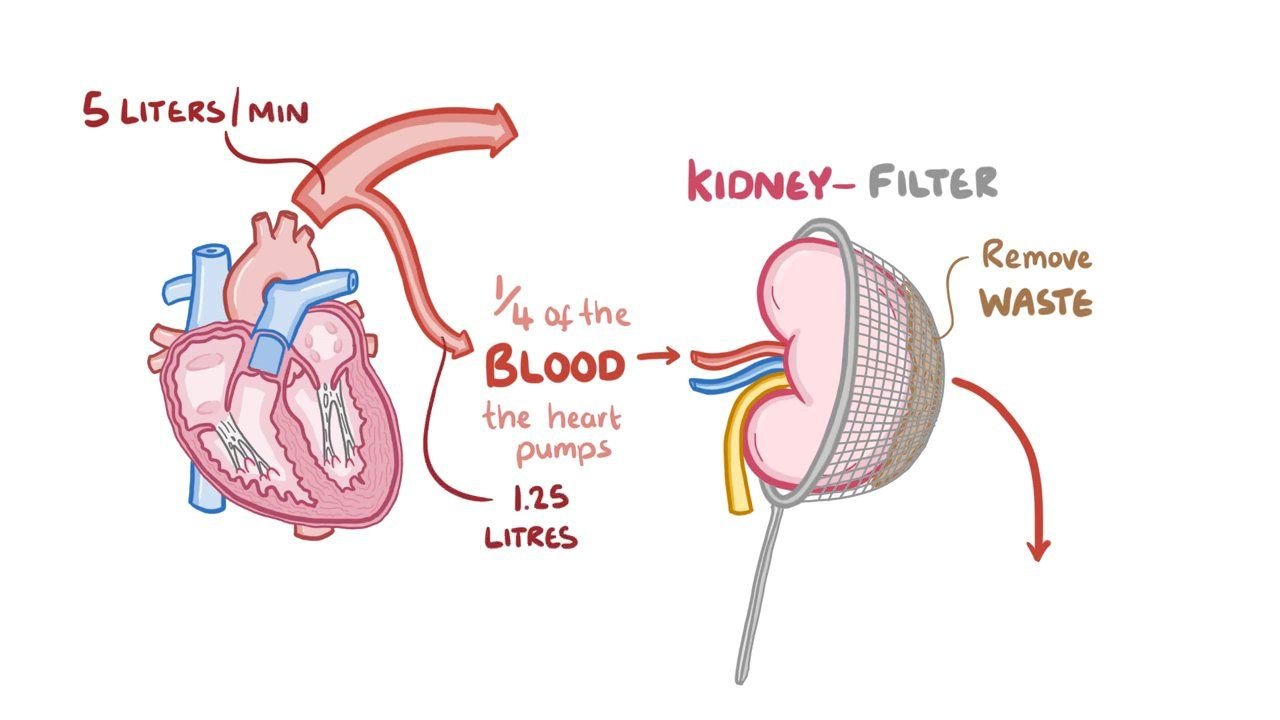
Today our topic of discussion is ” Regulation of Renal Blood Flow “. The kidneys are remarkable organs that play a vital role in maintaining homeostasis within the human body. Among their many functions, they are responsible for filtering blood, removing waste, balancing electrolytes, and regulating blood pressure.
To accomplish these tasks, the kidneys must receive a significant and steady supply of blood. Renal blood flow (RBF) is the volume of blood delivered to the kidneys per unit of time and is a crucial parameter for kidney function. This article explores the complex mechanisms by which renal blood flow is regulated, ensuring that the kidneys can perform their vital functions efficiently.
