound:
✓ Removal of stitches & drainage of pus.
✓ The wound is to be dressed with hot compression & antiseptic solution.
- Retained uterine products: Exploration of uterine cavity.
- Pelvic abscess: Colpotomy under ultrasound guidance.
- Laparotomy may be needed.
- Hysterectomy may be indicated.
Before childbirth
1. Maintain a healthy haemoglobin level, preferably above 11gm.
2. Get hold of vitamin and protein supplements, after discussing with the obstetrician.
3. Get immediate medical care for any wounds or even seasonal diseases.
4. Ensure balanced diet-consult doctor and discuss any conditions.
5. Have plenty of fluid intake.
6. Avoid sexual intercourse during last 2 months of pregnancy.
7. Avoid appearances in crowded and unhygienic places, this will prevent you from catching respiratory diseases.
8. If you have any condition, such as flu or asthma get reated timely.
9. Keep body resistance high-by eating well and treating all ailments.
After childbirth
1. Maintain proper hygiene especially around perineum: Clean perineal area after using toilet. Wipe it gently using antibacterial solution or wipes.
2. Keep the area dry, ventilated and clean.
3. Monitor vital parameters such as pulse and body temperature.
4. The environment should be free of dust, by frequent mopping and restricting visitors.
5. During periods, use soft sanitary napkins. Change it frequently and maintain hygiene.

4 important urinary complications of puerperium:
- UTI
- Retention of urine.
- Incontinence of urine.
- Suppression of urine.
4 Important organisms for UTI:
- E. coli
- Klebsiella
- Proteus
- Staphylococcus aureus