Regulation of Renal Blood Flow : The Urinary System
Anatomy and Function of Renal Blood Flow:
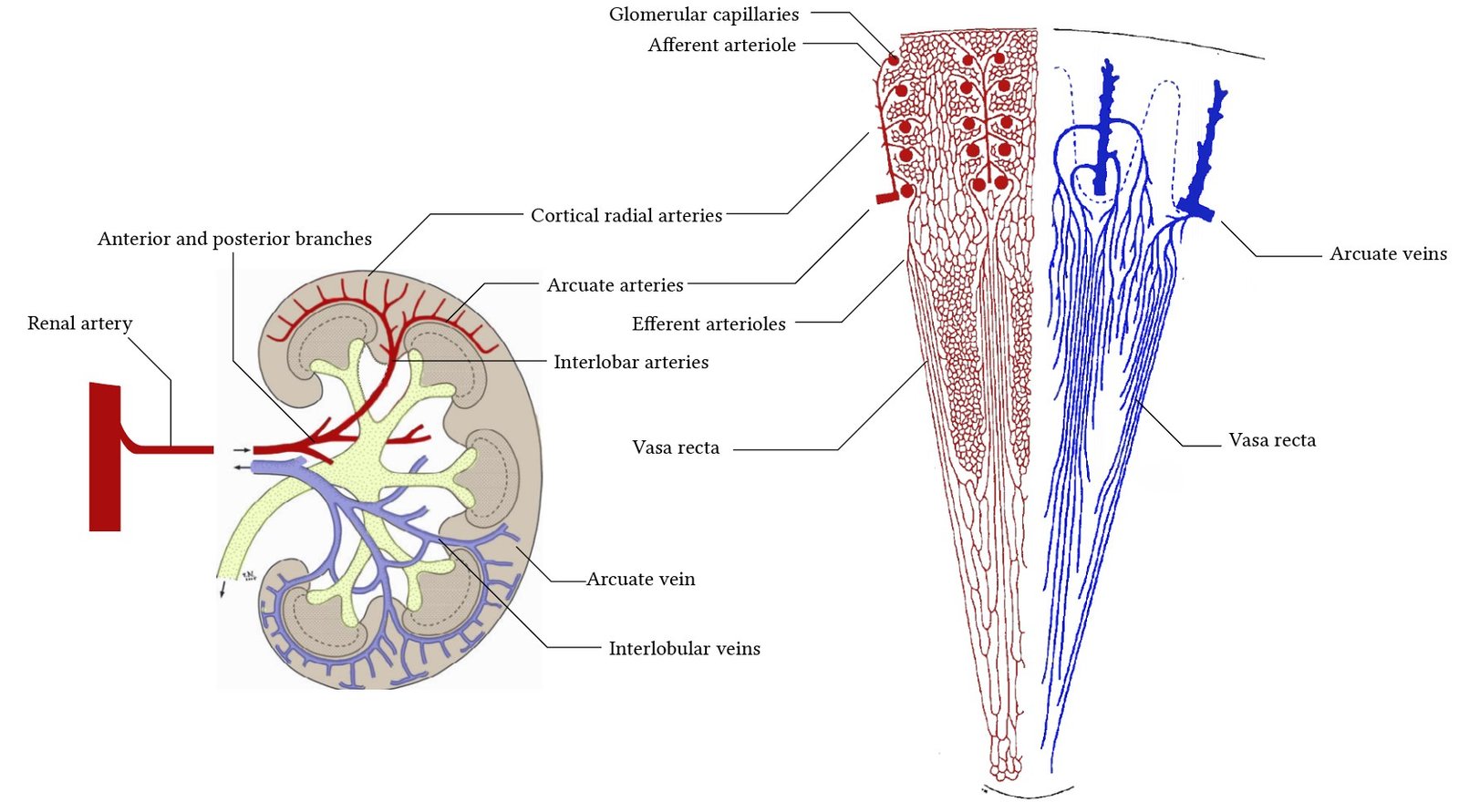
The kidneys are supplied with blood by the renal arteries, which branch from the abdominal aorta. Upon entering the kidney, the renal artery divides into smaller and smaller vessels, eventually forming afferent arterioles that lead to the glomeruli, where filtration of blood takes place. Blood exits the glomeruli through efferent arterioles, which then form a secondary capillary network around the tubules for further exchange of substances.
The unique arrangement of two capillary beds in series, glomerular and peritubular, is crucial for the kidneys’ ability to filter and modify the plasma. RBF must be tightly regulated to ensure efficient filtration without causing damage to the delicate renal structures.
Regulatory Mechanisms:
Regulation of RBF is complex and involves multiple factors that respond to systemic and local cues. These factors include:
- Neural Regulation: a. Sympathetic Nervous System (SNS): The SNS has a profound effect on RBF. Activation of the SNS causes vasoconstriction of the renal arterioles, thereby decreasing RBF. This response is particularly important during stress or hemorrhage when blood flow needs to be redistributed to vital organs.
- Hormonal Regulation: a. Renin-Angiotensin-Aldosterone System (RAAS): This hormonal cascade is crucial for blood pressure and fluid balance regulation. When RBF is low, the kidneys release renin, which converts angiotensinogen to angiotensin I, which is further converted to angiotensin II. Angiotensin II causes vasoconstriction and increases blood pressure, thus increasing RBF. b. Atrial Natriuretic Peptide (ANP): ANP is released from the heart when blood volume is high and causes vasodilation of the renal blood vessels, increasing RBF and promoting diuresis to decrease blood volume. c. Antidiuretic Hormone (ADH): Also known as vasopressin, ADH can affect RBF by causing vasoconstriction. However, its primary effect is on water reabsorption in the collecting ducts.
- Autoregulation: a. Myogenic Mechanism: Vascular smooth muscle reacts to changes in pressure. If arterial pressure increases, the afferent arteriole’s smooth muscle contracts to prevent an increase in RBF and glomerular filtration rate (GFR). b. Tubuloglomerular Feedback: This involves the macula densa, cells in the distal tubule that detect chloride ion concentration. If RBF is high, chloride ion concentration will be high, and the macula densa signals for arteriolar constriction, reducing RBF to normal levels.
- Local Factors: a. Nitric Oxide (NO): NO is a potent vasodilator produced by endothelial cells. It plays a role in maintaining low resistance in renal vasculature, promoting increased RBF. b. Prostaglandins: These local hormones are vasodilators and are produced within the kidney. They counteract the effects of SNS and RAAS, especially during times of stress to prevent excessive vasoconstriction.
- Metabolic Control: The kidneys consume a significant amount of oxygen for sodium transport. As such, an increase in renal metabolic activity can lead to vasodilation and increased RBF to meet the oxygen demand.

Pathophysiology of Renal Blood Flow Dysregulation:
Disruption in the regulation of RBF can lead to pathological conditions. Renal artery stenosis, for instance, can impair RBF by narrowing the vessels, leading to hypertension and ischemic renal disease. Additionally, conditions like diabetes mellitus can lead to diabetic nephropathy, where the intricate balance of RBF regulation is disrupted, contributing to kidney damage over time.
Clinical Implications and Monitoring:
Monitoring RBF is crucial in various clinical settings, such as during major surgery or in the management of critically ill patients. Clinical interventions often aim to preserve RBF to prevent acute kidney injury (AKI). The use of fluids, medications, and sometimes invasive monitoring techniques are employed to maintain adequate RBF in these situations.
Conclusion:
The precise regulation of RBF is central to the homeostatic functions of the urinary system. It involves an intricate interplay between neural, hormonal, and local factors that ensure the kidneys filter blood efficiently while protecting their structure and function. Understanding the dynamics of RBF regulation not only provides insights into kidney physiology but also has significant implications for the diagnosis and management of renal pathologies.
The article has covered an overview of the mechanisms involved in the regulation of renal blood flow and touched upon its pathophysiological aspects. It also underscored the clinical significance of RBF regulation and monitoring in various healthcare scenarios. A deeper understanding of these regulatory mechanisms is crucial for developing advanced therapeutic interventions to manage kidney diseases and conditions that compromise renal hemodynamics.
Read more: